Abstract
Due to the multifactorial and multisystemic nature of diabetes mellitus, it is often treated with a combination of therapeutic agents having different mode of action. Earlier, we have synthesized several organozinc complexes and evaluated their safety and antidiabetic properties in experimental type 2 diabetes mellitus (T2DM). More recently, we have synthesized a metformin-3-hydroxyflavone complex and studied its antidiabetic efficacy in experimental rats. In the present study, a new zinc-mixed ligand (metformin-3-hydroxyflavone) was synthesized, characterized by spectral studies and its antidiabetic properties was evaluated in HFD fed—low dose streptozotocin induced T2DM in rats. The hypoglycemic efficacy of the complex was evaluated through oral glucose tolerance test, homeostasis model assessment of insulin resistance, quantitative insulin sensitivity check index and by determining the status of important biochemical parameters. Oral administration of the complex at a concentration of 10 mg/kg body weight/rat/day for 30 days significantly improved the glucose homeostasis. The complex possesses significant antidiabetic properties relatively at a less concentration than metformin-3-hydroxyflavone complex in ameliorating hyperglycemia.
Diabetes mellitus is a multisystemic endocrine disorder known to interfere with the regulation of major metabolic pathways irrespective of its etiology with the common pathology of chronic hyperglycemia. Diabetes and its secondary complications are clinically treated with several drugs having the different mechanism of actions, such as biguanides, sulphonylureas, meglitinides, thiazolidines, α-glucosidase inhibitors, bile acid sequestrants, SGLT-2 (sodium/glucose cotransporter 2) inhibitors, GLP-1 (glucagon-like peptide-1) receptor agonists and insulin, either as monotherapy or combinatorial strategy. However, the maintenance of normoglycemia remains a major task in the treatment of patients with type 2 diabetes mellitus (T2DM) [1]. Accordingly, instead of a one-size-fit all approach, personalization is necessary, balancing the benefit of glycemic control with its potential risk factors taking into consideration of various etiological factors such as the patient's age, blood pressure control, lipid management, comorbidities that are frequently encountered in diabetic patients.
The ecologically derived plant secondary metabolites are known to play a pivotal role in alleviating the primary and secondary complications of dreadful human diseases such as cancer, diabetes, and atherosclerosis [2]. Among the various phytoingredients, flavonoids are known for their wide range of pharmacological as well as beneficial effects in the maintenance of human health care especially in quenching oxidative stress, a contributory factor for the progression of several secondary complications [3].
Metformin remains the optimum drug for the treatment of T2DM due to its proven safety record, weight neutrality and possible benefits on cardiovascular outcomes in addition to its low cost. Although metformin is efficacious in lowering the blood glucose levels, many patients with T2DM are not adequately controlled when metformin is prescribed as a monotherapy [4]. In the 21st century, a new class of metallopharmaceutical compounds containing zinc ions is expected to treat both the types of diabetes mellitus by making use of its unique pharmacological properties [5]. Ever since in 1980, Coulston and Dandona [6] reported the insulin mimetic activity of zinc ions, several researchers develop zinc complexes with various coordination modes around zinc (II) ion and evaluated its glucose normalizing effect. In the recent past, we have synthesized several new zinc complexes [78910] and evaluated for their toxicity as well as pharmacological properties in high fat diet (HFD) fed-low dose streptozotocin (STZ) induced experimental T2DM in rats. More recently, we have synthesized a metformin-3-hydroxyflavone complex and evaluated its antidiabetic efficacy [1112]. In the light of knowledge and expertise gained, in the present study an attempt has been made to synthesize a new metformin-zinc-flavonol complex and biochemically evaluated its toxicity as well as antidiabetic properties.
The synthesis of zinc complex involves two steps namely the synthesis of metformin-3-hydroxyflavone (Schiff base complex) and the synthesis of zinc-Schiff base complex [13]. The formation of zinc-Schiff base complex was confirmed by fourier transform infrared spectroscopy (FTIR), Mass, 1H nuclear magnetic resonance (NMR), and 13C NMR spectral studies.
Male Albino rats of Wistar strain weighing around 160 to 180 g were purchased from the Tamilnadu Veterinary and Animal Sciences University, Chennai and were housed under standard animal husbandry conditions. The rats were acclimatized for 2 weeks before initiating the experiments. Animal experiments were performed according to ethical norms approved by the Ministry of Social Justices and Empowerment, Government of India and Institutional Animal Ethics Committee guidelines (IAEC NO:03/10/12). Maximum efforts were taken to minimize the sufferings of the animals during the entire course of the study and no mortality was observed during the experimental period.
The experimental rats were designated into two dietary regimens either by feeding normal pellet diet (NPD) or HFD for 2 weeks. After 2 weeks of dietary manipulation, group 2 to 5 rats were injected with a single dose of STZ (35 mg/kg body weight/rat) in ice cold citrate buffer (pH 4.5, 0.1 mol/L) intraperitoneally. However, the control group of rats were fed with NPD and injected intraperitoneally with the same volume of citrate buffer [14]. Rats having the fasting blood glucose levels ≥250 mg/dL on the 3rd day after STZ injection were considered as diabetic and subjected to further studies.
The rats were divided into five groups and each comprising of six animals: Group 1: control rats; Group 2: HFD fed-STZ induced experimental diabetic rats; Group 3: HFD-STZ induced diabetic rats orally treated with metformin-3-hydroxyflavone complex (20 mg/kg body weight/rat) for 30 days; Group 4: HFD-STZ induced diabetic rats orally treated with zinc-metformin-3-hydroxyflavone complex (10 mg/kg body weight/rat) for 30 days; and Group 5: HFD-STZ induced diabetic rats orally treated with metformin (50 mg/kg body weight/rat) for 30 days.
On the day prior to sacrifice, oral glucose tolerance test (OGTT) was performed in all the groups of rats. As the insulin abnormality cannot be accurately detected by a single determination of insulin or glucose levels, the insulin resistance was evaluated by homeostasis model assessment of insulin resistance (HOMA-IR). Insulin resistance/sensitivity was assessed by quantitative insulin sensitivity check index (QUICK-I). After 30 days of treatment, the rats were fasted overnight, anesthetized and sacrificed by cervical decapitation. The biochemical parameters were analyzed using standard protocols. Blood was collected with and without anticoagulants for the separation of plasma and serum respectively. The levels of fasting blood glucose, hemoglobin, and glycosylated hemoglobin were estimated. Urine sugar was detected using urine strips. Ultrasensitive enzyme-linked immunosorbent assay (ELISA) kits were used for the assay of insulin and C-peptide. The levels of plasma protein, blood urea, serum uric acid, and serum creatinine were estimated. The results were expressed as mean±standard deviation of six rats per group and statistical significance was evaluated by one-way analysis of variance (ANOVA) using SPSS version 16 program (SPSS Inc., Chicago, IL, USA) followed by least significant difference. Values were considered statistically significant when P<0.05.
The effect of oral administration of the zinc-mixed ligand, Schiff base complex and metformin on glucose tolerance in diabetic rats after oral glucose load is represented in Table 1. Although the blood glucose levels reached a maximum peak value at 60 minutes after oral glucose load in all the three experimental groups of rats, the levels were significantly lower than those observed in diabetic group of rats and the peak was reversed to the physiological level in the next 60 minutes. However, the diabetic rats treated with zinc-mixed ligand complex showed statistically significant improvement in glucose homeostasis when compared to other two experimental groups of rats. Accordingly, the altered values of HOMA-IR and QUICK-I observed in the diabetic group of rats (7.80±0.06 and 0.30±0.01, respectively) were brought back to near normal values (4.01±0.04 and 0.38±0.01, respectively) upon treatment with oral administration of mixed ligand zinc complex.
Table 2 depicts the levels of fasting blood glucose, hemoglobin, glycosylated hemoglobin, plasma insulin, C-peptide, plasma protein, urea, uric acid, and creatinine in control as well as experimental groups of rats. The fasting blood glucose levels were elevated in the experimental diabetic rats which ultimately leads to elevated glycosylated hemoglobin levels. Plasma insulin and C-peptide levels in the diabetic rats were markedly reduced when compared with control rats whereas these altered levels were significantly improved to physiological range in diabetic rats treated with Schiff base as well as mixed ligand zinc complex. Urine sugar which was present in diabetic rats was no longer detected in the treated groups of rats.
The synthesis of a Schiff base ligand (L) from the co-ordination between 3-hydroxyflavone and metformin by a molar ratio method was yellow in color. Similarly, the new zinc-mixed ligand complex synthesized using Schiff base ligand (L) and zinc acetate was pale yellow in color and the yield was about 96%. The molecular formula of the proposed zinc-mixed ligand complex is C38H35N10O4 Zn. The IR, Mass spectra, 1H NMR, and 13C NMR spectral data provide a substantial evidence for the synthesis of the zinc-mixed ligand complex.
The data obtained through the oral glucose tolerance test evidenced the better efficacy of the zinc-mixed ligand complex than the metformin-3-hydroxyflavone complex in maintaining normoglycemia. The observed increase in the levels of fasting blood glucose and HbA1c is attributed to the insulin insufficiency and/or insulin resistance in diabetic rats. The normalization of altered biochemical parameters suggest that the zinc complex improves glucose homeostasis in diabetic rats and the efficacy was found to be superior to the Schiff base treated group of rats and the same was comparable with metformin which was administered at a concentration of 50 mg/kg body weight.
Enhanced insulin resistance coupled with increased muscle wasting is responsible for the observed decrease in protein synthesis which resulted in decreased plasma protein level in diabetic condition [15]. Muscle wasting due to chronic hyperglycemia leads to prominent scarcity of both hepatic as well as plasma proteins which in turn results in the excessive accumulation of nitrogenous wastes such as urea, uric acid, and creatinine in the systemic circulation than its excretion. The administration of zinc-mixed ligand complex to diabetic rats normalized the levels of plasma protein, blood urea, uric acid, and creatinine indicating the recovered renal function due to improved glycemic control [16].
The data obtained through OGTT, HOMA-IR, QUICK-I, and biochemical parameters evidenced that the oral administration of zinc-mixed ligand complex significantly improves the insulin sensitivity in diabetic rats to maintain normoglycemia. Normalization of protein metabolism upon treatment with zinc-mixed ligand complex suggests that the complex exerts beneficial effects on renal functions. In summary, the results of the present study clearly established that the zinc-mixed ligand complex shows better antidiabetic properties relatively at a lesser concentration than the Schiff base indicating that the addition of zinc significantly improved the efficacy of metformin-3-hydroxyflavone. Further studies are in progress to understand the molecular mechanisms involved in the action of zinc-mixed ligand complex in ameliorating the primary and secondary complications of T2DM.
ACKNOWLEDGMENTS
The research fellowship awarded by the University Grants Commission, Government of India, to Mr. K. Muruganantham (GCCO/A-2/UGC-MERITORIOUS/2015/1552 dated 19th November 2015) is gratefully acknowledged.
References
1. Thule PM. Mechanisms of current therapies for diabetes mellitus type 2. Adv Physiol Educ. 2012; 36:275–283. PMID: 23209008.
2. Pandey A, Tripathi P, Pandey R, Srivatava R, Goswami S. Alternative therapies useful in the management of diabetes: a systematic review. J Pharm Bioallied Sci. 2011; 3:504–512. PMID: 22219583.
3. Cornard JP, Merlin JC. Comparison of the chelating power of hydroxyflavones. J Mol Struct. 2003; 651-3:381–387.

4. Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999; 281:2005–2012. PMID: 10359389.
5. Yoshikawa Y, Yasui H. Zinc complexes developed as metallopharmaceutics for treating diabetes mellitus based on the bio-medicinal inorganic chemistry. Curr Top Med Chem. 2012; 12:210–218. PMID: 22236156.

6. Coulston L, Dandona P. Insulin-like effect of zinc on adipocytes. Diabetes. 1980; 29:665–667. PMID: 7002679.

7. Vijayaraghavan K, Iyyam Pillai S, Subramanian SP. Design, synthesis and characterization of zinc-3 hydroxy flavone, a novel zinc metallo complex for the treatment of experimental diabetes in rats. Eur J Pharmacol. 2012; 680:122–129. PMID: 22327044.

8. Sendrayaperumal V, Iyyam Pillai S, Subramanian S. Design, synthesis and characterization of zinc-morin, a metal flavonol complex and evaluation of its antidiabetic potential in HFD-STZ induced type 2 diabetes in rats. Chem Biol Interact. 2014; 219:9–17. PMID: 24854284.

9. Uma Maheswari J, Iyyam Pillai S, Subramanian SP. Zinc-Silibinin complex: synthesis, spectral characterization and biochemical evaluation of antidiabetic potential in high fat fed low dose STZ induced type 2 diabetic rats. J Chem Pharm Res. 2015; 7:2051–2064.
10. Gopalakrishnan V, Iyyam Pillai S, Subramanian SP. Synthesis, spectral characterization, and biochemical evaluation of antidiabetic properties of a new zinc-diosmin complex studied in high fat diet fed-low dose streptozotocin induced experimental type 2 diabetes in rats. Biochem Res Int. 2015; 2015:350829. PMID: 26783461.

11. Jaiganesh C, Roshana Devi V, Iyyam Pillai S, Subramanian S. Synthesis, characterization and evaluation of antidiabetic properties of a new metformin-3-hydroxyflavone complex studied in high fat diet fed-low dose streptozotocin induced experimental type 2 diabetes in Wistar rats. Int J Pharm Bio Sci. 2017; 8:1–15.

12. Jaiganesh C, Subramanian S. Metformin-3-hydroxyflavone, a new schiff base complex modulates the activities of carbohydrate regulatory enzymes in high fat diet fed-low dose streptozotocin induced type 2 diabetes in experimental rats. J Chem Pharm Res. 2017; 9:90–100.
13. Cornard JP, Vrielynck L, Merlin JC, Wallet JC. Structural and vibrational study of 3-hydroxyflavone and 3-methoxyflavone. Spectrochim Acta A Mol Biomol Spectrosc. 1995; 51:913–923.

14. Srinivasan K, Viswanad B, Asrat L, Kaul CL, Ramarao P. Combination of high-fat diet-fed and low-dose streptozotocin-treated rat: a model for type 2 diabetes and pharmacological screening. Pharmacol Res. 2005; 52:313–320. PMID: 15979893.

15. Park SW, Goodpaster BH, Lee JS, Kuller LH, Boudreau R, de Rekeneire N, Harris TB, Kritchevsky S, Tylavsky FA, Nevitt M, Cho YW, Newman AB. Health, Aging, and Body Composition Study. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care. 2009; 32:1993–1997. PMID: 19549734.

Table 1
Effect of zinc mixed ligand complex on oral glucose load test in experimental type 2 diabetic mellitus rats
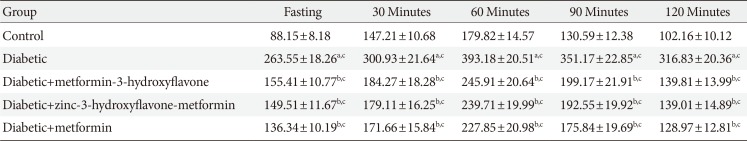
Table 2
The levels of fasting blood glucose, HbA1c, plasma insulin, C-peptide, urine sugar, plasma protein, blood urea, uric acid, and serum creatinine in control and experimental groups of rats
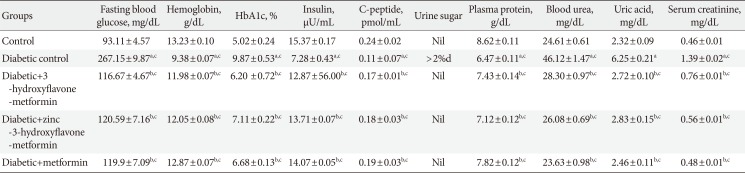
Values are presented as mean±standard error of the mean (n=6). One-way analysis of variance followed by post hoc test least significant difference was done.
HbA1c, glycosylated hemoglobin.
The results were acompared to control rats and bcompared to diabetic rats, cValues are statistically significant at P<0.05, dThis value indicates more than 2% sugar in urine sample.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download