1. Kotloff KL, Riddle MS, Platts-Mills JA, Pavlinac P, Zaidi AK. Shigellosis. Lancet. 2018; 391:801–812. PMID:
29254859.

2. Gentle A, Ashton PM, Dallman TJ, Jenkins C. Evaluation of molecular methods for serotyping Shigella flexneri. J Clin Microbiol. 2016; 54:1456–1461. PMID:
26984974.

3. Killackey SA, Sorbara MT, Girardin SE. Cellular aspects of Shigella pathogenesis: focus on the manipulation of host cell processes. Front Cell Infect Microbiol. 2016; 6:38. PMID:
27066460.

4. Khan WA, Griffiths JK, Bennish ML. Gastrointestinal and extra-intestinal manifestations of childhood shigellosis in a region where all four species of Shigella are endemic. PLoS One. 2013; 8:e64097. PMID:
23691156.

5. Banga Singh KK, Ojha SC, Deris ZZ, Rahman RA. A 9-year study of shigellosis in Northeast Malaysia: antimicrobial susceptibility and shifting species dominance. Z Gesundh Wiss. 2011; 19:231–236. PMID:
21654922.

6. Puzari M, Sharma M, Chetia P. Emergence of antibiotic resistant Shigella species: a matter of concern. J Infect Public Health. 2018; 11:451–454. PMID:
29066021.

7. Ashkenazi S, Cohen D. An update on vaccines against Shigella. Ther Adv Vaccines. 2013; 1:113–123. PMID:
24757519.

8. Harikrishnan H, Banga Singh KK, Ismail A. Outer membrane proteins analysis of Shigella sonnei and evaluation of their antigenicity in Shigella infected individuals. PLoS One. 2017; 12:e0182878. PMID:
28846684.

9. Mani S, Wierzba T, Walker RI. Status of vaccine research and development for Shigella. Vaccine. 2016; 34:2887–2894. PMID:
26979135.

10. Pore D, Mahata N, Pal A, Chakrabarti MK. Outer membrane protein A (OmpA) of Shigella flexneri 2a, induces protective immune response in a mouse model. PLoS One. 2011; 6:e22663. PMID:
21818362.

11. Tettelin H. The bacterial pan-genome and reverse vaccinology. Genome Dyn. 2009; 6:35–47. PMID:
19696492.

12. Pizza M, Scarlato V, Masignani V, et al. Identification of vaccine candidates against serogroup B meningococcus by whole-genome sequencing. Science. 2000; 287:1816–1820. PMID:
10710308.

13. He Y, Xiang Z, Mobley HL. Vaxign: the first web-based vaccine design program for reverse vaccinology and applications for vaccine development. J Biomed Biotechnol. 2010; 2010:297505. PMID:
20671958.

14. Gardy JL, Laird MR, Chen F, et al. PSORTb v.2.0: expanded prediction of bacterial protein subcellular localization and insights gained from comparative proteome analysis. Bioinformatics. 2005; 21:617–623. PMID:
15501914.

15. Krogh A, Larsson B, von Heijne G, Sonnhammer EL. Predicting transmembrane protein topology with a hidden Markov model: application to complete genomes. J Mol Biol. 2001; 305:567–580. PMID:
11152613.
16. Sachdeva G, Kumar K, Jain P, Ramachandran S. SPAAN: a software program for prediction of adhesins and adhesin-like proteins using neural networks. Bioinformatics. 2005; 21:483–491. PMID:
15374866.

17. Doytchinova IA, Flower DR. VaxiJen: a server for prediction of protective antigens, tumour antigens and subunit vaccines. BMC Bioinformatics. 2007; 8:4. PMID:
17207271.

18. Naz A, Awan FM, Obaid A, et al. Identification of putative vaccine candidates against Helicobacter pylori exploiting exoproteome and secretome: a reverse vaccinology based approach. Infect Genet Evol. 2015; 32:280–291. PMID:
25818402.

19. Nielsen H. Predicting secretory proteins with SignalP. Methods Mol Biol. 2017; 1611:59–73. PMID:
28451972.

20. Wilkins MR, Gasteiger E, Bairoch A, et al. Protein identification and analysis tools in the ExPASy server. Methods Mol Biol. 1999; 112:531–552. PMID:
10027275.

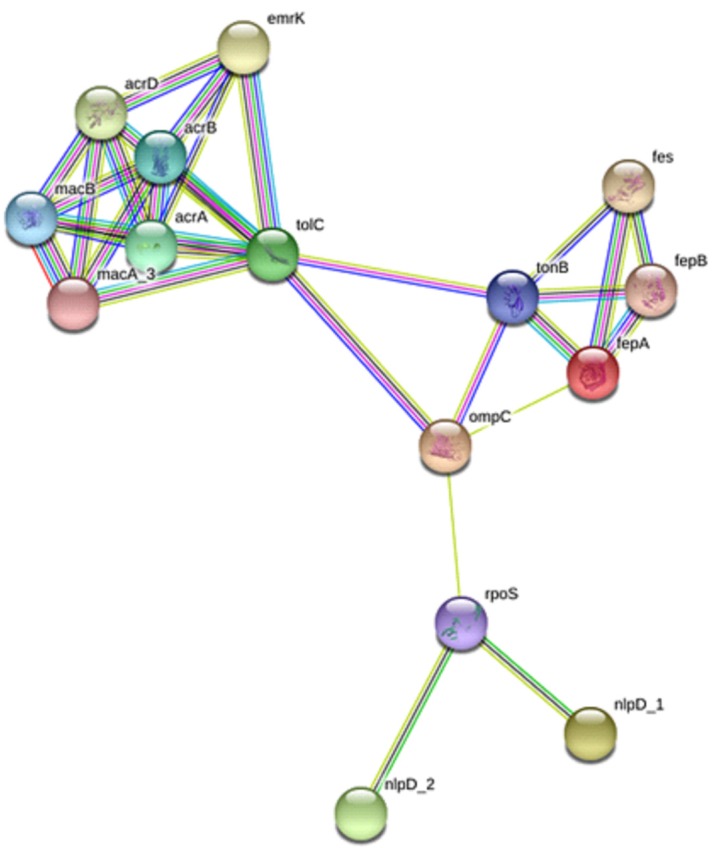
21. Szklarczyk D, Franceschini A, Wyder S, et al. STRING v10: protein-protein interaction networks, integrated over the tree of life. Nucleic Acids Res. 2015; 43(Database issue):D447–D452. PMID:
25352553.

22. El-Manzalawy Y, Dobbs D, Honavar V. Predicting linear B-cell epitopes using string kernels. J Mol Recognit. 2008; 21:243–255. PMID:
18496882.
23. Wang X, Sun Q, Ye Z, et al. Computational approach for predicting the conserved B-cell epitopes of hemagglutinin H7 subtype influenza virus. Exp Ther Med. 2016; 12:2439–2446. PMID:
27703505.

24. Singh H, Raghava GP. ProPred: prediction of HLA-DR binding sites. Bioinformatics. 2001; 17:1236–1237. PMID:
11751237.

25. Singh H, Raghava GP. ProPred1: prediction of promiscuous MHC class-I binding sites. Bioinformatics. 2003; 19:1009–1014. PMID:
12761064.

26. Tatusov RL, Galperin MY, Natale DA, Koonin EV. The COG database: a tool for genome-scale analysis of protein functions and evolution. Nucleic Acids Res. 2000; 28:33–36. PMID:
10592175.

27. Levine MM, Kotloff KL, Barry EM, Pasetti MF, Sztein MB. Clinical trials of Shigella vaccines: two steps forward and one step back on a long, hard road. Nat Rev Microbiol. 2007; 5:540–553. PMID:
17558427.

28. Rappuoli R, Covacci A. Reverse vaccinology and genomics. Science. 2003; 302:602. PMID:
14576423.

29. Oprea M, Antohe F. Reverse-vaccinology strategy for designing T-cell epitope candidates for Staphylococcus aureus endocarditis vaccine. Biologicals. 2013; 41:148–153. PMID:
23582120.
30. Rollauer SE, Sooreshjani MA, Noinaj N, Buchanan SK. Outer membrane protein biogenesis in Gram-negative bacteria. Philos Trans R Soc Lond B Biol Sci. 2015; 370:20150023. PMID:
26370935.

31. Maldonado RF, Sa-Correia I, Valvano MA. Lipopolysaccharide modification in Gram-negative bacteria during chronic infection. FEMS Microbiol Rev. 2016; 40:480–493. PMID:
27075488.

32. Jennison AV, Raqib R, Verma NK. Immunoproteome analysis of soluble and membrane proteins of Shigella flexneri 2457T. World J Gastroenterol. 2006; 12:6683–6688. PMID:
17075984.
33. Jarzab A, Witkowska D, Ziomek E, et al. Cyclic OmpC peptidic epitope conjugated to tetanus toxoid as a potential vaccine candidate against shigellosis. Vaccine. 2018; 36:4641–4649. PMID:
29960802.

34. Mathavan I, Beis K. The role of bacterial membrane proteins in the internalization of microcin MccJ25 and MccB17. Biochem Soc Trans. 2012; 40:1539–1543. PMID:
23176513.

35. Livermore DM. beta-Lactamases in laboratory and clinical resistance. Clin Microbiol Rev. 1995; 8:557–584. PMID:
8665470.

36. Raja SB, Murali MR, Devaraj SN. Differential expression of ompC and ompF in multidrug-resistant Shigella dysenteriae and Shigella flexneri by aqueous extract of Aegle marmelos, altering its susceptibility toward beta-lactam antibiotics. Diagn Microbiol Infect Dis. 2008; 61:321–328. PMID:
18358664.
37. Levy SB. Active efflux mechanisms for antimicrobial resistance. Antimicrob Agents Chemother. 1992; 36:695–703. PMID:
1503431.

38. Yang H, Duan G, Zhu J, et al. The AcrAB-TolC pump is involved in multidrug resistance in clinical Shigella flexneri isolates. Microb Drug Resist. 2008; 14:245–249. PMID:
19035770.
39. Miethke M, Marahiel MA. Siderophore-based iron acquisition and pathogen control. Microbiol Mol Biol Rev. 2007; 71:413–451. PMID:
17804665.

40. Ashida H, Ogawa M, Mimuro H, Kobayashi T, Sanada T, Sasakawa C. Shigella are versatile mucosal pathogens that circumvent the host innate immune system. Curr Opin Immunol. 2011; 23:448–455. PMID:
21763117.

41. Bagchi AK, Sinha AK, Adhikari R, Mukherjee J. Adaptive immune responses during Shigella dysenteriae type 1 infection: an in vitro stimulation with 57 kDa major antigenic OMP in the presence of anti-CD3 antibody. Mol Cell Biochem. 2010; 338:1–10. PMID:
19915959.
42. Kazi A, Chuah C, Majeed AB, Leow CH, Lim BH, Leow CY. Current progress of immunoinformatics approach harnessed for cellular- and antibody-dependent vaccine design. Pathog Glob Health. 2018; 112:123–131. PMID:
29528265.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download