Journal List > J Korean Acad Nurs > v.49(6) > 1142081
This study identified factors related to the quality of care in nursing homes, and elicited consensus opinions from experts on nursing homes.
A Delphi questionnaire was developed based on a review of the literature using the keywords “nursing homes,” “workforce,” and “quality of care.” A total of two Delphi surveys were conducted with 14 experts. The important and urgent factors related to the quality of care for nursing home residents emerged.
A consensus was achieved on the important and urgent factors relating to the quality of care. The related factors were grouped into four sections: Organizational Characteristics, Staffing Characteristics, the Long-Term Care Market and Legal and Policy Issues, and Nursing Processes. In total, 23 items were important factors and 26 items were urgent factors relating to the quality of care. In addition, the unanimous advocacy by the experts for increased hours per resident day for registered nurses (RNs, 41 minutes 59 seconds) was much higher than the current hours per resident day of RNs in Korea.
Korea is progressing toward becoming a developed nation in elder care, with the number of nursing homes increasing rapidly from 1,332 in 2008 to 3,289 in 2017 [1]. Following the adoption of Long-Term Care Insurance (a national social insurance) in 2008, 8% of elderly (585,287 elderly people) were eligible for long-termcare insurance in 2017 in Korea [1]. Considering that a high proportion of residents suffer from geriatric disease such as dementia, stroke, and Parkinson's disease, the need for appropriate health care is quite urgent. Furthermore, with an increasing numbers of elderly people diagnosed with dementia, researchers have continually mentioned that nursing home residents comprise a very vulnerable group [2]. Additionally, the coexistence of acute and chronic diseases lead to limitations in activities of daily life (ADL) for most residents, with about 56.3% needing help with ADLs due to walking or cognitive dysfunctions [3]. However, the quality of care in nursing home in Korea is still threatened, with 18.4% of the total sample size of nursing home residents experiencing a fall after being admitted to a nursing home [2]. In addition, urinary incontinence was observed in 48.0% of elderly people after being admitted to a nursing home [4]. Considering the frequency of emergency situations, such as falls and the need for endobronchial suction, the absence of resident doctors and limitations in the use of an affiliated health care facility mean that prompt and accurate judgment and corresponding emergency-care treatment skills of professional nurses are essential. Furthermore, in Korea, health care treatment in nursing homes is limited to acute treatments that are done by visiting a doctor in an affiliated health care organization, ignoring long-term management [5].
The quality of care in nursing homes has been affected by various factors including the physical characteristics of a facility, its employees, characteristics of the residents, the working environment for the staff, role ambiguity and conflict among employees, job stress, turnover rates, and a lack of human and material resources [67891011]. Improving the quality of care in nursing homes, including providing appropriate care and nursing services, not only increases the physical and cognitive functions of the elderly, but also improves the quality of life for the elderly [7]. Furthermore, appropriate nurse staffing decreases the number of falls, pressure ulcers, medication use, and the death rates of nursing home residents, as well as positively affects satisfaction with general care [6].
In particular, the quality of nursing staff in nursing homes that directly provide long-term elderly care service is an important factor that determines the quality of the long-term elderly care service. Most importantly, the quality of nursing staff affects the quality of care and the quality of life of nursing home residents [8]. In systematic reviews of nursing staff and quality of care, researchers reported that the quality of care of elderly residents improved with increased hours per resident day (HPRD), an increased proportion of registered nurses (RNs) compared to certified nurse aides (CNAs), and a decreased turnover rate of RNs [89]. Furthermore, when the organization hired more RN staff, the occurrence rate of pressure ulcers, use of psychotropic drugs, depression, cognitive decline, and mortality decreased, whereas the discharge rate from nursing homes increased [12].
In Korea, the total number of nurses who work in nursing homes was estimated at 1,485; representing only 1.8% of the total nursing home staff [1]. Thus, the appropriate treatment and the quality of care for elders living in nursing homes is worrying. In the United States, federal- and state-level requirements, expert recommendations have been proposed for several decades: The Hartford Institute for Geriatric Nursing Experts Panel (Hartford), Centers for Medicare and Medicaid (CMS), and the Institute of Medicine (IOM)—major national and related agencies in the United States—presented proposed proportions of staff with detailed but varied staff categorization standards for elderly-care facilities. For the minimum provision of HPRD, the CMS requires 0.75 hours (45 minutes) of RNs, 0.55 hours (33 minutes) of nursing assistants, and 2.8 hours (2 hours 48 minutes) of care workers. In 1996, the IOM suggested a 24-hour mandatory attendance of RNs.; They also recommended that the level of nursing-staff placement be increased based on the number of elderly residents, and that at least one RN should be present at all times [13]. However, the current policy for nursing home residents in Korea did not reflect differences in the roles and functions of RNs and CNAs, with most staff being CNAs rather than RNs. Smaller elderly care facilities have larger proportions of CNAs [14]. This is because a related statute allows the replacement of RNs (licensing system) with CNAs (certification system), disregarding the differentiations between the two groups. The two groups differ in the licensing and certification processes, as well as educational backgrounds and legal roles and responsibilities. The disregard of said differentiations mitigates the standard of placement of nursing staff in nursing homes [15]. Most nursing homes in Korea have hired CNAs to reduce the cost of hiring RNs. In addition, care provided by nursing staff is associated with the quality of care [671011]. The characteristics of an organization—for example, the better the working environment and the more pleasant the residents' environment—also relate to the quality of care [1011]. The competition index also relates that the quality of care is better when there are more nursing homes in an area [1011].
The quality of nursing staff in elderly care facilities is an important factor that determines the quality of service of long-term care for the elderly [16]. However, even experts in Korea have not reached an agreement about the specificities regarding staff, working environment, working conditions, and government regulations. These differing opinions make it difficult to find ways to improve the quality of care or the enactment of laws. In addition, no consensus emerged regarding the required number of HPRD to improve the quality of care, and it is not even possible to determine the appropriate level of HPRD for nursing homes. Thus, to have high-quality care provided in nursing homes in Korea, an agreement should be made on the factors that are important and urgent. To reach this agreement, validated recommendations from nursing home experts are required. The Delphi method is appropriate to generate a consensus based on the information needed [17]. For Korea's successful entry into the developed-nation status in elderly care, efforts are required to improve the optimal quality of nursing home residents' care and to efficiently operate long-term elderly care insurance. Prior studies have considered the relationship between specific factors selected by the researchers and the quality of care, but it is high time for an agreement.
The purpose of this study was to achieve a consensus on the necessary level of quality of care for elderly residents in nursing homes by using the Delphi method. For this study, we obtained opinions from a group of experts on RN staff requirements. The goal is to achieve optimal nursing staff in nursing homes.
This study was a Delphi study conducted to identify the factors that associated with the quality of care for nursing home residents by surveying experts twice with a semi-structured survey that was compiled after reviewing related literature.
The recommended number of participants required for a Delphi study is 5 to 20 [18]. Useful results can be obtained from a small group of 10 to 15 experts [19]. Considering the drop-out rate, we recruited 14 experts in various nursing home fields (i.e., a director, a professor who studies nursing home care, and nursing home staff). After reviewing whether they met the selection criteria, we made the final selection. The specific expert-inclusion criteria are as follows: (a) People with more than 5 years of experience working at a nursing home with 29 or more residents. We assumed such people would have a general understanding of the operation of the nursing home and care for residents in nursing homes; (b) People who have carried out research on nursing homes and nurse staffing for more than 10 years. Participants in the Delphi survey comprised 3 university faculty members whose research area focused on nursing home residents' outcomes, 4 administrators of nursing homes with more than 10 years of experience as administrators, 3 directors of offices specializing in elderly care, 3 bedside RNs whose specialty was in nursing homes, and 1 social worker. We achieved a 100.0% response rate. In the second Delphi survey, only 13 of 14 participants responded with a 92.9% response rate.
We developed items on the Delphi survey based on a literature review of factors that related to the quality of care in nursing homes. For a scientific search, we used PubMed, CINAHL Plus with Full Text, the Cochrane Library, Lexicomp online, PsyclNFO, PsyARTICLES Digital Library of the National Assembly, the Research Information Service System, and the Korean Studies Information Service System using the following keywords: quality of care, nursing home, long-term care, workforce, work environment, practice environment, turnover, and policy change. We searched for information and research on laws related to nursing home staffing using WESTLAW. After reviewing the abstracts of 97 searched papers, we selected 54 research papers limited to research on nursing home quality. We grouped the associated factors into four sections consisting of Organizational Characteristics, Staffing Characteristics, the Long-Term Care Market and Legal and Policy Issues, and Nursing Processes using Donabedian's structure–process–outcome quality-of-care model [20]. This model's three-part approach makes quality assessment possible, assuming that structure (organizational characteristics, staffing characteristics, long-term care market and legal and policy issues) influences process (nursing processes), which in turn, influences outcome (quality of care). We selected items that are frequently presented as factors related to quality of care in previous research. The area of Organizational Characteristics of nursing homes included 12 items on general characteristics, 11 items on physical and emotional environments, and 6 items on the working environment. The area of Staffing Characteristics included 7 items on nursing staff, 11 items on staff other than nursing, and 22 items on organizational culture, leadership, and delegation. The area of Nursing Processes is a single-category and had 8 items. The area of the Long-Term Care Market and Legal and Policy Issues comprised 7 items on the characteristics of the health care market and 2 items on law and policy.
We asked participants to evaluate the degrees of importance and urgency of each item using a 5-point Likert-type scale with higher scores indicating more importance and urgency. Additionally, to present the optimal number of nursing staff, we provided the Safe Staffing for Quality Care Act (S3691A-2013) in the United States [21], which designates 45 minutes as the minimum period of time per resident day for nurses at elderly care facilities. We also provided the results of previous research on the HPRD of 45 elderly care facilities in Korea (11 minutes 5 seconds for RNs, 10 minutes 31 seconds for CNAs, and 2 hours 42 minutes 28 seconds for care workers), and 60 elderly care facilities (6 minutes 29 seconds for RNs, 9 minutes 43 seconds for CNAs, 2 hours 34 minutes 48 seconds for caretakers) [1011]. Furthermore, the survey included an essay question to collect opinions about the HPRD of nursing staff for optimal care. The questions also sought opinions on the mandatory placement of RNs in nursing homes.
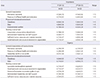
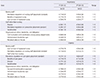
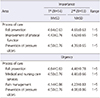
We compiled the second Delphi survey by deleting the items with scores less than 3.5 of 5 in the first Delphi survey (see Tables 1,2,3,4). The items deleted after the first survey were the following: opening year of the facility, religious affiliation, allowance of pets in the facility, and existence of labor in the facility (Table 5 provides a full list). We then restructured the survey by revising and supplementing the identical questions. Based on the results of the first Delphi survey, we surveyed degree of importance by including the following: 8 items on the general characteristics, 10 items on the physical and emotional environment, and 6 items on the working environment in the area of Organizational Characteristics; 7 items on the nursing staff, 9 items on staff other than nursing, and 21 items on organizational culture, leadership, and delegation in the area of Staffing Characteristics; 8 items in the area of Nursing Processes; 5 items on the characteristics of the health care market, and one item on law and policy in the area of Long-Term Care Market and Legal and Policy Changes. Additionally, we surveyed the topic of urgency by including the following: 5 items on general characteristics, 10 items on physical and emotional environments, and 6 items on working environments in the area of Organizational Characteristics; 7 items on nursing staff, 7 items on staff other than nursing, and 20 items on organizational culture, leadership, and delegation in the area of Staffing Characteristics; 7 items in the area of Nursing Processes; 3 items on characteristics of the health care market and one item on law and policy in the area of Long-Term Care Market and Legal and Policy Changes. Furthermore, we presented the results of the first Delphi survey about the HPRD for optimal care (average for RNs: 36 minutes 6 seconds; CNAs: 45 minutes 24 seconds; and care workers: 3 hours 25 minutes 42 seconds), This provided an opportunity for the experts to reassess and revise their opinions by comparing their own responses to the average responses. The areas of items and the scoring methods were identical to that of the first Delphi survey.
Ethical approval for this study was obtained from the institutional review board of E university (approval no. 154-10). The first Delphi survey was conducted from August 8 to September 4, 2018; and the second Delphi survey was conducted from September 13 to October 4, 2018. The researchers telephoned several experts listed as experts providing advice on the specific fields researched in this study in order to seek their consent. Participants were 3 bedside RNs for residents in nursing homes who had worked for more than 5 years and 5 researchers whose specialty focuses on nursing home staffing for more than 10 years. Participants understood the purpose and necessity of the research and agreed to participate.
The surveys were distributed either directly to the person or indirectly through e-mail. We asked participants to check the level of the importance and urgency of each item on a 5-point Likert-type scale (5=very important, very urgent, 1=totally unimportant, not at all urgent) on the first Delphi survey. After some items from the first Delphi Survey were deleted, we provided feedback to all participants on the mean, standard deviation, and level of consensus for all statements on the second Delphi survey. We asked participants to check the level of importance and urgency of each item on a 5-point Likert-type scale (5=very important, very urgent, 1=totally unimportant, not at all urgent) on Delphi Survey 2. Research participants received monetary compensation of about USD 30 on each occasion.
Study researchers analyzed the collected data with means and standard deviations using the SPSS 25.0 statistical program. By determining items with the highest scores in each area, we identified items of high importance and urgency among factors that were related to the quality of care for nursing home residents. For each item measured on a 5-point scale, only items experts selected with an average of 3.5 or higher are included in the final analysis.
The results of this study are summarized in terms of the items that converged through the Delphi surveys on the four domains. In this paper, we present the analysis results of the first and second Delphi surveys, where the results show the highest importance and urgency items. The mean score of importance and urgency appear in the tables. For the proposal for quality of care, the agreed results in each area through the first and second Delphi surveys are as follows.
In the first survey, “cleanliness” and “odor” were measured as the most important items, whereas in the second survey, “cleanliness,” “cooperation among various departments,” and “administrator's leadership and staff support” were the most important items. In the first survey, “odor,” “successful interdisciplinary approach,” and “good teamwork and secure environment in the organization” scored as the most urgent items, whereas in the second survey, “cleanliness” was the most urgent item (see Table 1).
In the first survey, “communication and coordination among various departments” scored as the most important item whereas in the second survey, “communication and coordination among various departments,” “administrator's leadership type,” and “perceived value on the job” were the most important items. In the first survey, “successful interdisciplinary approach” scored as the most urgent item; while on the second survey, “mandatory regulation on care worker placement” was the most urgent item (see Table 2). In addition, in the second survey, we presented the convergence of opinions from the first survey and asked participants to reassess the same questions. Results indicated 41 minutes 59 seconds for RNs, 47 minutes 22 seconds for CNAs, and 3 hours 25 minutes 23 seconds for careworkers. This figure is higher than the results from the first survey for all categories.
In the first and the second rounds, the most important item was “fall prevention.” In addition, in both the first and the second rounds, the most urgent item was “fall prevention” (see Table 3).
In the first and second rounds, the most important item was “long-term care insurance in 2008.” In the first survey, “long-term care insurance in 2008” scored as the most urgent item whereas in the second survey, “Number of registered nurses in the area of the nursing home” was the most important urgency item (see Table 4).
The goal of this research was to identify factors related to the quality of care for elderly residents of nursing homes to provide quality long-term elderly care services. For characteristics of nursing homes, survey participants identified cleanliness as the most important and urgent factor. As an operating standard of nursing homes, the environment of the facility should always be clean and attention paid to hygiene management [16]. However, 12 nursing homes have had tuberculosis infections and 10 infected with Ohm have been confirmed to have received treatment in Korea [22]. In addition, apart from a study on the relationship between the level of cleanliness and the quality of care in nursing homes, no study has assessed the level of cleanliness. Because “cleanliness” is the most important and urgent factor in the quality of care in this study, it is necessary to identify and improve the cleanliness in nursing homes.
Meanwhile, the strengthening of standards to establish the facility and ownership (profit or nonprofit) were found to be of less importance and urgency in this study, but this is important and requires discussion. In Korea, long-term care facilities are managed mostly by nonprofit organizations, but with the adoption of long-term care insurance in 2008, standards were lowered so private for-profit businesses could also establish and manage long-term care facilities to supply quantitative infrastructure within a short period of time. Due to the decreasing standards that require only the registration of the establishment and the easier establishment of smaller facilities, the number of facilities has greatly increased [23]. However, the user-centered operation style and the provision of facility benefits expected without considering the severity of the cases of elderly residents by grade and the standard of staff and facilities, while not accounting for the size of the facility, make it difficult to maintain the operation of elderly care facilities [24]. This difficulty has resulted in an increase in the accessibility of elderly residents to facilities but a decrease in the quality of long-term care services. According to the results of the facility evaluation by long-term care providers in 2015, local government facilities scored 87.6, incorporated facilities scored 80.1, and private facilities scored 69.7 [25]. Scores showed that the qualities of for-profit private facilities were relatively low. Unlike Korea, where private facilities already account for a higher proportion (80%), in Sweden, public facilities had a higher quality of care than private facilities, the number of which are increasing slightly [26]. Furthermore, a previous study on the effect of ownership of elder-care facilities on the quality of long-term care services reported that nonprofit facilities provide higher quality care compared to for-profit facilities [27]. Profit-driven nursing homes struggle to minimize expenditures. This struggle to minimize expenditures may lead to a lower quality of staffing and higher rates of adverse events, which in turn may lead to an over-all lower quality of care [27]. We also present a contrasting study. In Denmark, where private schools account for only 14% of the population, for-profit facility providers are allowed to operate their own waiting lists and can decide which residents to admit [28]. They are also allowed to provide extra services and charges for these patients [28]. For this reason, a study of public quality in Denmark showed no relationship between public quality and quality of care. As inconsistent research results emerged in each situation in each country, the relationship between public quality and quality of care should be studied further.
In relation to the staff and working environment of nursing homes, the leadership and support of the administrative staff and sufficient human and material resources were identified as most important and urgent factors. Additionally, cooperation among various departments, good teamwork, a secure environment in an organization, and a structural foundation to provide quality of care showed high scores. Nursing homes provide daily medical services along with cultural activities, leisure activities, social participation, and religious activities [29]. Therefore, each ministry performing them will have to cooperate to provide quality care to residents. Cooperation among departments contributes to enhancing the quality of care by enhancing employee satisfaction and improving understanding of residents [30]. This is the reason teamwork is an important and urgent factor to improve quality of care. To increase cooperation among departments, employees should take time to understand each other's work through regular communication. It is the leader's role to set the stage for such communication, and employees involved in communication need to actively discuss their opinions and difficulties, understand each other, and seek ways to enhance prosperity for all.
Previous researchers showed that the work environments of nursing staff had a significant impact on the quality of care [29]. In a previous study on the job satisfaction of staff at elderly care facilities [30], low emotional burnout, high organizational support and empowerment, strong cohesion between job groups, and a high sense of personal achievement were associated with a high job satisfaction. In addition, the average monthly salary and high satisfaction about salaries had a positive impact on the quality of services. The management practices of administrators of elderly care facilities and the formation of organizational culture were related to the increase in organizational commitment of the facility's workforce [30]. Thus, the quality of the workforce that provides long-term care insurance services are directly associated with the stable quality of services.
For efficient human-resource management, the standards of staff placement must be increased at the government level and improvements in benefits such as salaries, work hours, and work conditions must be established. Moreover, continued research is needed to promote the change in elderly care facilities for the establishment of a cultural environment in which caring for elderly residents is deemed important. Staff value their own work through the provision of education for organizational support and emotional empowerment, as well as the provision of work environments in which self-actualization is possible at the facility level.
Factors related to quality of care in facilities were found to be pain management, fall prevention, and the prevention of pressure ulcers. Significantly, the RNs are those tasked to follow empirical practical guidelines through expert knowledge, appropriate bases, and systematic approaches. Among them, fall prevention was the most important and urgent nursing process. A study found that about 18.4% of the sample experienced falls, including slips, after admission to nursing homes in Korea [31]. The incidence of falls was highly associated with hospitalization and deteriorated functional abilities [32]. Furthermore, the costs related to hospitalization, caregiver payments, and medication are enormous [33]. Considering the provision of high-quality care and the fall prevention of elderly residents, the necessity to mandate the placement of nurses who directly provide care in elderly care facilities was assessed. Systematic reviews about the nursing staff in elderly care facilities and the quality of care in elderly care facilities have shown that nursing staff affect a reduction in the occurrence of bedsores, the use of restraining bands, and hospitalization rates [89] as well as falls [34]. High HPRD of nursing staff in elderly care facilities have affected the reduction in the occurrence of bedsores in elderly residents [35]. Thus, it is clear that the establishment of institutional and environmental bases for the improvement of HPRD for nursing staff is an essential factor to improve the quality of care.
In Korea, the data on HPRD was unavailable, but limited studies reported that the HPRD in 45 selected nursing homes were 11 minutes 5 seconds for RNs; while in a study of 60 nursing homes, the HPRD was 6 minutes 29 seconds for RNs [1011]. The expert opinion for optimal HPRD found in this study was at 41 minutes 59 seconds for RNs. In conclusion, a significant difference emerged between the HPRD required by experts and the actual provided HPRD for nursing homes in Korea. By collecting opinions from experts and determining the research results, it is necessary to calculate an appropriate level of nursing staff to improve quality of care and deploy an appropriate level of nursing staff in facilities.
Compared to the status of Korea, the U.S. elderly care expert panel in Hartford in 2000, required that one care director is continuously present to provide direct care for at least 4.13 hours (4 hours 8 minutes). In addition, they required at least one RN for every 15 elderly residents (day), 20 elderly residents (evening), and 30 elderly residents (night) [7]. In recently passed laws related to the minimum workforce, the state of California increased the minimum HPRD from 3.0 hours to 3.2 hours [13]. As a result of an increase in nursing staff of HPRD by 9%, a commensurate improvement in quality of care has been reported [36]. In addition, elderly care facilities in Japan are divided into health care facilities for the elderly, welfare facilities for the elderly, and health facilities for the elderly according to medical requirements [37]. All three types of facilities require one person from the nursing staff (RN or Care worker) to be deployed per three residents; however, each facility requires different rates of RN and care worker placement, depending on the level of medical function of the facility [37]. Nursing homes with the highest medical functions require a 1:1 ratio of RNs to care workers.
Korea's nurse staffing standards are significantly lower than those of other countries (U.S. and Japan). In the U.S, the standard of nurse staffing is the number of RNs per residents by shift, whereas in Korea, the standard is RNs per resident, regardless of shift. As a result, at night, Korea's nursing homes often have no nurses. In addition, the higher the medical needs of residents, the more nurses they are supposed to deploy in Japan, but that is not the case in Korea. The medical needs of residents should also be considered when calculating proper nurse staffing. For policy implications, the available professional supply of RNs was an important and urgent factor in attaining quality care. The current situation, in which about 80% of elderly care facilities in Korea do not hire RNs, differs markedly from developed nations that clearly present the legal requirements about nurse placement and minimum HPRD. The practical placement of essential RN staff is clearly urgent. Although the Korea Nursing Association and the Korean Gerontological Nurses Association have recently advanced the mandatory placement of professional nurses to improve the safety and optimal quality of care for elderly residents of elderly care facilities by issuing a statement urging improvement in the level of placement of nurses in nursing facilities, and to realize labor costs [38], it cannot be denied that policy measures must be prioritized first.
In relation to the staff, the long-term care market, and legal and policy changes in nursing homes, long-term care insurance in 2008 was selected as most urgent and important. This system was introduced to improve the quality of care. In the long-term care insurance system, the government provides facility benefits to elders who enter elderly care facilities [1]. We predict this item is important in assessing the quality of care because the system provides much support (i.e., facility benefits) for nursing homes. Government support has enabled facilities to provide better services to residents.
In addition, a need persists to raise citizens' awareness of nursing homes. The government should disclose information on the quality of care and consumers should be allowed to choose which facilities to utilize. This format would contribute to improving quality of care even in the advent of increasing numbers of private elderly care facilities which aim to profit by lowering care quality.
This study has several limitations. First, experts have identified the ranking of items related to the quality of care, but have not been able to identify the specific material and urgent content. Another limitation is that although the items were organized through literature review, experts did not identify other important and urgent matters. Therefore, it is proposed that studies in the form of focus group interviews be carried out for experts. It also suggests that the Delphi study will proceed with the addition of essay-type items to describe specific items.
The opinions expressed in this study converged on the notion that the roles of the Ministry of Health and Welfare, the directors of nursing homes, RNs, and care workers were important to improve the quality of care. Participants identified various factors associated with the quality of care in elderly care facilities. Combining the suggestions on these factors, improvement in the establishment of infrastructure is necessary at the political, institutional, and environmental levels to provide high-quality care at both the government and facility levels.
To have appropriate professional long-term elder care services in nursing homes in Korea, professional stable RNs who address pain management, fall prevention, and skin integrity are essential. In addition, political measures to establish a stable health care referral system for nursing home residents and the strengthening of standards for nursing home establishment and staffing are urgently needed. In particular, legal and policy changes are needed on the mandatory placement of RN staff with appropriate HPRD of RNs with professional knowledge and empirical clinical guidelines to meet the diverse health care needs of residents.
1. National Health Insurance Service. Long term care insurance statistical yearbook (2008–2015) [Internet]. Wonju: National Health Insurance Service;c2010–2016. cited 2019 Feb 21. Available from: https://www.nhis.or.kr/bbs7/boards/B0160/19799?boardKey=37&sort=sequence&order=desc&rows=10&messageCategoryKey=&pageNumber=1&viewType=generic&targetType=12&targetKey=37&status=&period=&startdt=&enddt=&queryField=&query=.
2. Kim JI. General characteristics of senior citizens in the care facilities and influence upon quality of life, their activities of daily living and social support affects. Korean Public Health Research. 2011; 37(1):97–108.
3. Sunwoo D. Policy issues in elderly health and long-term care policy. Health and Welfare Policy Forum. 2016; 239:34–48.
4. Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean Journal of Urology. 2009; 50(5):450–456. DOI: 10.4111/kju.2009.50.5.450.
5. Ministry of Health and Welfare. Enforcement regulations of the elderly welfare act; Article 22;1 [Internet]. Sejong: Ministry of Health and Welfare;c2019. cited 2019 Feb 21. Available from: http://law.go.kr/%EB%B2%95%EB%A0%B9/%EB%85%B8%EC%9D%B8%EB%B3%B5%EC%A7%80%EB%B2%95%20%EC%8B%9C%ED%96%89%EA%B7%9C%EC%B9%99.
6. Zúñiga F, Ausserhofer D, Hamers JPH, Engberg S, Simon M, Schwendimann R. Are staffing, work environment, work stressors, and rationing of care related to care workers' perception of quality of care? A cross-sectional study. The Journal of Post-Acute and Long-Term Care Medicine. 2015; 16(10):860–866. DOI: 10.1016/j.jamda.2015.04.012.
7. Shin JH. Relationship between nursing staffing and quality of life in nursing homes. Contemporary Nurse. 2013; 44(2):133–143. DOI: 10.5172/conu.2013.44.2.133.
8. Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JPH. Nurse staffing impact on quality of care in nursing homes: A systematic review of longitudinal studies. The Journal of Post-Acute and Long-Term Care Medicine. 2014; 15(6):383–393. DOI: 10.1016/j.jamda.2013.12.080.
9. Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: A systematic review. International Journal of Nursing Studies. 2011; 48(6):732–750. DOI: 10.1016/j.ijnurstu.2011.02.014.
10. Bowblis JR, Ghattas A. The impact of minimum quality standard regulations on nursing home staffing, quality, and exit decisions. Review of Industrial Organization. 2017; 50(1):43–68. DOI: 10.1007/s11151-016-9528-x.
11. Shin JH, Shin IS. The effect of registered nurses on nursing home residents' outcomes, controlling for organizational and health care market factors. Geriatric Nursing. 2019; 40(3):296–301. DOI: 10.1016/j.gerinurse.2018.11.004.
12. He J, Staggs VS, Bergquist-Beringer S, Dunton N. Nurse staffing and patient outcomes: A longitudinal study on trend and seasonality. BMC Nursing. 2016; 15:60. DOI: 10.1186/s12912-016-0181-3.
13. Harrington C, Choiniere J, Goldmann M, Jacobsen FF, Lloyd L, McGregor M, et al. Nursing home staffing standards and staffing levels in six countries. Journal of Nursing Scholarship. 2012; 44(1):88–98. DOI: 10.1111/j.1547-5069.2011.01430.x.
14. Lee JM, Park MJ, Han EJ, Suh EE. A study on management of medical needs of the elderly in Korean long-term care facilities. Seoul: National Health Insurance Service;2012. 11. p. 3–5. Report No.: 2012-19.
15. Ministry of Government Legislation. Regulations on certified nurse aides and medical service providers [Internet]. Sejong: Ministry of Health and Welfare;c2017. cited 2019 Feb 23. Available from: http://www.law.go.kr/%EB%B2%95%EB%A0%B9/%EA%B0%84%ED%98%B8%EC%A1%B0%EB%AC%B4%EC%82%AC+%EB%B0%8F+%EC%9D%98%EB%A3%8C%EC%9C%A0%EC%82%AC%EC%97%85%EC%9E%90%EC%97%90+%EA%B4%80%ED%95%9C+%EA%B7%9C%EC%B9%99.
16. Kim J, Lee SY. A study on care workers' job performance and competency at long-term care homes. Health and Social Welfare Review. 2013; 33(2):243–273.
17. Delbecq AL, Van de Ven AH, Gustafson DH. Group techniques for program planning: A guide to nominal group and Delphi processes. Glenview (IL): Scott, Foresman;1975. p. 5–19.
18. Rowe G, Wright G. Expert opinions in forecasting: The role of the Delphi technique. In : Armstrong JS, editor. Principles of Forecasting: A Handbook for Researchers and Practitioners. New York: Springer;2001. p. 125–144.
19. Ziglio E. The Delphi method and its contribution to decision-making. In : Adler M, Ziglio E, editors. Gazing into the Oracle: The Delphi Method and Its Application to Social Policy and Public Health. London: Jessica Kingsley;1996. p. 3–33.
20. Donabedian A. The quality of care. How can it be assessed? JAMA. 1988; 260(12):1743–1748.
21. TrackBill. An act to amend the public health law, in relation to establishing the “safe staffing for hospital care act” [Internet]. Washington, D.C.: TrackBill;c2013. cited 2019 Feb 21. Available from: https://trackbill.com/bill/new-york-senate-bill-1634-establishes-the-safe-staffing-for-hospital-care-act/399758/.
22. Kim IS. Ohm and tuberculosis warning for elderly care facilities [Internet]. Seoul: DailyMedipharm;c2012. cited 2019 Feb 21. Available from: http://www.dailymedipharm.com/news/articleView.html?idxno=6076.
23. Sunwoo D. Analysis of installation status and policy implications of long-term care facilities for the elderly. Health Welfare Issue & Focus. 2015; (299):1–8.
24. Jeong EH, Jang MK. Study on improvement of operation of long-term care facilities: Focused on the priority facilities of beneficiaries. Seoul: Seoul Welfare Foundation;2012. 12. p. 5–15. Report No.:2012-23.
25. Comondore VR, Devereaux PJ, Zhou Q, Stone SB, Busse JW, Ravindran NC, et al. Quality of care in for-profit and not-for-profit nursing homes: Systematic review and meta-analysis. British Medical Journal. 2009; 339:b2732. DOI: 10.1136/bmj.b2732.
26. National Health Insurance Service. Long-term care facility evaluation result [Internet]. Wonju: National Health Insurance Service;c2017. cited 2019 Feb 21. Available from: http://www.longtermcare.or.kr/npbs/d/m/000/moveBoardView?menuId=npe0000000770&bKey=B0009.
27. Kwon H, Hong K. The effect of publicness on the service quality in long-term care facilities. Korean Journal of Social Welfare. 2015; 67(3):253–280.
28. Hjelmar U, Bhatti Y, Petersen OH, Rostgaard T, Vrangbæk K. Public/private ownership and quality of care: Evidence from Danish nursing homes. Social Science & Medicine. 2018; 216:41–49. DOI: 10.1016/j.socscimed.2018.09.029.
29. Ma C, Olds DM, Dunton NE. Nurse work environment and quality of care by unit types: A cross-sectional study. International Journal of Nursing Studies. 2015; 52(10):1565–1572. DOI: 10.1016/j.ijnurstu.2015.05.011.
30. Kim JH, Jang CS. The effect of the working environment of elderly care facility employees on the care service quality and the mediation effect of social support. The Journal of the Korea Contents Association. 2016; 16(5):533–547. DOI: 10.5392/jkca.2016.16.05.533.
31. Park AJ, Lim NY, Kim YS, Lee YK, Song JH. Incidence and predictors of falls in institutionalized elderly. Journal of Muscle and Joint Health. 2011; 18(1):50–62. DOI: 10.5953/JMJH.2011.18.1.050.
32. National Council on Aging. National Falls Prevention Resource Center [Internet]. Arlington (VI): National Council on Aging;c2019. cited 2019 Feb 21. Available from: https://www.ncoa.org/center-for-healthy-aging/falls-resource-center/.
33. Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: A systematic review. Osteoporosis International. 2010; 21(8):1295–1306. DOI: 10.1007/s00198-009-1162-0.
34. Shin JH, Hyun TK. Nurse staffing and quality of care of nursing home residents in Korea. Journal of Nursing Scholarship. 2015; 47(6):555–564. DOI: 10.1111/jnu.12166.
35. Lee HY, Blegen MA, Harrington C. The effects of RN staffing hours on nursing home quality: A two-stage model. International Journal of Nursing Studies. 2014; 51(3):409–417. DOI: 10.1016/j.ijnurstu.2013.10.007.
36. Chen MM, Grabowski DC. Intended and unintended consequences of minimum staffing standards for nursing homes. Health Economics. 2015; 24(7):822–839. DOI: 10.1002/hec.3063.
37. Kang EN. Staffing standards for long-term care facilities in selected countries. Health and Welfare Policy Forum. 2015; 225:72–79.
38. Chung KS. Promoting the realization of labor costs for nurse specialty nursing home pilot project [Internet]. Seoul: The Korean Nurses Association News;c2019. cited 2019 Feb 21. Available from: http://www.nursenews.co.kr/main/ArticleDetailView.asp?sSection=62&idx=23769.
- TOOLS
- ORCID iDs
-
Juh Hyun Shin

https://orcid.org/0000-0001-8058-7195Eun Mee Kim

https://orcid.org/0000-0001-8373-6141Ji Yeon Lee

https://orcid.org/0000-0002-7216-5723 - Similar articles




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download