Abstract
Purpose
To determine nurse staffing by classifying patients based on their nursing care needs and to benchmark current staffing against the Safer Nursing Care Tool (SNCT) staffing requirements.
Methods
Cross-sectional data were collected from four general wards at a tertiary hospital. Nursing activities conducted by 86 registered nurses were observed at 10-minute intervals. The nursing care needs of 780 inpatients were measured with two dimensions: acuity (10 nursing activities) and dependency (four activities of daily living).
Results
Nurses worked for 9.3 hours per shift on average, reflecting overtime work of 1.3 hours per nurse. Nurses spent 37% of their time on direct care, 54% on indirect care, and 9% on associated work. Nursing hours per patient day increased as nursing care needs became higher. Patients were classified into four groups based on their level of nursing care needs. The staffing ratio of groups 1-4 was 1:9.8, 1:8.0, 1:7.0, and 1:4.6, respectively. The current staffing (i.e., nursing hours) was as low as 53% of the SNCT benchmark, resulting in informal caregiving by patients' family or their privately hired attendants.
Figures and Tables
 | Figure 1(A) A decision tree result from recursive partitioning approach for classifying patients based on their nursing care needs; (B) corresponding visualization on two dimensional plane of the result. |
Table 1
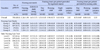
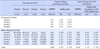
Nursing Activities and Hours Provided by Registered Nurses and Nursing Aides Empty Cells Indicate No Cases
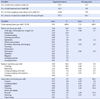
Table 2
Table 2. Relationships between the Items of the Nursing Care Needs and Nursing Hours per Patient and Shift Provided by Registered Nurses (N=780)

Acknowledgements
We thank Dr. Keith Hurst for providing support with the research methodology in data collection and analysis. We also acknowledge the Clinical Staff (Shelford Group chief nurses) as the source of the Safer Nursing Care Tool materials.
References
1. National Institute for Health and Care Excellence (GB). Safe staffing for nursing in adult inpatient wards in acute hospitals [Internet]. updated 2014, July 15. cited 2019, June 18. Available from: https://www.nice.org.uk/guidance/sg1.
2. Hoi SY, Ismail N, Ong LC, Kang J. Determining nurse staffing needs: the workload intensity measurement system. Journal of Nursing Management. 2010; 18:44–53. DOI: 10.1111/j.1365-2834.2009.01045.x.


3. Song KJ, Kim EH, Yoo CS, Park HA, Song MS, Park KO. Verification of reliability and validity of KPCS-1 and estimation of nursing time conversion index. Journal of Korean Clinical Nursing Research. 2010; 16(2):127–140.
4. National Health Insurance Service (KR). Standard guidelines for comprehensive nursing care service. Rev. 2017 ed. Wonju: National Health Insurance Service;2017.
5. Cho SH, Lee JY, June KJ, Hong KJ, Kim Y. Nurse staffing levels and proportion of hospitals and clinics meeting the legal standard for nurse staffing for 1996~2013. Journal of Korean Academy of Nursing Administration. 2016; 22(3):209–219. DOI: 10.11111/jkana.2016.22.3.209.

6. Smith S, Casey A, Hurst K, Fenton K, Scholefield H. Developing, testing and applying instruments for measuring rising dependency-acuity's impact on ward staffing and quality. International Journal of Health Care Quality Assurance. 2009; 22(1):30–39. DOI: 10.1108/09526860910927934.


7. Fenton K, Casey A. A tool to calculate safe nurse staffing levels. Nursing Times. 2015; 111(3):12–14.
8. The Shelford Group. Safer Nursing Care Tool implementation resource pack. Imperial Innovation Ltd;2018.
9. Hurst K. Ward workload and staffing data collection - general (acute nursing) pack. Hurst Research Ltd;2018.
10. Hurst K. UK ward design: Patient dependency, nursing workload, staffing and quality-An observational study. International Journal of Nursing Studies. 2008; 45(3):370–381. DOI: 10.1016/j.ijnurstu.2006.09.007.


11. Pelletier D, Duffield C. Work sampling: Valuable methodology to define nursing practice patterns. Nursing & Health Sciences. 2003; 5(1):31–38. DOI: 10.1046/j.1442-2018.2003.00132.x.


12. NHS National Services Scotland, Information Services Division. Nursing & midwifery workload and workforce planning programme [Internet]. Edinburgh: NHS National Services Scotland;cited 2019, June 18. Available from: https://www.isdscotland.org/Health-Topics/Workforce/Nursing-and-Midwifery/NMWWP/.
13. Hurst K, Smith A, Casey A, Fenton K, Scholefield H, Smith S. Calculating staffing requirements. Nursing Management (Harrow, London, England: 1994). 2008; 15(4):26–34. DOI: 10.7748/nm2008.07.15.4.26.c6616.
14. Hurst K. Gaming and up-coding. Nursing Management (Harrow, London, England: 1994). 2009; 15(9):19–23. DOI: 10.7748/nm2009.02.15.9.19.c6880.


15. The Shrewsbury and Telford Hospital NHS Trust. Nursing establishment review [Internet]. updated 2017, August. cited 2019, June 18. Available from: https://www.sath.nhs.uk/wp-content/uploads/2018/01/171130-11iv-Safer-Staffing-6-month-Nurse-Review.pdf.
16. Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees. Boca Raton, FL: Chapman and Hall/CRC;1984.
17. Jones CB, Finkler SA, Kovner CT, Mose JN. Financial management for nurse managers and executives. 5th ed. St. Louis, MO: Elsevier;2019.
18. Cho SH, Song KJ, Park IS, Kim YH, Kim MS, Gong DH, et al. Development of staffing levels for nursing personnel to provide inpatients with integrated nursing care. Journal of Korean Academy of Nursing Administration. 2017; 23(2):211–222. DOI: 10.11111/jkana.2017.23.2.211.

19. American Nurses Association. Optimal nurse staffing to improve quality of care and patient outcomes. Avalera Health;2015.
20. Cho SH, Kim YS, Yeon KN, You SJ, Lee ID. Effects of increasing nurse staffing on missed nursing care. International Nursing Review. 2015; 62(2):267–274. DOI: 10.1111/inr.12173.


21. Cho SH, Mark BA, Knafl G, Chang HE, Yoon HJ. Relationships between nurse staffing and patients' experiences, and the mediating effects of missed nursing care. Journal of Nursing Scholarship. 2017; 49(3):347–355. DOI: 10.1111/jnu.12292.


22. National Health Insurance Service(KR). 2019 Standard guidelines for comprehensive nursing care service [Internet]. Wonju: National Health Insurance Service;2019. updated 2019, July. cited 2019, August 2. Available from: https://www.nhis.or.kr/bbs7/boards/B0040/30288.
23. Tsutsui T, Tanaka A. Intensity of nursing care needs. 7th ed. Japanese Nursing Association Publishing Company;2018.
24. Hurst K. Selecting and applying methods for estimating the size and mix of nursing teams: a systematic review of the literature commissioned by the Department of Health. Leeds: Nuffield Institute for Health;2003.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download