Abstract
Chryseobacterium hominis is non-fermenting Gram-negative rod that was first identified as a novel species in 2007. Here, we report the first clinical case of C. hominis bacteremia, which was confirmed by MALDI-TOF MS and 16S rRNA gene sequencing. A 16-year-old boy diagnosed with acute lymphoblastic leukemia was hospitalized for three months. Two sets of blood culture test through a peripherally inserted central catheter (PICC), which was inserted a month ago, was performed when his white blood cell count declined and he had a high fever. Colonies of medium sizes that looked round, mucoid, sticky, and grayish on blood and chocolate agar plates were observed. Identification of bacteria using the VITEK MALDI-TOF MS system (BioMérieux, France) was not successful and the VITEK 2 system (BioMérieux, USA) indicated Sphingomonas paucimobilis, with a questionable level of confidence (92%). However, Microflex LT Biotyper (Bruker Daltonics, Germany) showed C. homins (log score: 1.81) and sequence of 16S rRNA showed a 100% identity with C. hominis. Piperacillin-tazobactam was administered since the isolate was susceptible to piperacillin-tazobactam but C. hominis showed growth in the next four follow-up culture of blood drawn through PICC. The fever subsided only after PICC was changed. The clinical prognosis and antimicrobial susceptibility test of C. hominis should be further studied.
Chryseobacterium hominis is an aerobic, non-motile, and non-fermenting gram-negative rod-shaped bacterium. C. hominis was first identified as a novel species in 2007 through clinical isolates biochemically similar to CDC groups II-h and II-c [1]. Here, we report the first clinical case of C. hominis bacteremia, which was confirmed by MALDI-TOF MS and 16S rRNA gene sequencing. This study was approved by the Institutional Review Board for Human Research, Yonsei University, Severance Hospital (4-2018-0685).
A 16-year-old boy diagnosed with acute lymphoblastic leukemia (ALL) six years ago was hospitalized for three months for conservative treatment. Suddenly, his white blood cell count showed a decline from a normal level to 2.20×109/L (neutrophils, 74.7%), at which time the patient's body temperature was 36.9–37.1℃. A few days later, the white blood cell count further decreased to 1.28×109/L (neutrophils, 71.9%), and the patient had a high fever over 38℃. Stenotrophomonas maltophilia was isolated from blood drawn by a peripherally inserted central catheter (PICC), which was implanted into the patient one month ago. Empirically, levofloxacin and piperacillin/tazobactam had been administered daily and trimethoprim/sulfamethoxazole had been administered for two days based on a chemotherapy regimen. S. maltophilia disappeared from the follow-up blood cultures after meropenem was administered instead of piperacillin/tazobactam. However, other medium-sized colonies that appeared round, mucoid, sticky, and grayish on a blood agar plate were observed in one of the two sets of blood culture samples. No observed growth on MacConkey agar led us to presume that bacteria were gram-positive. However, colonies of gram-negative bacilli that were catalase, oxidase, and indole positive were subsequently identified. Species identification using the VITEK MALDI-TOF MS system (BioMérieux, Marcy l'Etoile, France) was not successful; the VITEK 2 system (BioMérieux, Durham, NC, USA) indicated Sphingomonas paucimobilis, with a questionable level of confidence (92%). Microflex LT Biotyper (Bruker Daltonics, Leipzig, Germany) showed C. hominis (log score: 1.81). For confirmation, 721 base pairs of the 16S rRNA gene were sequenced, and the ezTaxon database (http://www. ezbiocloud.net/eztaxon) showed a 100% identity with C. hominis and a 97.46% identity with C. hagamense.
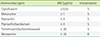
Antimicrobial susceptibility testing was performed using the VITEK 2 system AST-N225 card. According to the interpretive criteria of the Clinical and Laboratory Standards Institute M100, 27th ed. for non-Enterobacteriaceae [2], this isolate was susceptible to ciprofloxacin, minocycline, piperacillin, piperacillin-tazobactam, and trimethoprim-sulfamethoxazole, but resistant to meropenem (Table 1). It was susceptible to trimethoprim-sulfamethoxazole, but the drug failed at microbiological eradication. One of the reasons may be that trimethoprim-sulfamethoxazole was administered only for two days. As meropenem was administered instead of piperacillin-tazobactam, C. hominis showed growth in the next four follow-up culture of blood drawn through PICC. After replacing the patient's PICC, the culture tests of blood collected from venipuncture and the newly inserted PICC were all negative. His fever subsided shortly afterwards, and it took two weeks for the white blood cell count to reach normal levels. Finally, he was discharged three weeks later.
As there have been no clinical reports on C. hominis since it was listed as a novel species in 2007, its clinical significance has not been clearly established. However, some researchers have previously reported that Chryseobacterium spp. mainly infects newborns and immunocompromised hosts from all age groups [34]. In this case, C. hominis was repeatedly isolated from four blood samples drawn by PICC in a neutropenic ALL patient undergoing chemotherapy that included the administration of meropenem, to which the isolate was resistant. Although levofloxacin was administered daily, this isolate that is susceptible to ciprofloxacin was recovered repeatedly. Furthermore, the drug susceptibility study on Chryseobacterium spp. isolates reported that the most active antimicrobials were the newer quinolones, including levofloxacin [5]. In this case, C. hominis was an opportunistic pathogen causing a catheter-related blood stream infection, and its microbiological eradication was achieved after the PICC was removed.
In conclusion, we report a catheter-related blood stream infection case of C. hominis in an ALL patient. The identification of C. hominis by biochemical testing has limitations; however, it was readily identified and confirmed using MALDI-TOF MS and 16S rRNA sequencing in this study. The clinical prognosis and antimicrobial susceptibility testing of C. hominis should be further studied.
Figures and Tables
References
1. Vaneechoutte M, Kämpfer P, De Baere T, Avesani V, Janssens M, Wauters G. Chryseobacterium hominis sp. nov., to accommodate clinical isolates biochemically similar to CDC groups II-h and II-c. Int J Syst Evol Microbiol. 2007; 57:2623–2628.

2. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. CLSI supplement M100. 27th ed. Wayne, PA: Clinical and Laboratory Standards Institute;2017.
3. Bloch KC, Nadarajah R, Jacobs R. Chryseobacterium meningosepticum: an emerging pathogen among immunocompromised adults. Report of 6 cases and literature review. Medicine (Baltimore). 1997; 76:30–41.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download