INTRODUCTION
Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by arterial and venous thrombosis or pregnancy morbidity in patients with persistent antiphospholipid antibodies, such as anticardiolipin antibodies, lupus anticoagulant, and/or anti-ß2 glycoprotein-I antibodies.
1 APS can be suspected if any of the following occurs: fetal death at > 10 weeks, frequent miscarriages, severe preeclampsia, or a disease caused by an unknown origin of thrombus.
2 Nonthrombotic manifestations include thrombocytopenia, hemolytic anemia, cardiac valvular disease, livedo reticularis, and cognitive dysfunction.
3 The association of autoimmune disease with APS is well known, with systemic lupus erythematosus (SLE) being the most frequent disease associated with APS.
4
Meaningful results regarding the pathogenesis, clinical manifestations, treatment, and prevention of APS have been reported.
356 In 1990, the incidence and prevalence of APS were estimated approximately five new cases per 10
5 persons-years and 40–50 cases per 10
5 people, respectively.
7 Antiphospholipid antibodies have been also widely studied. Approximately 5% of the general population is expected to be positive for antiphospholipid antibodies; among healthy blood donors, 10% are positive for anticardiolipin antibody and 1% are positive for lupus anticoagulant.
89 Recently, a population-based research of 144,248 participants showed that during a 16-year study period, 33 incident cases were recorded and the annual incidence and estimated prevalence of APS were approximately two persons per 10
5 person-years and 50 per 10
5 people, respectively.
10 However, APS is a rare disease and needs to be studied in a large population. Till date, nationwide population-based epidemiology studies regarding APS are unavailable.
This research aims to conduct the first nationwide population-based study of prevalence, incidence, and related complications of APS based on the database of the National Health Insurance (NHI), which is a nationwide mandatory insurance scheme provided by the Korean government and covering more than 52 million Koreans.
DISCUSSION
This is the first nationwide population-based study of the incidence, prevalence, and related complications of APS based on HIRA data, which is a nationwide mandatory insurance scheme provided by the Korean government. Unlike a previous population-based study, our research showed that the incidence rate of APS differed according to gender and age groups. In secondary APS analysis, SLE was identified as the most relevant autoimmune disease, which was previously identified; however, it was observed that RA was also highly associated with secondary APS, particularly in men patients.
The Euro cohort (Euro-Phospholipid Project) and the Northwest Italian cohort (APS Piedmont Cohort) consisted of 1,000 and 274 diagnosed patients, respectively. They revealed various important clinical information through findings during the observation period along and past medical history. However, the cohort configuration itself had limitations in which selection biases are inevitable. Additionally, the Euro cohort, which is the largest cohort study, had diagnostic criteria as of 1999,
19 and 41.9% of patients were lost to follow-up, whereas the Italian cohort with 274 patients has yet to report further findings.
42021 These cohorts did not show general epidemiology on prevalence and incidence. Recently, a population-based study (Olmsted County study) of 144,248 participants showed that during the 16-year study period, 33 incident cases were recorded, and the annual incidence of APS was around two persons per 10
5 person-years, with an estimated prevalence of 50 per 10
5 people. However, patients with APS diagnoses were only few, and a specific area of the population was insufficient to analyze the overall epidemiology.
10 We analyzed the data of 3088 newly diagnosed patients with APS through the HIRA databases, which cover more than 52 million of Korean population, during the 9-year study period and showed the incidence and prevalence rates with other related clinical features (
Table 1).
Table 1
General characteristics and clinical manifestations in the Korean HIRA study in comparison with previous research
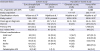
|
Characteristics |
Cohort study |
Population-based study |
|
Euro-phospholipid project |
APS piedmont cohort |
Olmsted county study |
Korea HIRA study |
|
No. of patients with APS |
1,000 |
217 |
33 |
3,088 |
|
Study population |
- |
- |
1.4 × 105
|
522.7 × 105
|
|
Classification criteria |
Wilson et al.19
|
Miyakis et al.1
|
Miyakis et al.1
|
Miyakis et al.1
|
|
Study period |
1999–2009 |
2012–present |
2000–2015 |
2008–2017 |
|
Mean age at diagnosis |
34 ± 13a
|
43.7 ± 15.3 |
54.2 ± 18.5 |
44.6 ± 16.6 |
|
Women |
820 (82) |
162 (74.7) |
18 (55) |
1,873 (60.7) |
|
Primary APS |
531 (53.1) |
115 (52.9) |
- |
1,766 (57) |
|
SLE-related APS |
362 (36.2) |
60 (27.6) |
6 (18) |
845 (27) |
|
Clinical manifestations |
|
|
|
|
|
Fetal lossb
|
83 (10.1) |
38 (23.5) |
3 (16.7) |
437 (23.3) |
|
DVT |
317 (31.7) |
81 (31.3) |
14 (42) |
619 (20.0) |
|
PTE |
90 (9.0) |
26 (12.0) |
13 (39) |
540 (17.5) |
|
Stroke |
131 (13.1) |
53 (24.4) |
11 (33) |
862 (27.9) |
|
TIA |
70 (7.0) |
- |
4 (12) |
|
Catastrophic APS |
9 (0.9)c
|
3 (1.3) |
- |
94 (3.0) |
The mean age at diagnosis was 44.6 ± 16.6 years, with 47.4 years for men and 42.8 years for women. The average age of diagnosis was lower than that in the Olmsted County study (54.2 vs. 44.6, respectively). The ratios of women in the two cohorts, namely, the Euro-Phospholipid Project and the APS Piedmont Cohort, were 82% and 74.7%, respectively. Meanwhile, such ratio in the population-based studies was relatively low in the Korean HIRA study (60.5%) and the Olmsted County study (55%). Therefore, selection biases were in cohort composition and indicated that more attention should be paid in men patients with APS.
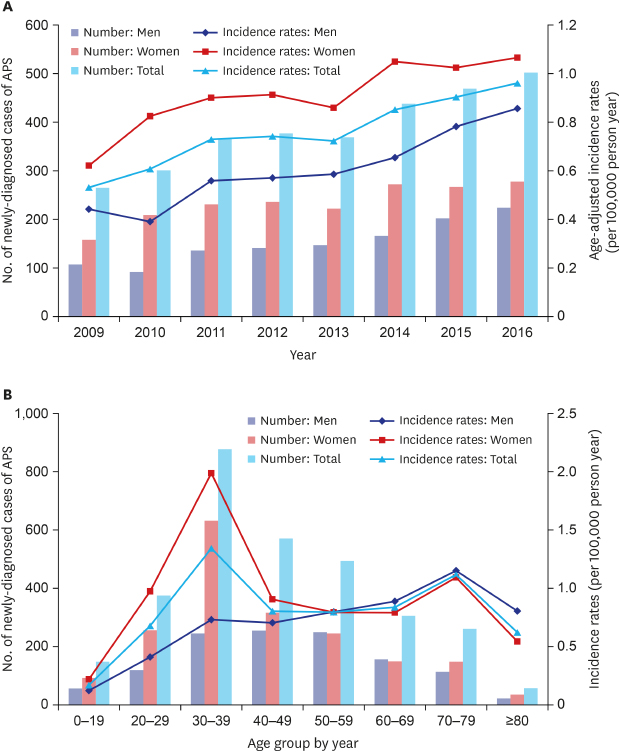
In the Olmsted County study, no difference in APS incidence rates by gender and no evidence of a differential age effect in men vs. women were found. However, in the current research, the incidence rates between men and women showed different patterns. Men showed peak incidence rates at 70–79 years old, while women revealed incidence peak at 30–39 years and at 70–79 years old. In men, the primary APS, secondary APS, and SLE-related APS incidence rates all showed a peak at 70–79 years old. In women, the primary APS incidence rate showed peaks at 30–39 years and at 70–79 years old, but both the secondary APS and SLE-related APS incidence rates showed a peak only at 30–39 years old. Unlike women, the incidence rate in men tended to increase with age at overall (
P trend < 0.001), primary APS (
P trend < 0.001), and secondary APS (
P trend < 0.001) (
Supplementary Tables 4,
5 and
Fig. 4). Considering that SLE was the most frequent autoimmune disease in secondary APS, the age group for both the peak incidences of SLE and secondary APS is the same.
22 In the epidemiology study of SLE in Korea, women demonstrated that the peak age of SLE incidence was at 30–39 years of age, which showed the same result in the current study; thus, the increase in SLE may be related to the increase in secondary APS in women.
23
Fig. 4
Age- and gender-adjusted incidence rate of primary, secondary, and systemic lupus erythematosus-related APS (per 105 person-year) by age group in Korean population during 2009–2016.
APS = antiphospholipid syndrome.

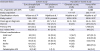
The incidence by year was 0.53 per 10
5 person-year in 2009 and increased to 0.97 per 10
5 person-year in 2016. However, the diagnosis rate increased rather than the number of patients. In 2008, 3,322 antiphospholipid antibody tests were performed, but in 2017, it increased annually to 17,341, which is more than fivefold (
Supplementary Fig. 2). Thus, physician's awareness and diagnostic efforts for APS have increased. The incidence rate in previous studies was relatively higher than that in the current study (Olmsted County study, 2 per 10
5 person-years vs. Korean HIRA study 0.75 per 10
5 person-year). However, studies investigating the actual incidence and prevalence of large populations, such as our research, are still unavailable. Another large-scale population-based study involving different ethnic group and regions is necessary.
The ratio of primary APS to secondary APS in men was approximately 2:1, but in women, it was 1:1.2; thus, secondary APS in women was higher than in men. In the secondary APS analysis, all autoimmune diseases were not mutually exclusive. SLE was the most common, but RA also showed a higher portion and was more in men than SLE. Other autoimmune diseases, except SLE and RA, were less than 8%. Among the autoimmune diseases, SLE (
P < 0.001), RA (
P = 0.026), Sjogren syndrome (
P = 0.002) and vasculitis (
P = 0.006) showed statistically different distribution according to gender. The prevalence of SLE and Sjogren syndrome higher in women, while that of RA and vasculitis was higher in men. DM and systemic sclerosis showed no statistically significant difference between men and women. RA can be overdiagnosed by physicians. In fact, increased cases of DVT and PTE in patients with RA were reported,
24 and only few studies regarding the association of RA with APS are available.
25 The reported prevalence of antiphospholipid antibodies in RA ranges from 5% to 75%, with a mean value of 28% and a median of 22%.
26 Therefore, apart from SLE, RA may be another major disease involved in the occurrence of APS.
For 1 year before and after the new diagnosis of APS, among 1,209 women with APS aged between 20 and 49 years, abortion and stillbirth codes were found in 437, with a fetal mortality rate of 14.2% (437/3088), which was higher than that in the Olmsted County study (9.1%). Fetal mortality relative to childbearing age in the women population was 36.1% (437/1209), but the definite fetal mortality may be higher because not all childbearing women are pregnant. In the Euro-Phospholipid Project, 1,580 cases of pregnancy in a total of 590 women had been recorded from symptoms onset until entry into the enrollment, of which 827 fetal deaths were reported, showing a high fetal mortality rate of 52.3%. In the case of preeclampsia and eclampsia, 82 out of 590 pregnant women were identified in the Euro-Phospholipid Project (8.2%); in the current study, 36 out of 1,209 childbearing-age women were found (1.2%), showing a relatively low rate. However, as with fetal mortality, the high actual incidence is expected. Such cases of high pregnancy morbidity and fetal loss emphasize the importance of early diagnosis and management of APS.
The Euro-Phospholipid Project reported that the incidence of newly identified CAPS during the 10-year observation period was approximately 1%,
4 but it was higher in our study (3%). In the Euro-Phospholipid Project, the patients died with CAPS who could not be registered, and 41.9% of the patients were lost to follow-up. Given that patients maintain regular medical follow-ups with preventive anticoagulants (77%) after the diagnosis, the incidence may lower than it actually is. In this study, thrombotic manifestations, namely, DVT and PTE, were 20% and 17.4%, respectively. Furthermore, all three studies have various differences. Stroke and TIA were identified in 28% of patients, and the highest incidence rate was reported in the Olmsted County study with the highest average diagnostic age.
The study has the strength of being the first nationwide population-based study with more than 52 million people, but some limitations were noted. First, the diagnostic codes, which were assigned by the health care providers, might not be entirely accurate. The results of antiphospholipid antibody test, imaging, and clinical manifestations were not available to the researchers. However, we used RID registration program with strict diagnostic conditions, and also attempted to overcome these limitations through the operational definition of at least two identical APS antibody tests and the use of anticoagulants for a long period of time. Second, the incidence of APS can differ according to the incidence of autoimmune diseases by region or ethnic groups. Especially, SLE is common in APS, and it showed various incidence rates across the world (0.3–23.2 per 10
5 person-years).
27 Therefore, the results of this study may not generalize all population groups.
Unlike a previous population-based study, the incidence of APS differed according to age groups and gender. The incidence of primary APS was higher than that of secondary APS in both gender. Furthermore, as already reported, secondary APS is highly associated with SLE; however, we observed that RA is also highly related. The findings of this study may help physicians understand the nature of epidemiology and the burden of APS.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download