1. Shin WG, Lee SW, Baik GH, Huh KC, Lee SI, Chung JW, et al. Eradication rates of
Helicobacter pylori in Korea over the past 10 years and correlation of the amount of antibiotics use: nationwide survey. Helicobacter. 2016; 21(4):266–278.

2. Kim JS, Kim BW, Hong SJ, Kim JI, Shim KN, Kim JH, et al. Sequential therapy versus triple therapy for the first line treatment of
Helicobacter pylori in Korea: a nationwide randomized trial. Gut Liver. 2016; 10(4):556–561.


3. Lee SW, Kim HJ, Kim JG. Treatment of
Helicobacter pylori infection in Korea: a systematic review and meta-analysis. J Korean Med Sci. 2015; 30(8):1001–1009.


4. Kim SG, Jung HK, Lee HL, Jang JY, Lee H, Kim CG, et al. Guidelines for the diagnosis and treatment of
Helicobacter pylori infection in Korea, 2013 revised edition. Korean J Gastroenterol. 2013; 62(1):3–26.

5. Yuan Y, Ford AC, Khan KJ, Gisbert JP, Forman D, Leontiadis GI, et al. Optimum duration of regimens for Helicobacter pylori eradication. Cochrane Database Syst Rev. 2013; (12):CD008337.
6. Bielański W, Konturek SJ. New approach to 13C-urea breath test: capsule-based modification with low-dose of 13C-urea in the diagnosis of
Helicobacter pylori infection. J Physiol Pharmacol. 1996; 47(3):545–553.

7. Kim BG, Lee DH, Ye BD, Lee KH, Kim BW, Kim SG, et al. Comparison of 7-day and 14-day proton pump inhibitor-containing triple therapy for
Helicobacter pylori eradication: neither treatment duration provides acceptable eradication rate in Korea. Helicobacter. 2007; 12(1):31–35.

8. Jung YS, Kim EH, Park CH. Systematic review with meta-analysis: the efficacy of vonoprazan-based triple therapy on
Helicobacter pylori eradication. Aliment Pharmacol Ther. 2017; 46(2):106–114.

9. Chen YI, Fallone CA. A 14-day course of triple therapy is superior to a 10-day course for the eradication of Helicobacter pylori: a Canadian study conducted in a ‘real world’ setting. Can J Gastroenterol Hepatol. 2015; 29(8):e7–10.
10. Lee JW, Kim N, Kim JM, Nam RH, Chang H, Kim JY, et al. Prevalence of primary and secondary antimicrobial resistance of
Helicobacter pylori in Korea from 2003 through 2012. Helicobacter. 2013; 18(3):206–214.

11. Lee JY, Kim N. Future trends of
Helicobacter pylori eradication therapy in Korea. Korean J Gastroenterol. 2014; 63(3):158–170.

12. Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of
Helicobacter pylori infection. Am J Gastroenterol. 2017; 112(2):212–239.

13. Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, Axon AT, et al. Management of
Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017; 66(1):6–30.

14. Graham DY, Lee SY. How to effectively use bismuth quadruple therapy: the good, the bad, and the ugly. Gastroenterol Clin North Am. 2015; 44(3):537–563.


15. Malfertheiner P, Megraud F, O'Morain CA, Atherton J, Axon AT, Bazzoli F, et al. Management of
Helicobacter pylori infection--the Maastricht IV/ Florence Consensus Report. Gut. 2012; 61(5):646–664.

16. Fuccio L, Minardi ME, Zagari RM, Grilli D, Magrini N, Bazzoli F. Meta-analysis: duration of first-line proton-pump inhibitor based triple therapy for
Helicobacter pylori eradication. Ann Intern Med. 2007; 147(8):553–562.

17. Yoon K, Kim N, Nam RH, Suh JH, Lee S, Kim JM, et al. Ultimate eradication rate of
Helicobacter pylori after first, second, or third-line therapy in Korea. J Gastroenterol Hepatol. 2015; 30(3):490–495.

18. Munteanu D, Etzion O, Ben-Yakov G, Halperin D, Eidelman L, Schwartz D, et al. Efficacy and safety of sequential versus quadruple therapy as second-line treatment for Helicobacter pylori infection-A randomized controlled trial. PLoS One. 2017; 12(9):e0183302.
19. Kim SB, Lee SH, Kim KO, Jang BI, Kim TN. Ten-day sequential therapy versus bismuth based quadruple therapy as second line treatment for
Helicobacter pylori infection. Korean J Gastroenterol. 2015; 66(5):261–267.

20. Chung JW, Lee JH, Jung HY, Yun SC, Oh TH, Choi KD, et al. Second-line
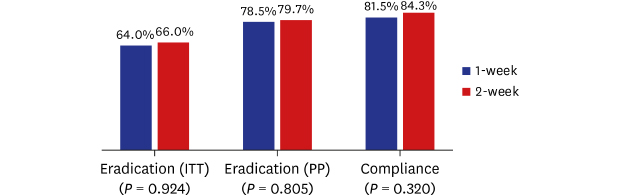
Helicobacter pylori eradication: a randomized comparison of 1-week or 2-week bismuth-containing quadruple therapy. Helicobacter. 2011; 16(4):289–294.

21. Lee BH, Kim N, Hwang TJ, Lee SH, Park YS, Hwang JH, et al. Bismuth-containing quadruple therapy as second-line treatment for
Helicobacter pylori infection: effect of treatment duration and antibiotic resistance on the eradication rate in Korea. Helicobacter. 2010; 15(1):38–45.

22. Yoon JH, Baik GH, Kim YS, Suk KT, Shin WG, Kim KH, et al. Comparison of the eradication rate between 1- and 2-week bismuth-containing quadruple rescue therapies for
Helicobacter pylori eradication. Gut Liver. 2012; 6(4):434–439.


23. Chung JW, Jung YK, Kim YJ, Kwon KA, Kim JH, Lee JJ, et al. Ten-day sequential versus triple therapy for
Helicobacter pylori eradication: a prospective, open-label, randomized trial. J Gastroenterol Hepatol. 2012; 27(11):1675–1680.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download