Abstract
Purpose
We sought to compare the efficacy as well as the safety of two maximum medical therapy combinations applied to lower the intraocular pressure (IOP) in different primary open-angle glaucoma (POAG) age groups.
Methods
This was a retrospective, consecutive case series study that included 60 eyes of 60 subjects with POAG, specifically 20 subjects aged 40 to 54 years, 21 aged 55 to 69 years, and 19 aged 70 years or older. All had been treated for at least 12 months with triple maximum medical therapy (TMT; dorzolamide/timolol, brimonidine, and latanoprost) to lower their IOP, which subsequently was changed to double maximum medical therapy (DMT, fixed drug combinations of tafluprost/timolol and brinzolamide/brimonidine). The rate of IOP change and adverse drug reactions were compared amongst the three age groups.
Results
The mean IOP change at three months after converting from TMT to DMT was −0.65 ± 1.42 mmHg (−3.84% ± 9.31%) among the overall study group, but this finding was not statistically significant (p = 0.108). In the 40 to 54 years and 55 to 69 years groups, the mean IOP change rates were +0.29 ± 0.96 mmHg (+2.40% ± 6.85%, p = 0.087) and −0.50 ± 0.99 mmHg (−3.05% ± 6.40%, p = 0.084) respectively. In the 70 years or older group, the mean IOP change, interestingly, was −1.80 ± 1.46 mmHg (−11.29% ± 9.31%, p < 0.001) and nine (47.4%) of the 19 subjects showed additional IOP reductions of 10% or more after converting from TMT to DMT. In all three age groups, the incidence rate of dry eye was significantly lower for DMT than for TMT (p = 0.031).
Glaucoma is a leading cause of blindness globally. Intraocular pressure (IOP) currently is the only factor proven to prevent or reduce the risk of development and/or progression of glaucoma [1]. Several previous studies have shown the importance of IOP lowering to the reduction of glaucoma progression risk [234].
The standard first-line therapy for IOP-lowering is the administration of topical ocular hypotensive medications [5]. Typically, the initial treatment is monotherapy. If the first-choice drug proves ineffective or if adverse effects are seen, the regimen is altered. In cases where the target IOP is not reached, switching to another monotherapy is an option [6]. However, if, after switching, the target IOP still cannot be reached, a different class of ocular hypotensive medication should be added [478]. As many patients must continue with topical medication for long durations of time, often for the rest of their lives, it is important to elucidate the combinations of ocular hypotensive medications that best reconcile maximal therapeutic efficacy with minimal adverse drug reactions (ADRs).
Many types of fixed drug combinations (FDCs) are currently available. FDC treatment entails the administration of two drugs in one bottle, with the chief advantage of this being the simplicity and convenience of the dosing regimen [910]. The introduction of various FDCs has led to changes in drug prescription patterns and increased numbers of possible drug combinations. Especially in patients who need maximum medical therapy, FDCs have advantages over multidrop or multi-bottle regimens in terms of patient convenience and adherence without any great sacrifice of the additive effects of the unfixed combinations.
This study's purpose was to compare the efficacy as well as the safety of two maximum medical therapy combinations for lowering the IOP in primary open-angle glaucoma (POAG) patients stratified by age.
The institutional review board of Seoul National University Hospital approved (1909-119-1066). this cross-sectional study, which adhered faithfully to the tenets of the Declaration of Helsinki. Informed consent was waived due to the study's retrospective nature.
Eligible-patient data were enrolled from the Seoul National University Hospital Web database and CDW SUPREME (compiled between January 2016 and August 2019). These retrospectively reviewed electronic medical records were those of POAG patients who had visited the Seoul National University Hospital's glaucoma clinic for regular check-ups and who had an antiglaucoma medication treatment history of using two different maximum medical therapy regimens.
All of the subjects underwent a complete ophthalmic examination, including a best-corrected visual acuity assessment, refraction, slit-lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry (Haag-Streit, Koniz, Switzerland), and dilated stereoscopic optic disc examination. Additionally, central corneal thickness measurements (Orbscan 73 II; Bausch & Lomb, Rochester, NY, USA), stereo disc photography, red-free retinal nerve fiber layer photography, Cirrus HD-OCT imaging (Carl Zeiss Meditec, Dublin, CA, USA), and central 24-2 threshold testing via the Humphrey visual field (VF) analyzer (HFA II; Humphrey Instruments, Dublin, CA, USA) were undertaken.
Our clinical maximum medical therapy protocol for lowering of IOP entails triple maximum medical therapy (TMT; dorzolamide/timolol, brimonidine, and latanoprost) or double maximum medical therapy (DMT, tafluprost/timolol and brinzolamide/brimonidine). Patients eligible for inclusion in this study were those who met the following criteria: (1) POAG on TMT for at least 12 months; (2) stable IOP for the three most recent months of TMT (in other words, in all cases, the IOP had been lowered by 20% or more from the untreated IOP and maintained at this point without any subsequent laser or surgical glaucoma treatments); and (3) at least nine months of follow-up following conversion to DMT. Conversely, the exclusion criteria were (1) a history of intraocular surgery (including cataract surgery that had been performed during the present study's time period), (2) eyes showing any other active ocular pathology, (3) any uncontrolled systemic disease, and (4) usage of topical and/or oral medications possibly affecting IOP (e.g., steroids) over the course of the current study.
The diagnosis of POAG was based on the appearance of the optic disc (localized or diffuse neuroretinal rim thinning/notching) on stereo disc photography with retinal nerve fiber layer defect in the corresponding region (based on red-free fundus imaging), an open angle as confirmed by gonioscopic examination, and the presence of glaucomatous VF defect. Glaucomatous VF defects were defined as follows: (1) a cluster of three points having probabilities of less than 5% in at least one hemifield on a pattern deviation map, including at least one point having a probability of less than 1% or a cluster of two points having a probability of less than 1%; (2) glaucomatous hemifield test results that were outside the normal limits; and (3) a pattern standard deviation of more than 95% of the normal limits, as conf irmed by at least two reliable examinations (false-positives/negatives <15%, fixation losses <15%). If both eyes of a single patient were eligible, one was chosen randomly.
Details on the antiglaucoma eye drops used in this study—namely, the concentrations, the preservatives, and the manufacturer names—are as follows: latanoprost/0.005%/benzalkonium chloride (BAK)/Xalatan (Pfizer, New York, NY, USA); brimonidine/0.15%/purite/Alphagan P (Allergan, Dublin, Ireland); dorzolamide/timolol FCD/2%,0.5%/BAK/Cosopt (Santen Pharmaceuticals, Osaka, Japan) for TMT; tafluprost/timolol FCD/0.0015%/BAK/Tapcom (Santen Pharmaceuticals, Osaka, Japan); and brinzolamide/brimonidine FCD/1%, 0.2%/BAK/Simbrinza (Alcon, Geneva, Switzerland) for DMT.
Patients administered latanoprost or tafluprost/timolol were instructed to instill one drop of latanoprost or tafluprost/timolol once per day at 8 p.m. Patients receiving brimonidine, a dorzolamide/timolol FDC, or a brinzolamide/brimonidine FDC were instructed to instill one drop of brimonidine, dorzolamide/timolol FDC, or brinzolamide/brimonidine FDC twice per day at 8 a.m. and 8 p.m. Thus, with the TMT and DMT protocols, the total numbers of antiglaucoma eye drops administered were five and three, respectively.
Most of the study subjects had used at least one topical antiglaucoma medication before starting TMT. For all of the patients, TMT was changed to DMT without any washout period between the two regimens.
Goldmann applanation tonometry was used to measure IOP at baseline and during every follow-up visit thereafter. The collected IOP measurements were compared between the two regimens at one, three, and six months before the conversion to DMT and at one, three, and six months after the conversion.
Clinical signs of conjunctival hyperemia were determined based on reference photographs (Contact Lens Research Unit grading scales). Another ADR sign, dry eye, was defined as follows: mild to moderate dry eye corresponded to a dry eye severity level of 1 or greater, as suggested by both the Delphi Panel Consensus for Dry Eye Management and the International Dry Eye Workshop. Allergic conjunctivitis associated with antiglaucoma medications was diagnosed based on clinical symptoms and signs including pruritus, conjunctival injection, follicular conjunctival reaction, contact dermatitis of the eyelids, and eyelid swelling. Other side effects such as eye irritation, blurred vision, foreign body sensation, or symptoms of dry mouth were subjectively assessed and reported by each patient.
The three age groups' normally distributed demographic and clinical characteristics were compared by one-way analysis of variance with Tukey's post-hoc test. Categorical data were analyzed using either Fisher's exact test or McNemar's test. Each group's IOPs with TMT and DMT were compared by paired t-test. In each analysis, either parametric or nonparametric tests were employed according to the results of a normality test. Statistical analyses were performed using the IBM SPSS Statistics ver. 22.0 (IBM Corp., Armonk, NY, USA). A two-tailed p-value of less than 0.05 was considered to represent statistical significance.
During the study period from January 2016 to August 2019, a total of 68 patients met all of the inclusion criteria. Among those, six patients were excluded due to cataract surgery performed during the study's follow-up period, leaving a final cohort of 60 POAG patients (60 eyes).
The age groups' demographics and clinical characteristics are compared in Table 1. There were no significant intergroup differences regarding sex distribution, follow-up duration, or systemic factors (e.g., diabetes mellitus, hypertension). Likewise, there were no significant spherical equivalent, central corneal thickness, or baseline VF mean deviation variations either.
With TMT, the mean IOP for the most recent three months was 15.3 ± 2.02 mmHg, while, with DMT, it was lower, albeit only slightly and insignificantly so (14.7 ± 2.04 mmHg, p = 0.108). Fig. 1 compares the IOP measurements between TMT and DMT during the follow-up period.
A subgroup analysis was performed to assess any possible differences related to age. The recruited subjects' ages ranged from 40 to 83 years, and they were divided so that the age intervals were similar among the groups as follows: group 1 (age, 40–54 years), group 2 (age, 55–69 years), and group 3 (age, ≥70 years). Table 2 compares the three age groups' IOP variables between TMT and DMT. In the 40 to 54 years group (n = 20), the mean IOP change at three months after conversion from TMT to DMT was +0.29 ± 0.96 mmHg (+2.40% ± 6.85%), while in the 55 to 69 years group (n = 21), it was −0.50 ± 0.99 mmHg (−3.05% ± 6.40%), with neither of these findings being statistically significant (p = 0.087 and p = 0.084). In the 70 years or older group (n = 19), the mean IOP change, interestingly, was −1.80 ± 1.46 mmHg (−11.29% ± 9.31%, p < 0.001), with nine (47.4%) of the 19 subjects showing additional IOP reductions of 10% or more after conversion to DMT.
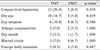
The ADRs reported for each treatment are provided in Table 3. As is apparent, there were no serious ADRs encountered in this study. Dry eye occurred significantly less frequently with DMT (4 patients, 6.7%) than with TMT (10 patients, 16.7%; p = 0.031).
In our results, the mean IOPs for the TMT and DMT regimens were statistically equivalent. The data obtained from the subgroup analysis indicated that the mean rate of IOP change after converting from TMT to DMT was not statistically significant in either the 40 to 54 years or the 55 to 69 years groups. In the 70 years or older group, however, the mean IOP, interestingly, was significantly lower with DMT than with TMT.
Although both of the regimens—that is, TMT and DMT—entailed maximum medical therapy, their different constituents should be taken into account. TMT consisted of latanoprost, brimonidine, dorzolamide, and timolol, while DMT included taf luprost, brimonidine, brinzolamide, and timolol. However, according to previous reports, 2% dorzolamide and 1% brinzolamide share similar IOP-lowering efficacies [11], and those of 0.005% latanoprost and 0.0015% tafluprost are comparable as well [121314]. Suzuki et al. [15] reported randomized controlled study results comparing the efficacy and safety of a tafluprost/timolol fixed combination and a latanoprost/timolol fixed combination. In their study, there were no significant differences observed between the two groups in terms of IOP, superficial punctate keratopathy score, tear breakup time, or hyperemia score after 12 weeks. However, eye irritation and eye pain were significantly decreased in the tafluprost/timolol group when compared with in the latanoprost/timolol group. Additionally, the capacity difference between brimonidine-purite 0.15% and brimonidine 0.2% should be considered. Previous studies have shown comparable IOP-lowering efficacies of brimonidine-purite 0.15% and brimonidine 0.2% over the course of three to 12 months both in glaucoma and ocular hypertension [161718]. Therefore, the IOP-lowering efficacies of TMT and DMT would be expected to be similar too and, in fact, our present results indicated equivalent IOP-lowering efficacies between TMT and DMT for the 60 POAG patients studied.
Joh and Jin [19] analyzed two different combinations of maximum medical therapy for lowering the IOP administered in 82 POAG subjects. Specifically, they compared the IOP-lowering efficacies between a TMT group including patients who were treated with tafluprost, brimonidine, and a brinzolamide/timolol FDC and a DMT group including patients who were treated with a tafluprost/timolol FDC and a brinzolamide/brimonidine FDC, respectively. Thus, in their study, the active ingredients of the medications were identical in the two groups, and the differences were the capacity of brimonidine and the type of preservative. They demonstrated that the two regimens' IOP reduction rates were statistically equivalent but that the incidence rates of conjunctival hyperemia and dry eye were signif icantly lower in the DMT group during the 12 months of follow-up. In the current study as well, we found similar IOP-lowering efficacies between the two different maximum medical therapies and a lower incidence of dry eye with DMT in POAG patients whose regimen had been switched from TMT to DMT.
According to the subgroup analysis, with DMT, the mean IOP was significantly lower, especially in the elderly (≥70 years) group. Age-related physical or mental conditions can have adverse effects on adherence to daily topical medication regimens [20]. Winfield et al. [21] reported a high noncompliance prevalence compounded by an inability among older patients to properly instill eye drops. Patients older than 60 years of age relative to younger patients have been found to experience greater difficulty with the physical application of eye drops, to more frequently require additional assistance, and to encounter increased difficulty with remembering to apply eye drops [22]. In this respect, too, it is known that the frequency of dosing is inversely correlated with medication adherence [23]. In the current study, the total numbers of instilled antiglaucoma eye drops for TMT and DMT were five and three, respectively. From this point of view, improved medication compliance could make DMT's IOP-lowering efficacies better than TMT's among elderly patients.
The differences in pH levels and preservative composition between the two regimens could be other factors affecting both patient compliance and IOP-lowering efficacies. DMT presents a more physiological pH than TMT (6.5–7.2 vs. 5.8–7.4) [24], and the impact of physiological pH on compliance has previously been reported [2526]. In terms of preservative composition, TMT contains purite as well as BAK, whereas DMT includes only BAK. However, since purite has been reported to improve safety and tolerability relative to BAK [2728], the differences due to preservatives between the two groups are not considered to be significant. In light of these facts, further investigation of the pH levels or preservative compositions of antiglaucoma medications and their associations with patient compliance and IOP-lowering effects is warranted.
There are several limitations to our study that should be considered. First, the study subjects maintained the TMT regimen for longer than 12 months, whereas the DMT regimen was followed for only a minimum of nine months. Although with DMT, we observed a significantly lower frequency of ADRs (e.g., dry eye), the significant difference in treatment duration might have affected the ADR-frequency results. Additionally, although the absence of a washout period between the two regimens reflected a real-world clinical setting, the remaining IOP-lowering effects of TMT might have affected the IOP during the DMT regimen. Second, while we suggested “compliance” as one of the factors supporting DMT's better IOP-lowering effect relative to TMT in older age, we did not objectively compare or assess the compliance level in each patient. Further studies assessing compliance level with structured questionnaires or interviews should be conducted to more thoroughly investigate the effects of medication-regimen simplification for elderly patients. Third, our study population was limited to subjects aged older than 40 years, so caution needs to be exercised in any attempts to generalize our results to younger age groups. Fourth, patients who had changed their regimen from TMT to DMT owing to poor IOP control were not included in the final analysis. The rationale for the regimen change in most of our cases was reduced dosing and thus improved patient convenience. These factors could have affected the difference in the degree of IOP reduction between TMT and DMT. Fifth and finally, the follow-up period was somewhat short. Future studies with longer follow-up periods are needed for more thorough comparisons of the two regimens' long-term IOP-lowering efficacies.
In conclusion, DMT relative to TMT was shown to be an effective and safe maximum medical therapy for lowering of IOP in POAG patients, especially in elderly patients. This suggests, albeit tentatively, a possibility of that the simplification of drug administration may improve adherence in elderly patients.
Figures and Tables
 | Fig. 1Graph depicting changes in intraocular pressure (IOP) during triple maximum medical therapy (TMT) and double maximum medical therapy (DMT). IOPs were compared between the two regimens at one, three, and six months before the conversion to DMT and one, three, and six months after the conversion in each age group. Note that the X-axis is not to scale but does depict the times at which the IOPs were measured. The Y error bars indicate the standard deviation of the mean. |
References
1. European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 3: Treatment principles and options Supported by the EGS Foundation: Part 1: Foreword; Introduction; Glossary; Chapter 3 Treatment principles and options. Br J Ophthalmol. 2017; 101:130–195.


2. The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000; 130:429–440.

3. Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003; 121:48–56.

4. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120:701–713.

5. Friedman DS, Nordstrom B, Mozaffari E, Quigley HA. Variations in treatment among adult-onset open-angle glaucoma patients. Ophthalmology. 2005; 112:1494–1499.


6. Webers CA, Beckers HJ, Nuijts RM, Schouten JS. Pharmacological management of primary open-angle glaucoma: second-line options and beyond. Drugs Aging. 2008; 25:729–759.

7. Quigley HA, Enger C, Katz J, et al. Risk factors for the development of glaucomatous visual field loss in ocular hypertension. Arch Ophthalmol. 1994; 112:644–649.


8. Inoue K, Ishida K, Tomita G. Effectiveness and safety of switching from prostaglandin analog monotherapy to prostaglandin/timolol fixed combination therapy or adding ripasudil. Jpn J Ophthalmol. 2018; 62:508–516.


9. Barnebey HS, Orengo-Nania S, Flowers BE, et al. The safety and efficacy of travoprost 0.004%/timolol 0.5% fixed combination ophthalmic solution. Am J Ophthalmol. 2005; 140:1–7.


10. Lee AJ, McCluskey P. Fixed combination of topical brimonidine 0.2% and timolol 0.5% for glaucoma and uncontrolled intraocular pressure. Clin Ophthalmol. 2008; 2:545–555.



11. Seong GJ, Lee SC, Lee JH, et al. Comparisons of intraocular-pressure- lowering efficacy and side effects of 2% dorzolamide and 1% brinzolamide. Ophthalmologica. 2001; 215:188–191.


12. Uusitalo H, Pillunat LE, Ropo A. Phase III Study Investigators. Efficacy and safety of tafluprost 0.0015% versus latanoprost 0.005% eye drops in open-angle glaucoma and ocular hypertension: 24-month results of a randomized, double-masked phase III study. Acta Ophthalmol. 2010; 88:12–19.


13. Uusitalo H, Egorov E, Kaarniranta K, et al. Benefits of switching from latanoprost to preservative-free tafluprost eye drops: a meta-analysis of two Phase IIIb clinical trials. Clin Ophthalmol. 2016; 10:445–454.



14. Ikeda Y, Mori K, Tada K, et al. Comparison study of intraocular pressure reduction efficacy and safety between latanoprost and taf luprost in Japanese with normal-tension glaucoma. Clin Ophthalmol. 2016; 10:1633–1637.


15. Suzuki K, Otsuka N, Hizaki H, et al. Multicenter, randomized, controlled study comparing tafluprost/timolol fixed combination with latanoprost/timolol fixed combination in primary open-angle glaucoma and ocular hypertension. Adv Ther. 2018; 35:796–808.


16. Mundorf T, Williams R, Whitcup S, et al. A 3-month comparison of efficacy and safety of brimonidine-purite 0.15% and brimonidine 0.2% in patients with glaucoma or ocular hypertension. J Ocul Pharmacol Ther. 2003; 19:37–44.


17. Kim CY, Hong S, Seong GJ. Brimonidine 0.2% versus brimonidine Purite 0.15% in Asian ocular hypertension. J Ocul Pharmacol Ther. 2007; 23:481–486.


18. Katz LJ. Twelve-month evaluation of brimonidine-purite versus brimonidine in patients with glaucoma or ocular hypertension. J Glaucoma. 2002; 11:119–126.

19. Joh HJ, Jin SW. Comparison of different combinations of maximum medical therapy for lowering intraocular pressure in primary open angle glaucoma: 12-month retrospective consecutive case series. Jpn J Ophthalmol. 2019; 63:322–327.


20. Broadway DC, Cate H. Pharmacotherapy and adherence issues in treating elderly patients with glaucoma. Drugs Aging. 2015; 32:569–581.


21. Winfield AJ, Jessiman D, Williams A, Esakowitz L. A study of the causes of non-compliance by patients prescribed eyedrops. Br J Ophthalmol. 1990; 74:477–480.



22. Lacey J, Cate H, Broadway DC. Barriers to adherence with glaucoma medications: a qualitative research study. Eye (Lond). 2009; 23:924–932.


23. Jin H, Kim Y, Rhie SJ. Factors affecting medication adherence in elderly people. Patient Prefer Adherence. 2016; 10:2117–2125.



24. Lockington D, Macdonald EC, Stewart P, et al. Free radicals and the pH of topical glaucoma medications: a lifetime of ocular chemical injury? Eye (Lond). 2012; 26:734–741.



25. Manni G, Denis P, Chew P, et al. The safety and efficacy of brinzolamide 1%/timolol 0.5% fixed combination versus dorzolamide 2%/timolol 0.5% in patients with open-angle glaucoma or ocular hypertension. J Glaucoma. 2009; 18:293–300.


26. Mundorf TK, Rauchman SH, Williams RD, et al. A patient preference comparison of Azarga (brinzolamide/timolol fixed combination) vs Cosopt (dorzolamide/timolol fixed combination) in patients with open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2008; 2:623–628.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download