Abstract
Background and Purpose
Methods
Results
Conclusions
Figures and Tables
Fig. 1
Predicted symptom profiles of K-PDSS-2 item responses for the sleep-disturbance subtypes based on latent class analysis. K-PDSS-2: Korean version of Parkinson's Disease Sleep Scale-2, PD: Parkinson's disease.
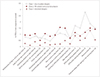
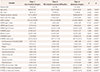
Table 3
Convergent validity of K-PDSS-2 with other motor and nonmotor measurements and patient-perceived quality of life

Data are mean±standard deviation values.
*p<0.05. p values are from the Spearman correlation test.
K-MADRS: Korean version of the Montgomery-Åsberg Depression Rating Scale, K-MMSE: Korean version of the Mini-Mental State Examination, K-NMSS: Korean version of the Non-Motor Symptoms Scale, K-PDQ-39: Korean version of the 39-item Parkinson's Disease Questionnaire, K-PDSS-2: Korean version of Parkinson's Disease Sleep Scale-2, MoCA-K: Korean version of the Montreal Cognitive Assessment, rs: Spearman rank-order correlation coefficient, UPDRS: Unified Parkinson's Disease Rating Scale.
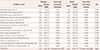
Table 5
Demographics and clinical characteristics of study patients in three sleep-disturbance-related latent classes
Data are n (%) or mean±standard deviation values. p values are from the chi-square test or the Kruskal-Wallis test followed by post-hoc comparisons with Bonferroni-corrected Mann-Whitney tests.
*Significant difference between classes 1 and 3, †Significant difference between classes 1 and 2, ‡Significant difference between classes 2 and 3. K-MADRS: Korean version of the Montgomery-Åsberg Depression Rating Scale, K-MMSE: Korean version of the Mini-Mental State Examination, K-NMSS: Korean version of the Non-Motor Symptoms Scale, K-PDQ-39: Korean version of the 39-item Parkinson's Disease Questionnaire, K-PDSS-2: Korean version of Parkinson's Disease Sleep Scale-2, LEDD: levodopa equivalent daily dosage, MoCA-K: Korean version of the Montreal Cognitive Assessment, PD: Parkinson's disease, UPDRS: Unified Parkinson's Disease Rating Scale.
Acknowledgements
Notes
Author Contributions
Conceptualization: Seong-Beom Koh, Joong-Seok Kim, Sang Jin Kim, Sang-Myung Cheon, Tae-Beom Ahn, Han-Joon Kim, Hui-Jun Yang.
Data curation: Sang Jin Kim, Han-Joon Kim, Hui-Jun Yang.
Formal analysis: Han-Joon Kim, Hui-Jun Yang.
Investigation: Seong-Beom Koh, Joong-Seok Kim, Sang Jin Kim, Tae-Beom Ahn, Sang-Myung Cheon, Han-Joon Kim, Jin Whan Cho, Yoon-Joong Kim, Hyeo-Il Ma, Mee Young Park, Jong Sam Baik, Phil Hyu Lee, Sun Ju Chung, Jong-Min Kim, In-Uk Song, Ji-Young Kim, Young-Hee Sung, Do Young Kwon, Jae-Hyeok Lee, Jee-Young Lee, Ji Seon Kim, Ji Young Yun, Hee Jin Kim, Jin Youg Hong, Mi-Jung Kim, Jinyoung Youn, Ji Sun Kim, Eung Seok Oh, Won Tae Yoon, Sooyeoun You, Kyum-Yil Kwon, Hyung-Eun Park, Su-Yun Lee, Younsoo Kim, Hui-Jun Yang, Hee-Tae Kim.
Methodology: Seong-Beom Koh, Joong-Seok Kim, Sang Jin Kim, Sang-Myung Cheon, Tae-Beom Ahn.
Project administration: Seong-Beom Koh, Joong-Seok Kim, Sang Jin Kim, Sang-Myung Cheon, Tae-Beom Ahn.
Software: Han-Joon Kim, Hui-Jun Yang.
Writing—original draft: Han-Joon Kim, Hui-Jun Yang.
Writing—review & editing: Sang Jin Kim.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download