INTRODUCTION
Considerable advances in antiepileptic drug treatment have been made since the 1990s thanks to the development of new-generation antiepileptic drugs with minimal adverse effects. Lamotrigine [LTG; 3,5-diamino-6(2,3-dichlorophenyl)-1,2,4-triazine] has a structure different from those of classical antiepileptic drugs and works by inhibiting the excessive release of the excitatory transmitter glutamate in the central nervous system.
1 LTG is known to have fewer side effects than other anticonvulsive agents, making it more reliable. Several clinical reports have described the effectiveness and safety of LTG for most types of epilepsy, including absence seizure and partial seizure, as well as for mood disorders.
234567
Despite a low frequency of known side effects, LTG reportedly exhibits several unique dosage-related side effects, including skin rashes.
8 However, few studies have investigated the effects of LTG on language and cognitive functions, particularly in the pediatric age group. Pressler et al.
9 reported that prescribing LTG to newly diagnosed children and adolescents with epilepsy had no impact on their cognitive function. However, most previous studies have only investigated adult patients and have focused on the effectiveness of LTG or the effect of different anticonvulsant agents on cognitive function, with a lack of specific research into the effect of LTG on language function.
101112
The present study extensively analyzed the effects of LTG on both cognitive and language functions in newly diagnosed pediatric epileptic patients receiving LTG monotherapy. We evaluated the language problem-solving abilities and receptive and expressive vocabulary in newly diagnosed pediatric patients undergoing LTG monotherapy with the aim of reaffirming its safety profile in relation to language development.
METHODS
Patients
The present study performed a retrospective chart review of prospectively collected data, including the type of epilepsy, demographic findings, and results of language function tests in 134 newly diagnosed pediatric epileptic patients (86 males and 48 females), who were evaluated at the Department of Pediatrics of Chonbuk National University Hospital prior to initiating treatment with LTG monotherapy. All patients started treatment with LTG alone, which was maintained until they had performed a second set of language function tests. Twenty-two of the 134 patients recruited for this study were excluded for the following reasons: a test interval of longer than 12 months (4 patients) and lack of data (18 patients). Thus, 112 patients (69 males and 43 females) were finally included in the study (
Table 1).
The control group comprised 50 children residing in the same province (Chonbuk province) who had no medical or medication history that might have affected their language ability. The age of the patient cohort was 9.6±2.7 years (mean±SD), while that of the control group was 9.1±3.3 years, making them a mean of around 6 months younger than the patient group. During this study, the subjects in the control group did not take a placebo pill or any medicine that could affect their language and cognition.
This study was performed after being approved by the Institutional Review Board of Chonbuk National University Research Council (approval no. CUH 2019-01-017).
Method
The starting LTG dosage was 1 mg/kg/day (maximum: 25 mg/day) for the first 14 days, which was increased to 2 mg/kg/day for the subsequent 14 days and then up to 7 mg/kg/day (or 200 mg/day) for maintenance. The mean dosage was 4.5 mg/kg/day. Language function tests were administered in the patient group prior to initiating LTG monotherapy and immediately after the titration level had been reached (usually 3 months later).
Language tests
Test of Problem Solving
The Test of Problem Solving (TOPS) is an evaluation tool that measures the metalinguistic skills in transforming logical thinking to language in children aged 5–12 years.
13 Our previous study
14 used the same TOPS as that used in the present study, and it is briefly described as below.
The purpose of the TOPS is to measure problem-solving skills by evaluating the ability to answer questions in specific situations. The test consists of three different categories: 1) 18 questions for determining causes, including answers to the question “why?,” 2) 20 questions for making inferences, including answers to the question “how?,” and 3) 12 questions for predicting, including answers to the questions “how do you know?” and “what happens?” The raw, mean, and total scores were determined for each category. Scores ranging from 0 to 2 were assigned depending on how the children responded in each category, yielding a total score of 100. The lengths of the answers to the questions were compared using the mean length of utterance in words (MLU-w), which defines a mean score of the length of articulation obtained by adding all words in the answer and then dividing them by the number of sentences included in the answer.
Vocabulary test: Receptive and Expressive Vocabulary Test
The Receptive and Expressive Vocabulary Test (REVT) is the standardized test that has been internally approved and externally applied for evaluating receptive vocabulary development skills, and it has been found to be applicable to individuals aged from 2.2 to 40.9 years.
15 The REVT comprises a total of 175 questions, and its responses involve children pointing to a picture and the examiner then providing a stimulus word. The illustration used in this study was an excerpt from material published by the American Guidance Service. The time required to finish the examination was 10–20 min. Raw scores were calculated based on baseline and ceiling results, and equivalent ages were also measured. The baseline was defined as the last item in the highest series of eight consecutive correct answers. The ceiling response was deemed to have occurred when a child incorrectly identified six of eight consecutive items. The raw score was calculated by subtracting the number of errors between the highest baseline and lowest ceiling.
Articulation test: Urimal Test of Articulation and Phonology
Articulation was evaluated using the Urimal Test of Articulation and Phonology, which is one of the articulation tests used for children aged between 2 and 12 years.
Articulation patterns were analyzed when the examinee answered the question after the examiner presented different picture cards as well as a target tone. A digital audio tape recorder (TC-D10/TC-D10 Pro, Sony, Tokyo, Japan) was used to record the responses of the examinees. Recording was performed in a room that blocked out external noise as much as possible, and the microphone was kept approximately 10 cm from their lips. When a child failed to answer, the examiner presented the target tone once and then asked the child to answer again.
Statistical analysis
Statistical analysis was performed using SPSS for Windows (version 18.0, SPSS Inc., Chicago, IL, USA). The independent t-test was used to compare differences between the control group and the epileptic patients prior to taking LTG, and the paired t-test was used to compare differences between before and after taking LTG. The criterion for statistical significance was set at p<0.05.
RESULTS
TOPS results
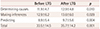
Comparison of problem solving for questions in the “determining causes” category
The scores in the determining-causes category were 11.9±4.7 and 12.9±4.8 for the pediatric epileptic patients before and after taking LTG, respectively, and the highest score was 36. There was a significant difference between before and after taking LTG (
p<0.01) (
Fig. 1,
Table 2) and also between the normal control group and the patients treated with LTG (
p<0.01).
In a comparison of linguistic representation skills of the children before taking LTG, they attempted to express their solutions to the question “why?” However, their answers were not very specific, occasionally providing inappropriate information or presenting one-word answers only. However, after taking LTG they were able to propose appropriate solutions with a specific reason and used more than two subjects and associated predicates (
Table 3).
After taking LTG, 42.6% of the entire group showed an increased mean score for answers to questions in the determining-causes category compared with that before taking LTG; the remaining 57.4% showed a decreased mean score.
Comparison of problem solving for questions in the “making inferences” category
The scores in the making-inferences category were 12.9±6.2 and 13.6±6.0 for the pediatric epileptic patients before and after taking LTG, respectively, and the highest score was 40. There was a significant difference between before and after taking LTG (
p<0.05) (
Table 2) and also between the normal control group and the patients treated with LTG (
p<0.01).
A close examination of verbal expressions before taking LTG revealed that the number of inappropriate expressions was larger for questions in the making-inferences category than for the other questions. After taking LTG, the examinees expressed diverse problem-solving methods that varied based on their experience. Cases that showed the greatest disparity between before and after taking medication are presented in
Table 3.
After taking LTG, 46.5% of the entire group showed an increased mean score for answers to questions in the makinginferences category compared with before taking LTG, while the score decreased in 38.6% and remained the same in 14.8%.
Comparison of problem solving for questions in the “predicting” category
The scores in the predicting category were 8.9±5.4 and 9.7±5.6 for the pediatric epileptic patients before and after taking LTG, respectively, and the highest score was 24. There was a significant difference between before and after taking LTG (
p<0.01) (
Table 2) and also between the normal control group and the patients treated with LTG (
p<0.01).
The problem-solving methods and verbal expressions used when answering questions differed significantly between before and after taking LTG. Prior to taking LTG, examines often provided only one answer to explain conditions or situations in the illustration, whereas after taking LTG they proposed at least three conditions when expressing expected results or speculation. After taking LTG the patients clearly expressed their predictions using words such as “maybe” and “could be,” but articulated their evidence of a clue using “because of,” which is not an appropriate expression for predictions (
Table 3).
After taking LTG, 48.5% of the entire group showed an increased mean score for answers to questions in the predicting category compared with that before taking LTG, whereas the score decreased in 44.6% and remained the same in 6.9%.
Changes in total problem-solving score in the TOPS
The total score among the preschool children for problem solving in the TOPS increased significantly from 33.5±14.5 before taking LTG to 35.7±14.2 after taking LTG (
p<0.01) (
Table 2), and the maximum score was 100. There was also a significant difference between the normal control group and the examinees after taking LTG (
p<0.01). After taking LTG, 57.4% of the entire group showed an increased problem-solving score compared with that before taking LTG, while the score decreased in 27.7% and remained the same in 14.8%.
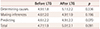
MLU-w in the TOPS
The MLU-w score in the determining-causes category did not differ significantly between before taking LTG (4.9±1.8) and after taking LTG (5.1±2.2,
p>0.05) (
Table 4). In contrast, the MLU-w scores in the making-inferences and predicting categories increased respectively between before and after taking LTG, but the changes were not statistically significant (both
p<0.05). The total problem-solving MLU-w score did not change significantly between before taking LTG (4.7±1.9) and after taking LTG (5.0±2.1,
p>0.05). Before taking LTG, the total problem-solving score in the determining- causes, making-inferences, and predicting categories showed statistically significant differences between the normal control group and the patients (
p<0.01).
Analyses of covariance revealed that changes in the TOPS scores did not differ significantly with sex, electroencephalography, diagnosis, or quantity of medication (all p>0.05).
Comparison of receptive language
The REVT was applied to epileptic patients before and after taking LTG. A comparative analysis was performed to determine whether LTG had an effect on receptive vocabulary development skills. The equivalent language age increased significantly from 9.4±3.4 years before taking LTG to 9.9±3.3 years after taking LTG (p<0.01). There was a significant difference between the normal control group and the patients before taking LTG. After taking LTG, 77.2% of the entire group showed an increase in the age for receptive vocabulary development skills, while this decreased in 16.8% and remained the same in 5.9%.
Articulation test
Articulation errors were evaluated according to the following four categories: substitution, distortion, omission, and addition. A mean of 97.8% patients articulated a correct consonant before taking LTG, while 98.5% articulated a correct consonant after taking LTG, with no significant difference (p>0.05). There was a significant difference between the normal control group and the patients before taking LTG (p<0.05).
The main error before and after taking LTG was distortion, with common errors and distortion detected in the alveolar fricative /s/, /s*/ and palatal affricate /ch/, respectively. Moreover, substitution error commonly occurred in the alveolar fricative /s/, /s’/ and palatal affricate /ch/. Omission error was noted in the velar plosive /k/ and alveolar liquid /l/.
DISCUSSION
Most caregivers of epileptic patients are concerned not only about epilepsy control but also the side effects of anticonvulsants, particularly medication-induced cognitive impairment, and hence it is very important to identify medicines with fewer side effects for the increasing pediatric patient population. LTG is considered a drug that can satisfy this condition; nonetheless, more data are required to make accurate judgments about cognitive and language functions, especially in the pediatric age group.
Gillham et al.
16 compared the effects of treatments with LTG and carbamazepine on health-related quality of life using the modified Side Effect and Life Satisfaction (SEALS) inventory, which includes items divided into the following five subscales: worry, temper, cognition, dysphoria, and tiredness. They showed that patients treated with carbamazepine had significantly worse SEALS scores than patients treated with LTG. Aldenkamp et al. reported cognitive improvements in newly diagnosed epileptic patients that favored LTG over both placebo and valproate.
17 A previous study even found that the spatial learning ability in rats improved upon exposure to LTG.
18 Although there have been reports of adverse effects of topiramate therapy on language development in children,
1920 few studies have evaluated the effects of relatively recently developed antiepileptic drugs on language function in the pediatric age group.
The present study analyzed the changes in language function in children treated with LTG, with a particular focus on the TOPS. Comparative analyses of problem-solving abilities were performed in three categories: determining causes, making inferences, and predicting. The mean score in the determining-causes category increased to 42.5%; furthermore, 46.5% and 48.5% of examinees showed increases in mean scores in the making-inferences and predicting categories, respectively, after LTG treatment. The MLU-w score increased between before and after taking LTG from 4.9 to 5.1 in the determining-causes category, from 4.6 to 4.9 in the making-inferences category, and from 4.7 to 5.0 in the predicting category. The total problem-solving MLU-w score also increased, from 4.7 to 5.0 (
Table 4). The answers before taking LTG were occasionally inappropriate or involved only one word, whereas the answers after taking LTG were grammatically correct and provided appropriate solutions with specific reasons.
The REVT was used as a comparative analysis tool for the receptive vocabulary development skills, which refer to the ability to see, hear, and understand linguistic stimuli. Receptive vocabulary development skills appeared to improve significantly after taking LTG (p<0.01). After taking LTG, 77.2% and 16.8% of epileptic patients exhibited higher and lower receptive language ages, respectively.
Articulation errors were evaluated according to substitution, distortion, omission, and addition categories. There was no significant change in the percentage of correct consonants and articulation patterns after taking LTG (p>0.05). It can be assumed that all vocal organ functions, language comprehension ability, and the discourse and pragmatic part of expressive language were relatively intact after taking LTG, because the evaluations of language and problem-solving skills, receptive vocabulary development skills, and articulation all indicated improvements.
From our comparative analyses of receptive vocabulary development skills as well as language and problem-solving skills before and after LTG treatment we concluded that LTG exerted no adverse effects on language in this study, for several reasons: first, the language and problem-solving skills improved significant in all categories (i.e., determining-causes, making-inferences, and predicting). After taking LTG, the answers of examinees became appropriate and were in the form of grammatically correct sentences. These results suggest that LTG treatment has no adverse effects on language and problem-solving skills. Second, the receptive vocabulary development skills improved after LTG treatment, and so it can be assumed that LTG treatment has no adverse effect on receptive vocabulary development skills. Third, the change in the percentage of correct consonants did not differ significantly between before and after taking LTG. The main articulation error was distortion both before and after treatment. As suggested in the above results and discussion, problem-solving skills, receptive vocabulary development skills, and the percentage of correct consonant improved significantly. This implies that clinical treatment with LTG will not lead to linguistic problems in pediatric epileptic patients.
The present study was subject to some limitations. Long-term patient monitoring and diverse tools for language evaluation were applied, but the methodology was still inadequate. Furthermore, it should be considered whether any improvement in scores is due to the practice effect or development, since the patients were exposed to repeated tests. Future studies should therefore employ more-specific methodologies and involve larger numbers of patients. Furthermore, our team plans to perform additional studies of the effects of long-term LTG medication use on language and problem- solving skills.
Notwithstanding the above limitations, we consider that the results obtained in this study provide useful preliminary data for patients treated with LTG, health-care workers, and speech therapists, and could be practical data for informing further studies of anticonvulsant medications.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download