Abstract
Background and Purpose
Methods
Results
Figures and Tables
 | Fig. 2Association of FGF23 with the burden of ICAS (A) and the burden of ECAS (B). X-axis indicates the burden of each type of cerebral atherosclerosis, and Y-axis indicates the value of natural logarithm of FGF23. ECAS: extracranial cerebral atherosclerosis, FGF23: fibroblast growth factor 23, ICAS: intracranial cerebral atherosclerosis. |
Table 1
Comparison of clinical characteristics and blood laboratory findings according the presence of cerebral atherosclerosis
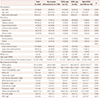
Data are n (%), mean±SD, or median [interquartile range] values.
*p<0.05 compared with no cerebral atherosclerosis in a Bonferroni post-hoc analysis, †p<0.05 compared with ECAS only in a Bonferroni post-hoc analysis, ‡p<0.05 compared with ICAS only in a Bonferroni post-hoc analysis.
ECAS: extracranial cerebral atherosclerosis, FGF23: fibroblast growth factor 23, ICAS: intracranial cerebral atherosclerosis, NIHSS: National Institute of Health Stroke Scale, WMHs: white-matter hyperintensities.
Table 2
Results of multivariate analyses of the presence and burden of cerebral atherosclerosis

Data are odds ratio (95% CI) values.
*Odds ratio could not be obtained because the FGF23 concentrations of patients with both ECAS and ICAS exceeded 182.0 pg/mL, †Adjusted for sex, age, BMI, coronary artery disease, prestroke antithrombotics, stroke subtype, NIHSS score, high-grade WMHs, Klotho, triglyceride, WBC count, total calcium, and CRP, ‡Adjusted for sex, age, hypertension, stroke subtype, NIHSS score, high-grade WMHs, WBC count, phosphate, and uric acid, §Adjusted for sex, age, hypertension, prestroke antithrombotics, NIHSS score, high-grade WMHs, Klotho, triglyceride, WBC count, and CRP.
BMI: body mass index, ECAS: extracranial cerebral atherosclerosis, FGF23: fibroblast growth factor 23, ICAS: intracranial cerebral atherosclerosis, NIHSS: National Institutes of Health Stroke Scale, WBC: white blood cell, WMHs: white-matter hyperintensities.
Acknowledgements
Notes
Author Contributions
Conceptualization: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Data curation: Dong-Ryeol Ryu, Hyung Jung Oh, Tae-Jin Song.
Formal analysis: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Funding acquisition: Tae-Jin Song.
Investigation: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Methodology: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Project administration: Tae-Jin Song.
Resources: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Supervision: Tae-Jin Song.
Validation: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Visualization: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Writing—original draft: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.
Writing—review & editing: Yoonkyung Chang, Jinkwon Kim, Ho Geol Woo, Tae-Jin Song.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download