Dear Editor,
Cerebellar ataxia (CA) is a heterogeneous disorder with various primary and secondary causes.1 The lack of a definitive cure means that many patients are unwilling to be evaluated for this disease. Financial expense is also a huge obstacle, although the economic burden on patients in South Korea has decreased since the July 2009 enforcement of the differential copayment system for rare incurable diseases.
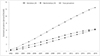
This retrospective cohort study searched the Health Insurance Review and Assessment Service (HIRA) database for patients who were registered more than twice as ataxia [G11 in the tenth revision of the International Classification of Disease, but not hereditary spastic paraplegia (G11.4)] between January 1, 2002 and December 31, 2016. During that period the estimated number of patients with CA in South Korea increased from 274 to 6,391. The crude prevalence increased from 0.58 to 12.47 patients/100,000, while the crude prevalence of hereditary and nonhereditary CA increased from 0.29 to 6.17 patients/100,000, and from 0.27 to 6.30 patients/100,000, respectively (Fig. 1).
Few previous studies have investigated the prevalence of CA. Similar research using the HIRA database found that the prevalence in South Korea was 8.22 patients/100,000 in 2012.2 However, a study based on the national registry for intractable diseases in Japan estimated that the prevalence was 18.5 patients/100,000 in 2008,3 while multicenter studies found it to be 31.1 patients/100,0004 in Japan and 10.2 patients/100,0005 in the UK.
While the estimated prevalence of CA in 20122 was much lower than that found in Japanese studies that analyzed the national registry,3 this study reflects a growing trend. However, we attribute this trend to the increased rate of diagnosis and the enforcement of the differential copayment policy, rather than indicating an actual increase in CA prevalence.
Recent advances in research and genetic analysis techniques are also important contributors. The first study of the distribution of spinocerebellar ataxia in South Korea was conducted in 2003,6 since when other studies have been conducted in 20117 and 2017.8 Additionally, the continuous education of neurologists, whose number increased dramatically from 462 in 2000 to 1,637 in 2015,9 may have increased the rate of CA diagnoses. Also, South Korea is one of the fastest-aging countries in the world, and this change in the population structure might also have affected the results.
According to a study conducted in South Korea in 2018, only about 30% of CA patients diagnosed at a tertiary hospital had hereditary CA.10 However, the crude prevalence rates of hereditary and nonhereditary CA were estimated to be almost the same in the present study. This discrepancy might be due to the discovery of a genetic abnormality in hereditary CA being more likely to be actively registered in the database in order to obtain financial support from the government system. Also, unlike the above-mentioned study, this database is not created by neurology experts as a claims database, and so the diagnostic accuracy is not guaranteed, which could result in the estimated prevalence of CA being either overestimated or underestimated. This suggests that it is essential for neurology experts to establish an objective database and for continuous research to be performed. Despite these limitations, this study is meaningful in that it performed a nationwide preliminary survey that confirmed the trends in the crude prevalence over decades. The findings of this longterm study suggest that changes in the real world, including in government policies, directly impact the estimated prevalence of rare diseases—but not their real prevalence—by influencing the rate of diagnosis.
Follow-up studies are required to facilitate the establishment of a national database for rare neurological movement disorders by neurologists. The establishment of new policies and changes in the clinical settings must be considered in any research that utilizes the national health insurance database in South Korea.
References
1. Stephen CD, Brizzi KT, Bouffard MA, Gomery P, Sullivan SL, Mello J, et al. The comprehensive management of cerebellar ataxia in adults. Curr Treat Options Neurol. 2019; 21:9.


2. Joo BE, Lee CN, Park KW. Prevalence rate and functional status of cerebellar ataxia in Korea. Cerebellum. 2012; 11:733–738.


3. Tsuji S, Onodera O, Goto J, Nishizawa M. Study Group on Ataxic Diseases. Sporadic ataxias in Japan--a population-based epidemiological study. Cerebellum. 2008; 7:189–197.


4. Shibata-Hamaguchi A, Ishida C, Iwasa K, Yamada M. Prevalence of spinocerebellar degenerations in the Hokuriku district in Japan. Neuroepidemiology. 2009; 32:176–183.


5. Muzaimi MB, Thomas J, Palmer-Smith S, Rosser L, Harper PS, Wiles CM, et al. Population based study of late onset cerebellar ataxia in south east Wales. J Neurol Neurosurg Psychiatry. 2004; 75:1129–1134.



6. Lee WY, Jin DK, Oh MR, Lee JE, Song SM, Lee EA, et al. Frequency analysis and clinical characterization of spinocerebellar ataxia types 1, 2, 3, 6, and 7 in Korean patients. Arch Neurol. 2003; 60:858–863.


7. Kim HJ, Jeon BS, Lee WY, Chung SJ, Yong SW, Kang JH, et al. SCA in Korea and its regional distribution: a multicenter analysis. Parkinsonism Relat Disord. 2011; 17:72–75.


8. Choi KD, Kim JS, Kim HJ, Jung I, Jeong SH, Lee SH, et al. Genetic variants associated with episodic ataxia in Korea. Sci Rep. 2017; 7:13855.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download