This article has been
cited by other articles in ScienceCentral.
Dear Editor,
A 65-year-old male (patient 1) who had a history of diffuse panbronchiolitis (DPB) with sinusitis for longer than 15 years presented with a 3-month history of weakness and numbness of both legs and the left hand. Sudden-onset painful weakness of the left distal leg had been the first symptom, which was followed by foot drop with paresthesia in the right leg 3 weeks later and weakness of the left hand 2 months after symptom onset. On admission, a neurological examination showed weakness in dorsiflexion (MRC grade 2/1, right/left) and plantar flexion (MRC grade 3/4, right/left) of the ankles, and grip power weakness (MRC grade 3) of the left hand. Nerve conduction study (NCS) showed distal multifocal axonal neuropathy (
Supplementary Table 1 in the online-only Data Supplement). Needle electromyography (EMG) demonstrated abnormal spontaneous activities with reduced recruitment of motor unit action potentials in the tibialis anterior (TA) bilaterally, right gastrocnemius medialis, and left first dorsal interosseous. Laboratory tests revealed leukocytosis (16,700/µL), and elevated erythrocyte sedimentation rate (ESR; 103 mm/h, normal <20 mm/h) and CRP (8.64 mg/dL, normal <0.3 mg/dL). The patient showed positive titers for serum myeloperoxidase-specific antineutrophil cytoplasmic antibody (MPO-ANCA), antinuclear antibody (ANA), and rheumatoid factor (RF). Neither proteinuria nor hematuria was found in urinalysis. High-resolution computed tomography (HRCT) of the chest showed diffuse thickening of the bronchial wall and multiple centrilobular nodules (
Supplementary Fig. 1A in the online-only Data Supplement). The arterial partial pressure of oxygen (PaO
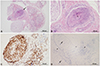
2) was 60 mm Hg, and the ratio of the forced expiratory volume in one second to the forced vital capacity (FEV1/FVC) was 56%. Analysis of the CSF produced unremarkable findings. A sural nerve biopsy revealed dense lymphoplasmacytic infiltration of the vascular walls, but neither extravascular eosinophils nor granulomatous inflammation was identified (
Fig. 1). The patient was diagnosed with vasculitic neuropathy (VN) in MPO-ANCA-associated vasculitis and treated with IV pulsed methylprednisolone (IVpM) and oral prednisone. The weakness symptoms improved except for foot drop at a 6-week follow-up, although the patient was treated for pneumonia immediately after the IVpM treatment.
A 40-year-old woman (patient 2) with an 8-year history of DPB and pansinusitis who was undergoing antibiotic prophylaxis with clarithromycin due to the frequent relapse of a respiratory infection presented with a 1-week history of painful weakness in both lower legs and the left hand. A neurological examination showed weakness (MRC grade 4+/3, right/left) of ankle dorsiflexion, decreased grip power (MRC grade 4) of the left hand, and sensory loss in both soles and the left palm. NCS showed distal asymmetric sensorimotor axonal polyneuropathy with no conduction block (
Supplementary Table 1 in the online-only Data Supplement). EMG demonstrated increased insertional activities in the TA bilaterally and the left abductor pollicis brevis. Laboratory tests showed leukocytosis (14,900/µL) and elevated ESR (98 mm/h) and CRP (6.74 mg/dL). The patient showed positive titers for serum ANA, RF, and anti-Ro/SSA, but negativity for ANCA and antiganglioside antibodies. The chest HRCT findings were consistent with DPB (
Supplementary Fig. 1B in the online-only Data Supplement). PaO
2 was 69 mm Hg and FEV1/FVC was 59.5%. The patient was treated with intravenous immunoglobulin G (IVIg) under the presumptive diagnosis of immune-mediated axonal multifocal neuropathy, which resulted in marked improvement of her symptoms. Six weeks later the patient complained of mild painful weakness of the right hand, and follow-up NCS showed distal sensorimotor axonal neuropathy with reduced compound muscle action potentials of the right median and left peroneal nerves.
DPB is a chronic inflammatory lung disease that exclusively affects the respiratory bronchioles.
1 It is clinically characterized by chronic cough, sputum, exertional dyspnea, and sinusitis, and which is radiologically characterized by bilateral diffuse micronodules with bronchiectasis.
1 Peripheral neuropathy in patients with DPB or chronic bronchiectasis has rarely been reported.
2 Our patient 1 with DPB was diagnosed with pathologically proven VN, which might indicate a relationship between DPB and MPO-ANCA. Patient 2 was also suspected of having VN for the following reasons: 1) clinically by two episodes of acute painful weakness confined to the distal limb in an asymmetric and asynchronous fashion,
3 2) electrophysiologically by distal multifocal axonal sensorimotor polyneuropathy in a non-length-dependent fashion,
3 and 3) laboratorially by leukocytosis and elevated inflammatory markers in the absence of constitutional symptoms or signs of infection.
3 The possibility of immune-mediated neuropathy associated with asymptomatic/pauci-symptomatic Sjögren's syndrome (SS) remains questionable due to the absence of additional studies for the diagnosis of SS.
4 Our patient 1 was treated with corticosteroids, while patient 2 was treated with IVIg. Both therapeutic options were clinically effective against peripheral neuropathy in the patients, although there was a limited response regarding the foot drop in patient 1, who experienced delayed diagnosis and treatment. Corticosteroids are preferentially recommended for treating patients with suspected VN,
3 but IVIg may be considered a first-line alternative in patients with DPB considering that DPB is known to increase the susceptibility to chronic airway infection,
2 and that immunosuppressive agents can increase the risk of infection generally.
5
These cases highlight that immune-mediated peripheral neuropathy including VN can occur in patients with DPB. Further study is required to clarify the relationships among DPB, peripheral neuropathy, and autoantibodies. Early diagnosis and prompt treatment can be important for preventing profound neurological sequelae.
Figures and Tables
Fig. 1
Histopathological features of patient 1. A: Sural nerve biopsy shows a markedly inflamed blood vessel (arrow) between peripheral nerve bundles. B: The obliterated arteriole has fragmented elastic laminae (arrowhead) and dense lymphoplasmacytic infiltrates in the wall (A and B: hematoxylin and eosin stain, ×40 and ×100, respectively). C: Leukocyte common antigen immunohistochemistry highlights inflammatory cells in the vascular walls (×200). D: Epon section shows few remaining myelinated fibers with a myelin bulb (arrows) and blood vessels with inflammatory cells (arrowheads) (toluidine blue stain, ×200).
Acknowledgements
This work was supported by a grant (BCRI 19049) from the Chonnam National University Hospital Biomedical Research Institute.
References
1. Poletti V, Casoni G, Chilosi M, Zompatori M. Diffuse panbronchiolitis. Eur Respir J. 2006; 28:862–871.


2. Park J, Banno S, Sugiura Y, Yoshikawa K, Naniwa T, Wakita K, et al. Microscopic polyangiitis associated with diffuse panbronchiolitis. Intern Med. 2004; 43:331–335.


3. Collins MP, Dyck PJ, Gronseth GS, Guillevin L, Hadden RD, Heuss D, et al. Peripheral Nerve Society Guideline on the classification, diagnosis, investigation, and immunosuppressive therapy of non-systemic vasculitic neuropathy: executive summary. J Peripher Nerv Syst. 2010; 15:176–184.


4. Flament T, Bigot A, Chaigne B, Henique H, Diot E, Marchand-Adam S. Pulmonary manifestations of Sjögren’s syndrome. Eur Respir Rev. 2016; 25:110–123.


5. Fardet L, Petersen I, Nazareth I. Common infections in patients prescribed systemic glucocorticoids in primary care: a population-based cohort study. PLoS Med. 2016; 13:e1002024.

Supplementary Materials
Supplementary Fig. 1
Chest high-resolution computed tomography findings. Axial images show diffuse multiple centrilobular nodules and bronchiectasis and bronchitis of both lungs in patient 1 (A) and patient 2 (B), which suggests diffuse panbronchiolitis.
Supplementary Table 1
Results of nerve conduction studies of the two patients




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download