This article has been
cited by other articles in ScienceCentral.
Dear Editor:
Dermatologic complaints account for 3.3% of patients visiting the emergency department (ED)
1. Although most dermatologic problems are not life-threatening, specialized differential diagnosis is important because dermatologic diseases can interfere with normal daily activities. However, in most hospitals, dermatologists cannot reside in the ED for 24 hours. Consequently, most patients did not receive specific diagnosis and medical care. Thus, analysis of dermatologic diagnosis in the ED could be useful data for emergency physicians.
There are three published papers from Korea regarding patients with skin problems visiting the ED. Among them, one was published in 1997 and, therefore, does not reflect the current situation
2. Another paper addresses eight years of progress, but the diagnosis was made by emergency medicine physicians only
3. In the last paper, grasping the overall trends is difficult owing to the limited time period covered by the report
4. In the current paper, patients treated over a period 11-years in a single secondary hospital providing a referral to dermatologists were analyzed. Although numerous international studies have provided information on emergency dermatoses, only a few published studies have attempted to characterize emergency dermatology referrals. To the best of our knowledge, this study includes the largest series of prospectively obtained data on the ratio of dermatology referrals from the ED. The aims of this study were to twofold: first, to determine clinical characteristics of patients with a dermatological problem in ED using a large population data; second, to identify skin conditions that required referrals to the dermatologists. This study included patients who received a dermatology diagnosis code in the ED of Dongguk University Hospital, Korea, between January 1, 2006, and December 31, 2016. The hospital is a 700-bed secondary care hospital, with emergent medical services being provided by emergency physicians; a dermatology on-call system is available 24 h/d. The hospital uses an electronic medical record (EMR) system, and a diagnosis code is required prior to discharge from the ED. Therefore, the EMR system provides a good source of accurate data. The International Statistical Classification of Diseases, 10th Revision (ICD10) codes were first extracted from patients visiting our dermatology outpatient clinic. Then, a list of patients given these ICD codes in the ED was collected. Based on the collected medical records, diagnosis frequencies, hospitalization rates, and dermatology referral rates were analyzed. All data were analyzed using Excel 2013 (Microsoft, Redmond, WA, USA).
We identified 20,863 patients with dermatologic complaints. Dermatological patients accounted for 5.9% of all ED patients, corresponding to an average of 5.2 patients per day. The number of dermatologic diagnoses made in the ED increased 645%, from 478 to 3,085 during an 11-years. Approximately equal numbers of males (49.8%) and females (50.2%) were observed. Children under 10 years accounted for 40.9% of cases. Of the 181 diagnoses identified in this study, urticaria/angioedema, burns, and cellulitis were the three most common dermatoses in ED. The 10 most common ones contributed to 79.6% of all diagnosis Urticaria is the most common in both children and adults. In adults, disease frequencies of allergic contact dermatitis, herpes zoster infection, cellulitis, and drug eruption are higher than in children (
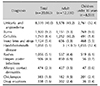
Table 1). During the eleven years, 1.95% of patients were admitted for their skin disease. The main dermatoses leading to hospitalization were herpes zoster infections (39.7%), followed by cellulitis (19.5%) and staphylococcal scalded skin syndrome (5.9%). Of the 20,863 patients, 19.5% of patients were referred to dermatologists. The most common diseases referred to dermatologists were shown in
Table 2.
In accordance with previous studies, a large number of ED dermatoses were urticaria/angioedema. Other previous studies reported an analogous disease spectrum; cellulitis, herpes zoster, contact dermatitis, and drug eruption. To the best of our knowledge, the publications regarding dermatology referrals from ED physicians are scarce. Previous studies reported similar disease spectrum; bullous disease, erythema multiforme, and drug eruption
5. Especially, eczema herpeticum, scabies, bullous disorder, and pityriasis rosea were only diagnosed by dermatologists in this study. Those dermatoses were unfamiliar to ED physicians. Among them, misdiagnosis of scabies may lead to serious results. Therefore, clinical manifestations and examinations of scabies should be included in the education program in ED physicians. The five most frequent diagnosis (urticaria and angioedema, burns, cellulitis, insect bites and stings, and hand, foot, and mouth disease) had rarely referred to a dermatologist in our study, which partly explains the low referral rate to dermatologists. This is because ED physicians have more experience, as these skin problems commonly encountered in the ED. Also, as the lack of ability of non-dermatologist to diagnosis even in common dermatosis had been reported before
6, common dermatoses in ED may assist the ED physicians to make better clinical decisions. In addition, 75% of diagnosis of cellulitis by primary care physicians were incorrect after re-evaluated by dermatologists
7. Those high rates of misdiagnosis of dermatoses would suggest a significant role of dermatologists in the ED and more focused training for ED physicians about the confusing skin conditions.
Our study presents some limitations. Children under 10 years represented the largest group. This result seems to reflect the demographics of the population served by the hospital. According to the 2015 data from the Korea National Statistical Office, children under 14 years olds constituted 13.90%, 14.44%, 17.21% in the total nation, the city of the hospital, neighboring city of the hospital populations, respectively. These demographic characteristics may partially explain the high proportion of pediatric patients in this study. Also, as this study was a single center study, generalizing the results to all populations may be limited. In addition, the dermatologists involved in this study were all dermatology residents; hence, the accuracy of their diagnosis was limited. However, as the accuracy of diagnosis made by dermatology residents and dermatology specialists were 91% and 96%, respectively, versus 52% for non-dermatologist physicians
8, this would not have influenced the reliability of our findings.
In conclusion, it might be impossible to educate all the dermatosis to ED physicians, therefore, common dermatosis in ED and skin conditions that required referrals to the dermatologists should be addressed in ED physicians and dermatology residents education.
Figures and Tables
Table 1
Top 10 dermatologic diagnoses by frequency
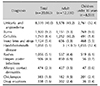
Table 2
Dermatoses mainly referred to a dermatologist in ED

ACKNOWLEDGMENT
The Institutional Review Board of the Dongguk University Ilsan Hospital approved the study (IRB no. DUIH 2017-08-007).
References
1. Baibergenova A, Shear NH. Skin conditions that bring patients to emergency departments. Arch Dermatol. 2011; 147:118–120.


2. Son BS. A statistical analysis of dermatologic emergency patients visiting the emergency room over 10 years (1986∼1995). Korean J Dermatol. 1997; 35:223–227.
3. Lee HJ, Jung HJ, Nam JH, Park JH, Lee GY, Kim WS. A statistical analysis of dermatology patients visiting the emergency department in the recent 3 years (2010~2012). Korean J Dermatol. 2015; 53:10–15.
4. Kim JY, Cho HH, Hong JS, Jin SP, Park HS, Lee JH, et al. Skin conditions presenting in emergency room in Korea: an eight-year retrospective analysis. J Eur Acad Dermatol Venereol. 2013; 27:479–485.


6. Tay LK, Lee HY, Thirumoorthy T, Pang SM. Dermatology referrals in an East Asian tertiary hospital: a need for inpatient medical dermatology. Clin Exp Dermatol. 2011; 36:129–134.


7. Arakaki RY, Strazzula L, Woo E, Kroshinsky D. The impact of dermatology consultation on diagnostic accuracy and antibiotic use among patients with suspected cellulitis seen at outpatient internal medicine offices: a randomized clinical trial. JAMA Dermatol. 2014; 150:1056–1061.


8. Federman DG, Concato J, Kirsner RS. Comparison of dermatologic diagnoses by primary care practitioners and dermatologists. A review of the literature. Arch Fam Med. 1999; 8:170–172.












 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download