This article has been
cited by other articles in ScienceCentral.
Abstract
The prevalence of gestational diabetes mellitus (GDM) has been increasing worldwide, as has the economic cost associated with this condition. GDM threatens the health of the mother and child, and thus proper monitoring and management are essential. Mobile healthcare services have been applied to manage some diseases, particularly chronic diseases. We aimed to evaluate the utility of a mobile application in nutritional intervention by observing cases of a mobile application in a series of patients with GDM. We provided a mobile-based intervention to GDM patients and collected biochemical and nutritional information. The mobile-based nutritional intervention was effective in controlling carbohydrate intake and improving blood glucose level for patients with GDM.
Keywords: Gestational diabetes, Diet therapy, Mobile applications, Diet, food, and nutrition
INTRODUCTION
The prevalence of gestational diabetes mellitus (GDM) is increasing worldwide [
1], including in Korea [
2]. The economic cost associated with treating GDM has also been increasing [
3]. GDM carries risks of complications to both the mother and fetus, including the need for a cesarean section, shoulder dystocia, macrosomia, or neonatal hypoglycemia, among others. Various risk factors are known to be associated with GDM; among them, pre-pregnancy obesity, inadequate nutrition, and sedentary lifestyle have been suggested to be modifiable factors, while advanced maternal age, personal history of GDM or prediabetes, family history of diabetes, ethnicity (Asian, Hispanic, native- and African-American), maternal history of low birth weight, twin pregnancy, and genetic susceptibility have been proposed as unmodifiable factors for GDM [
4].
Previous studies have shown that women with GDM were 7.43-fold more likely to subsequently develop type 2 diabetes mellitus than were women who had a normoglycemic pregnancy [
5]. Moreover, it has been reported that the maternal glucose concentration has a strong, continuous association with perinatal complications, including birth weight and fetal hyperinsulinemia [
6]. Therefore, glycemic control is very important for women with GDM. Among patients with GDM, medical nutrition therapy (MNT) might be necessary immediately after GDM detection, because diet management is important for maintaining blood glucose levels within the normal range. The Korean Diabetes Association recommends that MNT be the first step in GDM management [
7]. The goals of MNT for pregnant women with GDM are to control the blood glucose level and to prevent ketosis, but also to ensure adequate nutrient intake for achieving the recommended weight gain and supporting fetal growth. Apart from glycemic control, excessive weight gain in patients with GDM can increase the risk of a cesarean section. Traditionally, dietary recommendations for women with GDM have focused on restricting carbohydrate (CHO) intake. However, recently, nutritional strategies that can help improve maternal glucose levels and prevent an excessive infant birth weight have been proposed [
8]. A personalized dietary intervention might help in ensuring adequate meals are consumed, controlling maternal blood glucose, and maintaining proper fetal weight gain.
Mobile healthcare, a field that has grown rapidly in recent decades, allows for the timely and cost-effective treatment of diseases over long distances. In the early 2000s, information technology-based disease management consisted of short message services and internet-based patient portals, and focused on medication adherence, motivation for self-management, and provision of appointment reminders [
9]. Since then, disease management options have expanded to include educational materials and recommendations for lifestyle interventions [
10]. Several previous studies have assessed the effectiveness of mobile healthcare applications for adult patients with diabetes; however, few studies have included women with GDM. Miremberg et al. [
11] reported that smartphone use for disease management significantly lowered blood glucose levels in patients with GDM. As proper nutrition and glycemic control during pregnancy are essential to maternal and fetal health, the use of mobile-application (mAPP)-based healthcare may prove to be beneficial in helping patients control their glucose levels. Therefore, herein, we examined the effects of an mAPP-based nutritional intervention program in a series of patients with GDM.
CASE
All participants signed a written informed consent before participation and this study was approved by the Institutional Review Board (IRB) of Kangbuk Samsung Hospital (IRB No. 2019-11-049). The cases were 4 singleton participants who were diagnosed with GDM between 24 and 28 weeks of pregnancy. We collected data on their lifestyle habits, including diet, and laboratory data at baseline, at 32 and 36 weeks of gestation and after delivery. The mAPP (Huraypositive Inc., Seoul, Korea) was used as a communication platform between the patients with GDM and medical professionals. All participants measured and recorded their diabetes self-management activities, including blood glucose level, diet, exercise, and medication intake, using monitoring system devices, such as a glucometer with a Bluetooth connection and an accelerometer. The mAPP collected patients' clinical data and any messages sent to medical staff. After a user entered information into the mAPP, the data were automatically transmitted through a wireless network to the study server.
The overall process of nutrition management is shown in
Figure 1. At baseline, a certified clinical dietitian conducted nutrition assessments and delivered nutrition education to each patient; the dietitian also collected data on each patient's dietary history, including dietary habits and food intake (24-hour recall method). Participants were taught basic diet therapy for GDM, which included guidance regarding their food choices, meal planning, and sample recipes, among others. Training for using a meal plan was provided using a food exchange table (for participants who had not been prescribed any insulin treatment) or CHO counting (for participants prescribed insulin treatment). Participants were further instructed by the clinical dietitian on how to record their food intake and check their data and dietary report within the mAPP.
 | Figure 1 The overall process of nutrition management provided to participants.
|
Throughout the study period, the clinical dietitian posted tailored messages to each patient twice a month until delivery, while educational material on GDM management was provided once a week. The educational material consisted of information on CHO sources, snacks, beverage intake, oily fish intake, calcium intake, dietary interventions for constipation, and precautions recommended when eating out. At 32 and 36 weeks, a 3-day food diary was collected and evaluated. Messages were tailored based on the individual glycemic control status, diet, and physical activity data. In addition, 14 nutrition facts were listed in the mAPP, which consisted of general knowledge regarding nutrition (
Figure 2).
 | Figure 2
Samples of nutrition fact listed in the mAPP, weekly nutrition education material, and tailored message. (A) Nutrition fact listed in the mAPP. (B) Weekly nutrition education material. (C) Tailored message.
mAPP, mobile-application.

|
After delivery, the clinical dietitian provided another education session, which focused on postpartum nutritional care and dietary management for weight control and diabetes prevention.
Table 1 shows the changes in participants' energy and nutrient levels over the course of the study.
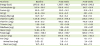
Table 2 shows the CHO:protein:fat proportions of participants according to the study period. No significant differences in these proportions were noted between periods. Protein intake decreased at week 36 compared to baseline, although, with a single exception, participants met over 90% of their protein recommended nutrient intake (RNI) for pregnant women. Iron consumption levels remained stable throughout the study; however, the proportion of animal iron consumed decreased over time. Calcium intake gradually decreased compared to baseline. The RNI for calcium (700 mg per day) was met at baseline, but not at week 32 or 36. The mean hemoglobin A1c level was 5.4% at baseline, which was retained until delivery (5.5% at week 36). Blood glucose levels, particularly postprandial glucose levels, were improved at week 36 compared to baseline. Individual data on key nutrients and the blood glucose level are shown in
Figure 3.
Table 1
Nutreints intake of participants
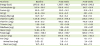
|
Nutrients |
Baseline |
At 32 weeks |
At 36 weeks |
|
Energy (kcal) |
1,870.2 ± 82.8 |
1,567.7 ± 192.7 |
1,549.9 ± 242.5 |
|
Carbohydrate (g) |
247.4 ± 38.8 |
198.0 ± 41.6 |
210.7 ± 26.6 |
|
Protein (g) |
88.2 ± 15.7 |
90.2 ± 14.2 |
81.6 ± 19.3 |
|
Fat (g) |
64.9 ± 14.6 |
49.4 ± 6.2 |
49.1 ± 9.6 |
|
Dietary fiber (g) |
30.7 ± 3.7 |
25.3 ± 6.3 |
25.0 ± 7.0 |
|
Vitamin A (µRE) |
1,011.8 ± 577.2 |
1,454.4 ± 478.2 |
1,135.5 ± 471.5 |
|
Vitamin C (mg) |
157.6 ± 51.5 |
166.3 ± 88.5 |
145.6 ± 58.0 |
|
Thiamin (mg) |
1.22 ± 0.16 |
1.53 ± 0.50 |
1.17 ± 0.23 |
|
Riboflavin (mg) |
1.41 ± 0.38 |
1.36 ± 0.18 |
1.32 ± 0.27 |
|
Niacin (mg) |
18.83 ± 4.79 |
17.89 ± 2.51 |
18.04 ± 3.69 |
|
Folate (µg) |
842.1 ± 108.5 |
625.5 ± 138.7 |
629.2 ± 171.6 |
|
Calcium (mg) |
803.5 ± 161.9 |
679.9 ± 140.3 |
637.1 ± 195.8 |
|
Iron (mg) |
17.8 ± 1.2 |
17.5 ± 3.6 |
13.1 ± 7.7 |
|
Animal iron (mg) |
5.03 ± 2.1 |
3.9 ± 1.4 |
3.4 ± 0.8 |
|
Plant Iron (mg) |
12.7 ± 2.2 |
13.6 ± 4.0 |
16.5 ± 7.3 |

Table 2
Macronutrient composition of the diet participants consumed (n = 4)

|
Macronutrients |
Baseline |
At 32 weeks |
At 36 weeks |
|
Carbohydrate (%) |
51.4 ± 8.3 |
49.2 ± 5.2 |
52.6 ± 3.3 |
|
Protein (%) |
18.3 ± 3.1 |
22.9 ± 4.4 |
20.1 ± 1.9 |
|
Fat (%) |
30.2 ± 6.2 |
27.9 ± 0.9 |
27.3 ± 1.7 |

 | Figure 3
Individual nutrients intake status and blood glucose level throughout the study period.
FBS, fasting blood sugar; PP2, 2-hours post-prandial glucose*; CHO, carbohydrate; RNI, recommended nutrient intake.
*PP2 was measured after oral intake of 75 g glucose.

|
DISCUSSION
The data obtained from this case series suggest that mobile healthcare might be an effective form of intervention for pregnant women diagnosed with GDM.
CHO intake directly affects the blood glucose level [
12]. A CHO-controlled meal plan is an important part of MNT for GDM [
7]. Although CHO restriction has been a key nutritional strategy for treating GDM, it has recently been revealed that strict CHO restriction can increase fat consumption, worsening insulin resistance and potentially raising the blood glucose level [
13]. The Korean Diabetes Association recommends a CHO-restricted diet, consisting of 50% CHOs, 30% protein, and 20% fat, noting that it can improve the postprandial blood glucose level and help prevent excessive fetal growth [
7]. In the present study, the level of nutrient intake of the participants and health outcome were improved by the mAPP-based nutrition management program. Total CHO consumption decreased, and the proportion of CHO remained at around 50% of the diet. Furthermore, improvement in glycemic control was observed in this study. Previously, Guo et al. [
14] reported that patients with GDM who followed a mobile health intervention demonstrated significantly lower hemoglobin A1c before delivery, lower rates of off-target measurements of both fasting blood sugar and 2-hour postprandial glucose, and lower frequency of outpatient service usage than did control patients who received standard care. Similarly, Miremberg et al. [
11] reported that mAPP-based feedback and communication for patients with GDM was effective in achieving glycemic control (measured with mean blood glucose, fasting glucose, and 1-hour postprandial glucose). Our findings are consistent with the results of these prior studies. Herein, the hemoglobin A1c level achieved was within the target range and the blood glucose levels (fasting and postprandial) improved in all participants.
It is essential to meet the recommended energy, protein, and micronutrient intake levels to achieve proper maternal health and fetal growth. The physiological needs of pregnant women change to meet the additional nutritional needs of the fetus that arise during pregnancy. Among our participants, protein levels were low and insufficient to meet the RNI. Additionally, while participants' calcium intake met the RNI at baseline, it subsequently decreased below the RNI level (700 mg). These reductions in protein and calcium consumption might have resulted from changes to the overall diet, for example, the CHO restriction. In Korea, CHO-based foods, such as rice, are the major parts of a meal. As a result, any restrictions in CHO-rich food intake might be accompanied by reduced intake of other nutrients, including protein and micronutrients. These results suggest that the overall diet quality must be emphasized alongside CHO restriction to improve glycemic control in the nutritional management of patients with GDM. Moreover, mAPPs for diabetes tend to focus on glycemic control. Therefore, when planning new mAPP-based nutrition strategies for patients with GDM, more attention should be given to providing guidance on achieving healthy and balanced food intake.
The efficacy of mAPPs developed to support the management of chronic diseases varies depending on the patient's compliance and individualized management methods. A personalized approach is key to increasing user compliance. Clinical dietitians play an important role in providing personalized nutrition advice. However, only a few studies conducted on mobile-based management for GDM included a clinical dietitian. In the future, the involvement of a clinical dietitian should be considered when planning and developing mAPP-based nutrition care services.
In conclusion, a mobile-based nutrition management program for patients with GDM was effective in controlling CHO intake and improving glycemic control. However, reduced intake of some nutrients was observed. Future management approaches for patients with GDM should focus on achieving glycemic control as well as maintaining the optimal nutrition status.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download