INTRODUCTION
Diabetes mellitus is a serious health problem, and its global burden is continually increasing. The International Diabetes Federation estimated that the number of people with diabetes was 451 million in 2017, and that the figure is expected to increase to 693 million worldwide by 2045.
1 In Korea, the prevalence of diabetes has been increasing rapidly, reaching 13.4% and 28.0% in individuals older than 30 and 65 years, respectively, in 2017.
2 However, the treatment rate of Korean population with diabetes is 66.7%, and the control rate (hemoglobin A1c <6.5%) is only 32.9%, indicating the absence of adequate control.
2
The effective management of diabetes can reduce the risk of complications in affected individuals. Diabetes self-management education (DSME) empowers people with diabetes to control the disease through education programs, including regular physical activity, nutrition therapy, smoking cessation, adherence to drug therapy, and preventive care practices. DSME has become essential as diabetes care has increasingly become the responsibility for people with diabetes, their families, and healthcare professionals. The American Diabetes Association recommends that people with diabetes should engage in DSME to improve their knowledge, skills, and the ability to control the disease.
3 DSME can improve health status, clinical outcomes, and quality of life and reduce diabetes-related costs.
4567 However, recent studies have shown that the rate of participation in DSME in Korea ranges from 15% to 53%.
8910
Identifying sociodemographic factors related to attendance in DSME programs is crucial to achieve equality and increase the involvement of socioeconomically vulnerable groups in these programs. However, few studies have investigated these factors. This study investigated these factors in community-dwelling adults with diabetes using data from a nationwide Korean survey, and assessed whether these variables differed according to the type of institutions providing DSME.
MATERIALS AND METHODS
Study population
Data from the 2016 Korea Community Health Survey (KCHS) conducted by the Korean Centers for Disease Control and Prevention were analyzed. KCHS is an ongoing annual cross-sectional, nationwide survey that started in 2008. A sample of 900 participants from 253 community health centers was selected to obtain a sampling error of ±3% with a 95% confidence interval (CI) for each major health index in each center. KCHS used a two-stage sampling design and created a sample extraction frame by linking registered population data from the Ministry of Public Administration and Security with housing data from the Ministry of Land, Infrastructure, and Transport. In the first stage, the sampling area (Tong · Ban/Ri) was extracted as the probability proportional to size based on the number and types of households in the smallest administrative units (Dong/Eup · Myeon). In the second stage, the number of sample households was extracted from the sampling area using a systematic sampling method. All participants older than 19 years were interviewed by trained researchers using computer-assisted personal interviewing process. Using multistage stratified cluster sampling, the 2016 KCHS survey included 228452 family residents. Of the total respondents aged ≥30 years, 23862 were diagnosed with diabetes. After excluding 462 subjects with missing sociodemographic information, the final sample consisted of 23400 people. Written consent was obtained from all participants. The study protocol was approved by the Institutional Review Board of Wonkwang University Hospital (WKUH 2019-05-008).
Data
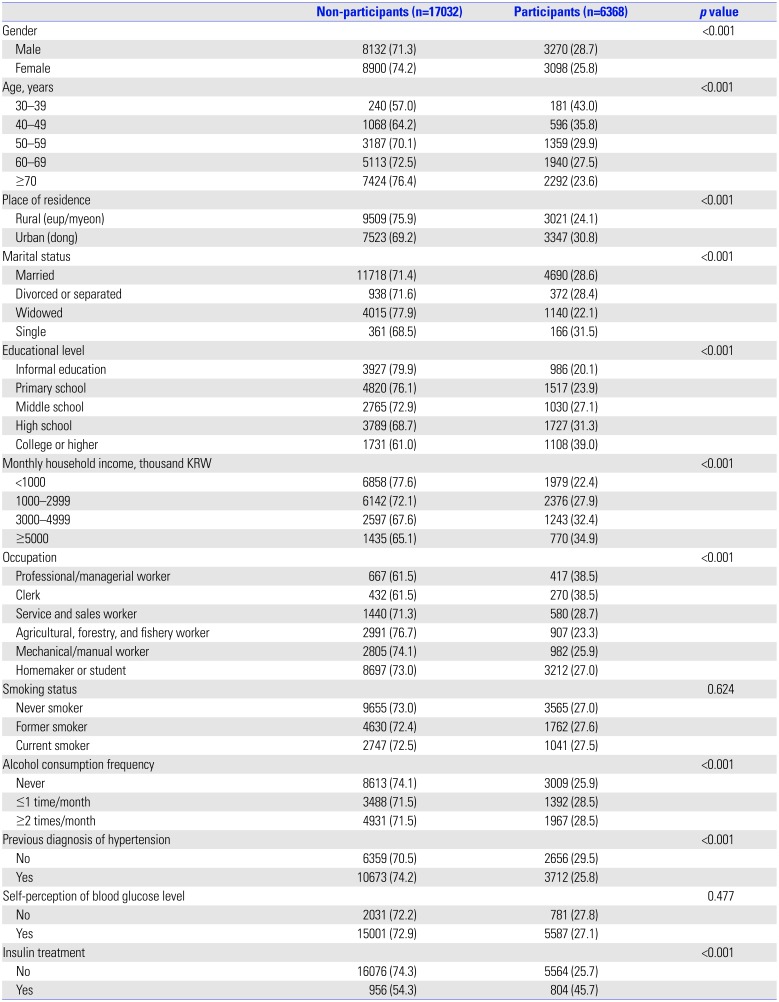
Information on sociodemographic variables, health behaviors, and health status were collected using standardized questionnaires. The evaluated variables were age group (30–39, 40–49, 50–59, 60–69, and ≥70 years of age), place of residence (rural or urban), marital status (married, divorced/separated, widowed, or single), educational level (informal education, primary school, middle school, high school, or college or higher), monthly household income (<1000, 1000–2999, 3000–4999, or ≥5000 thousand KRW), and type of occupation (professional/managerial worker, clerk, service/sales worker, agricultural/forestry/fishery worker, mechanical/manual worker, or homemaker/student).
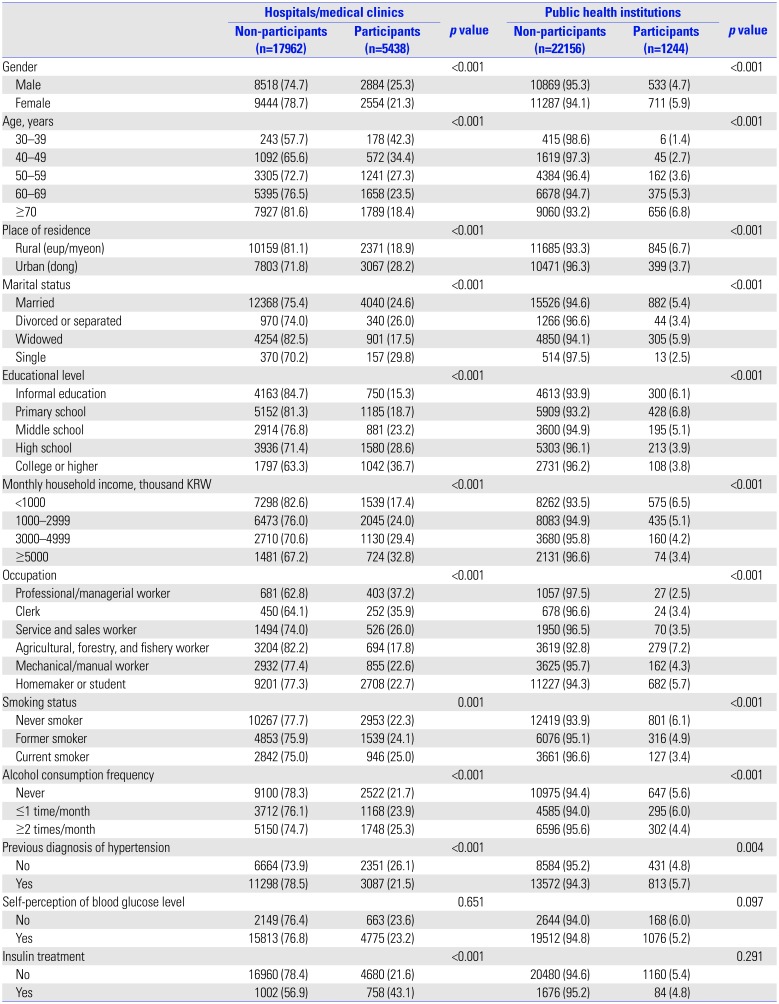
Confounding variables included smoking status (never, former, or current smoker), alcohol consumption frequency (never, ≤1 time/month, or ≥2 times/month), previous diagnosis of hypertension (yes or no), self-perception of blood glucose level (yes or no), and insulin treatment (yes or no). The outcome variable (attendance to DSME programs) was evaluated using the following questions: “Have you ever participated in education on diabetes care (excluding consultations with doctors, nurses, or other professionals lasting less than 10 minutes)?” The respondents who answered “Yes” to this question were classified according to the type of institutions: hospitals/medical clinics (HMCs) and/or public health institutions (PHIs).
Statistical analysis
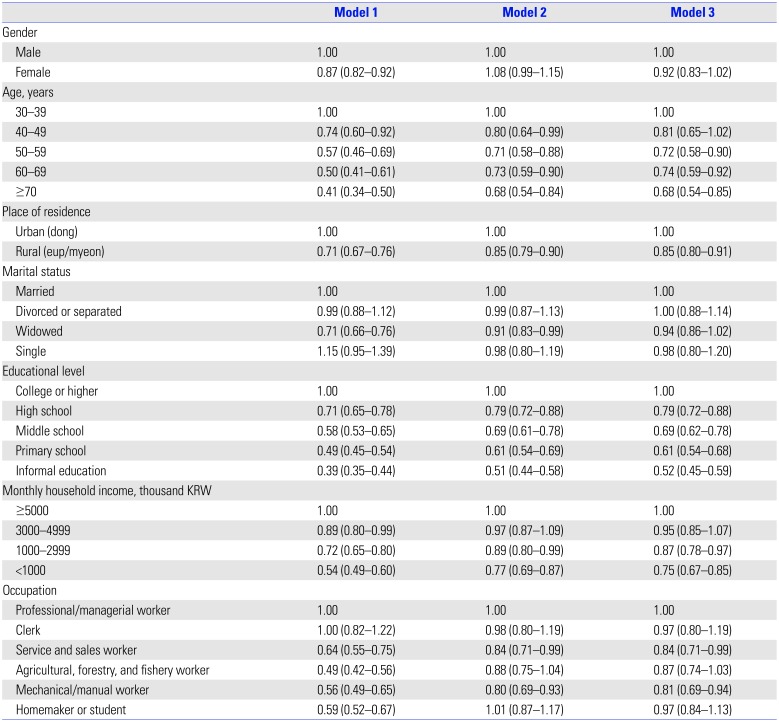
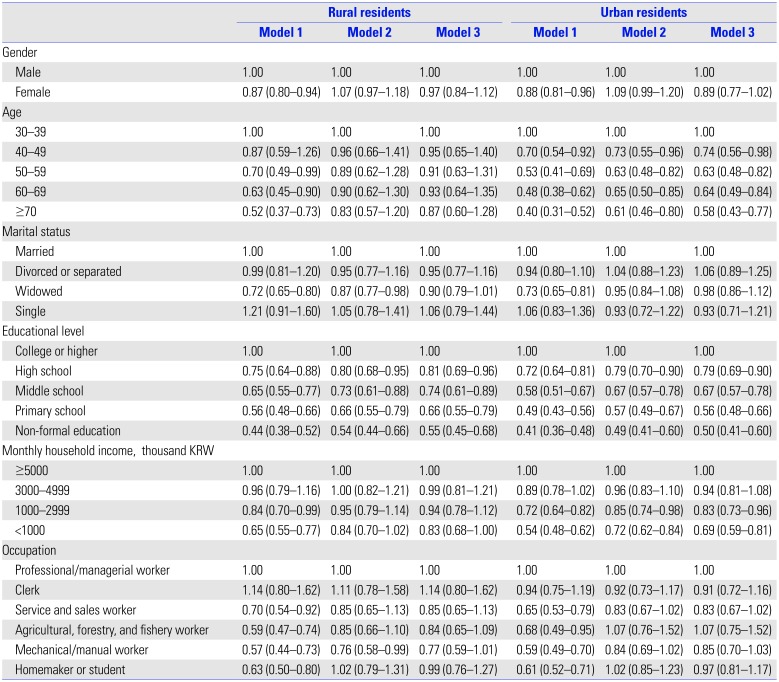
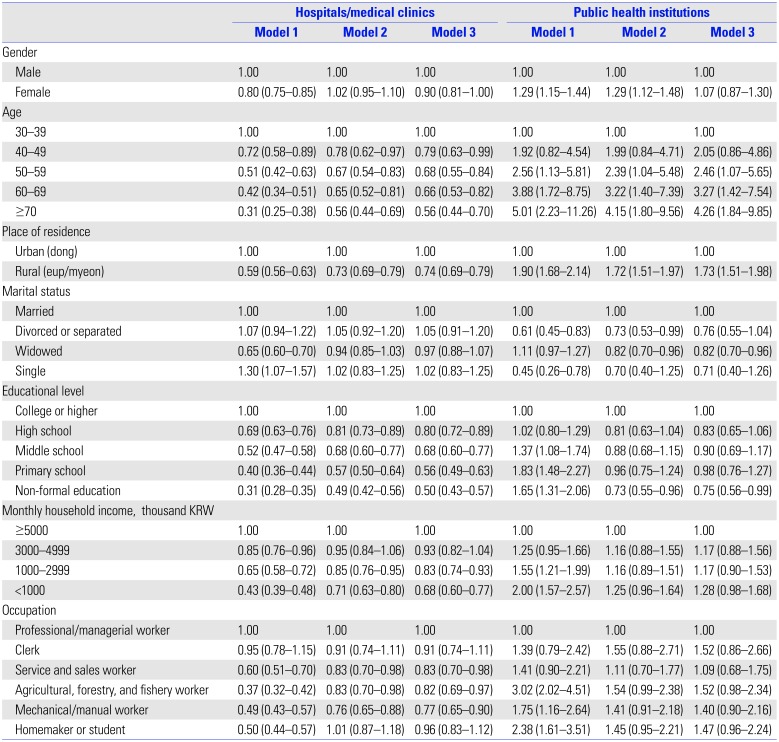
Variables were presented as frequency (percentages), and differences in sociodemographic variables related to participation in DSME were assessed using chi-square test. Logistic regression analysis was used to examine the association between these variables and involvement in DSME. Model 1 was unadjusted; model 2 was adjusted for sociodemographic variables; and model 3 was adjusted for sociodemographic variables, smoking status, frequency of alcohol consumption, previous diagnosis of hypertension, self-perception of blood glucose level, and insulin treatment. Odds ratios (ORs) with 95% CIs for participation in DSME according to the abovementioned variables were calculated. All statistical analyses were performed using SPSS software version 22.0 (IBM Co., Armonk, NY, USA). A p-value less than 0.05 was considered statistically significant.
DISCUSSION
We identified the sociodemographic factors associated with participation in DSME in a large community-dwelling population with diabetes. Older age, living in rural areas, lower education level, lower monthly household income, and the type of occupation were significantly associated with lower overall attendance to DSME programs. However, older age, living in rural areas, and the type of occupation (agricultural/forestry/fishery worker and homemaker/student) were significantly associated with higher participation in DSME at PHIs.
Younger adults with diabetes showed lower diabetes self-efficacy for self-management, poorer self-management, and poorer glycemic control than older adults.
11 Furthermore, given that the number of young adults with diabetes is increasing, higher engagement of younger people with diabetes in DSME is essential. Epidemiological studies have shown that older people with diabetes are less likely to engage in DSME.
1213 Although previous studies in Korea reported that age was not an independent factor for attending DSME,
810 the present results have shown that overall enrollment in DSME was relatively lower in older age groups. Furthermore, older people were more likely to attend DSME at PHIs than at HMCs. Therefore, the participation of older adults was lower as the overall percentage of people enrolling in DSME at HMCs was more than four times higher than at PHIs (23.2% vs. 5.3%).
Consistent with previous studies, education level was one of the most significant factors associated with enrollment in DSME.
8101214 Compared to individuals with diabetes with college or higher education, people with diabetes with informal education were nearly half as likely to attend DSME. People with higher education may have more knowledge about diabetes and higher access to information on the importance of long-term management of diabetes.
810 Moreover, educational level was inversely associated with the risk of cardiovascular disease and all-cause mortality.
15
There are 33394 HMCs in Korea (3237 hospitals and 30157 clinics) and 3492 PHIs (252 health centers, 1336 secondary health care facilities, and 1904 primary healthcare facilities).
16 In this study, residents living in rural areas participated less in DSME compared to those living in urban areas. Moreover, rural residents were 0.74 times less likely to engage in DSME at HMCs and 1.73 times more likely to attend DSME at PHIs. Since the proportion of people engaging in DSME at HMCs (23.2%) was approximately four times higher than that at PHIs (5.3%), the overall rate of participation in rural areas was significantly lower than that in urban areas, since most PHIs in Korea are located in rural areas. Among PHIs in Korea, there is one health center in each municipal-level administrative division (city, county, and district). Nonetheless, primary healthcare facilities (sub-health centers and primary healthcare posts) are located predominantly in rural areas (eup – myeon) across counties, which are vulnerable areas for medical services. Therefore, 93.5% of PHIs are distributed mainly in rural areas.
16 Although the development of DSME programs at PHIs helps close the educational gap in rural and urban areas, the overall enrollment in DSME in rural areas is significantly lower than that in urban areas, since the proportion of PHIs in healthcare institutions is very small (9.5%).
Among the occupational groups, service/sales worker and manual worker groups engaged less in DSME. Agricultural/forestry/fishery worker group participated less in DSME at HMCs and more at PHIs (borderline significance). There were no significant differences in the attendance between agricultural/forestry/fishery worker and professional/managerial worker (reference) groups. Most (94.9%) of the agricultural/forestry/fishery workers lived in rural areas. Therefore, expanding DSME at both HMCs and PHIs located in rural areas is crucial to reduce the disparity in participation by region and occupation.
Comprehensive community education programs should be improved and expanded at HMCs and PHIs. In addition, diabetes education programs can be developed in the evenings and weekends to increase attendance by socioeconomically disadvantaged individuals with diabetes.
12 The use of technology enables the rapid development of person-centered interventions that support self-management to improve access to education, especially for rural residents and people with low socioeconomic status.
1718 A recent review article demonstrated that utilizing technology-enabled DSME significantly improved health outcomes.
17 In addition, physician recommendation or encouragement may increase attendance at DSME.
1920 Receiving regular primary care was the strongest predictor of participation in DSME, suggesting that DSME is not a substitute for diabetes treatment for people without a regular primary care physician.
21
The present study showed that 27.2% of people with diabetes participated in DSME, which is lower than that in countries that provide reimbursement of costs for DSME by insurance. According to the Behavioral Risk Factor Surveillance System in the United States,
12 more than half (53.7%) of people with diabetes reported engaging in DSME, among whom those without health insurance had a significantly lower DSME participation rate. A population-based study in Germany showed that 47% of type 2 diabetes patients participated in DSME.
22 In Ontario, Canada, 30% of survey participants reported attending a diabetes education center.
21 In countries like the United States and Germany, DSME for diabetes patients is an insurance benefit covered by both public and private health insurance services, since data indicate that the education of diabetes patients can reduce diabetes-related social costs. Reimbursement for DSME costs in the United States is available through the Centers for Medicare and Medicaid Services (CMS) and most private insurances policies, if the DSME program meets the standards set by a CMS-designed national accreditation organization. In Germany, diabetes education is fully compensated by German statutory health insurance. In Canada, in addition to medical treatment, health insurance benefits apply to both education and counselling. This means that patients with diabetes can receive integrated care from team-based health resources, including dieticians, nurses, and educators. Health insurance coverage is an important factor affecting diabetes education.
1223 Therefore, in Korea, DSME should be reimbursed by the Korea National Health Insurance system to improve the healthcare of people with diabetes, and to reduce complications and costs.
There is one problem that must be discussed. Hypoglycemia is a common complication in both type 2 and type 1 diabetes patients that has serious clinical, social, and economic consequences, the frequency of which is likely to increase with the increasing prevalence of diabetes.
24 Our results have shown that more than half (54.3%) of the people with diabetes using insulin do not participate in DSME. Since insulin users have a much higher risk of developing hypoglycemia,
25 the lack of DSME participation among insulin users can be particularly dangerous. Careful titration of insulin therapy can achieve good glycemic control without the risk of hypoglycemia.
26 Mitigation of hypoglycemic risks should include strategies for raising awareness of risks and prevention through education of patients and families. It is also important to take hypoglycemic risks into account when selecting medications and therapies for individual patients.
27
This study had some limitations. First, the study's cross-sectional design did not allow for establishing a causal relationship. Second, the type of educators (doctors, nurses, or other specialists) and type of education (individual or group) were not identified,
28 which limited the analysis of differences in sociodemographic factors according to the type of DSME. Third, recall bias may have affected the results, since information about enrollment in DSME was self-reported. Despite these limitations, our study had several strengths. First, data from a national survey were analyzed to study a large sample of community-based adults with diabetes. Second, several sociodemographic factors that could affect attendance at DSME were assessed to identify disparities in participation. Third, both the percentage of participation in DSME programs and type of institution providing these programs were determined to identify inequalities between institutions.
In conclusion, the rate of participation in DSME among community-dwelling adults with diabetes was 27.2%, including 21.9% at HMCs, 4.0% at PHIs, and 1.3% at both types of institution. Overall, older age, living in rural areas, lower education level, lower household income, and type of occupation were significantly correlated with lower participation in this program. DSME is a useful tool for managing diabetes, and it has been shown to improve health status, clinical outcomes, and the quality of life of patients. DSME implementation strategies that take into account the differences in regional characteristics and the distribution of medical care institutions in urban and rural areas are needed. In urban areas, DSME is needed for middle-aged and elderly, low-educated, and low-income people with diabetes, and it could be provided by actively utilizing HMCs. On the other hand, in rural areas, HMCs and PHIs should work together to provide DSME, especially for people with low level of education. Therefore, customized DSME programs targeting socioeconomically vulnerable groups, including residential region and reimbursement of DSME by public insurance, are needed to solve the inequalities in participation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download