Abstract
Atrial fibrillation (AF) is responsible for 10–20% of cerebral infarctions. Several mobile devices have been developed to screen for AF and studies of AF screening have been conducted in several countries to evaluate the applicability of these mobile devices. In this tradition, we conducted a community-based AF screening using an automated single-lead electrocardiogram (SL-ECG). This survey examined 2,422 participants in a community dementia screening program who were aged 60 years or older in the preliminary study, and 5,366 participants at 9 Senior Welfare Centers aged 60 years or older in the expanded study. AF screening was conducted using an automated SL-ECG (Kardia Mobile, AliveCor, Mountain View, CA, USA). AF was confirmed with a 12-lead electrocardiogram in subjects classified as having AF on the SL-ECG. In the preliminary study, of the 2,422 subjects, 124 had AF on the SL-ECG. The prevalence of AF was 3.0% (95% confidence interval [CI]: 2.4–3.8). The positive predictive value (PPV) of SL-ECG was 58.9% (95% CI: 50.1–67.1). Of the subjects diagnosed with AF, 65.8% (95% CI: 54.3–75.6) were newly diagnosed. In an expanded study, of the 5,366 subjects, 289 had AF on SL-ECG. The prevalence was 2.6% (95% CI: 2.2–3.1) and PPV of SL-ECG was 48.8% (95% CI: 43.1–54.5). In this community-based AF screening, we found that AF is underdiagnosed and undertreated. These results suggest that the early detection of AF using mobile devices is needed in Korea.
Although stroke mortality has declined rapidly over the past 20 years, stroke is still the third most common cause of death in Korea.1 There are two kinds of stroke: cerebral hemorrhage and cerebral infarction. Three-quarters of stroke patients have cerebral infarction, and atrial fibrillation (AF) is responsible for 10–20% of these kinds of strokes. In Korea, 3.1–7.6% of patients with AF develop strokes each year.2 In addition, the prevalence of AF is 2.35% in men and 1.71% in women aged ≥60 years, and the incidence of AF increases by 1.5 to 2 times with each decade.3 Oral anticoagulants (OAC) have been found to reduce the risk of cerebral infarction by about 70%.4 Therefore, the early detection and treatment of patients with AF is a good way to reduce the burden of AF-related diseases.
Several mobile devices have been developed to screen for AF. These devices diagnose AF using pulse irregularity or rhythm analysis of a single-lead electrocardiogram (SL-ECG). The emergence of mobile devices capable of diagnosing AF is providing an opportunity to re-evaluate AF screening. Recently, the National Institute for Health and Clinical Excellence (NICE) recommended an automatic blood pressure monitor for the early detection of AF.5 Studies of AF screening have been conducted in other countries to evaluate the applicability of these mobile devices,678 however, the use of AF screening with mobile devices has not yet been evaluated in Korea. Therefore, we conducted a community-based AF screening using a SL-ECG.
In the preliminary study, 2,422 individuals who participated in a community dementia screening program in Dong-gu, Metropolitan Gwangju and were aged 60 years or older were screened for AF between April and June 2017. In the expanded study, the screening program was expanded to five districts, 5,366 individuals aged 60 years were screened for AF. Between April and September 2018, the expanded screening program was conducted at two Senior Welfare Centers in Gwangsan-gu and Buk-gu, three centers in Nam-gu, and one center in Dong-gu and Seo-gu.
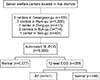
Subjects underwent AF screening using the Kardia Mobile (AliveCor, Mountain View, CA, USA) (Fig. 1). This SL-ECG consists of a pair of electrodes and records lead I in the 12-lead ECG. When one finger of each hand is placed on each electrode, the ECG is recorded for about 40 seconds and immediately reports the ECG results as ‘Normal’, ‘AF’, or ‘Unclassified’. A 12-lead ECG was performed within 20 minutes for the subjects identified as having AF on the Kardia Mobile, and all 12-lead ECGs were reviewed by a cardiologist. Treatment of the AF was recommended for the newly diagnosed AF patients and, 1 month later, they were interviewed by telephone to determine whether they had visited a clinic or hospital for treatment of the AF. Figs. 2 and 3 are flow charts of the study design.
In the preliminary study, information on lifestyles and medical history was obtained in a face-to-face interview using a structured questionnaire. Smoking history was coded as never, ex-smoker, and current smoker. Alcohol consumption was coded as non-drinker and current drinker. Medical history included hypertension, diabetes, hyperlipidemia, thyroid disease, angina pectoris, myocardial infarction, AF, heart failure, valvular heart disease, transient ischemic stroke, cerebral infarction, cerebral hemorrhage, and peripheral artery disease. However, in the expanded study, this information was not collected.
The general characteristics of the subjects are presented according to the presence or absence of AF. Continuous variables are reported as the mean±standard deviation and categorical variables as the number (proportion). The t-test was used to compare continuous variables, and the chi-square test was used for categorical variables. All analyses were performed using R ver. 3.5.1 (The R Foundation for Statistical Computing, Vienna, Austria).
In the preliminary study, of the 2,422 subjects, 2,140 were normal, 158 were unclassified, and 124 had AF on the SL-ECG. Of the latter 124, 73 (58.9%, 95% confidence interval [CI]: 50.1–67.1) were confirmed to have AF on the 12-lead ECG, 32 (25.8%) were in normal sinus rhythm, 9 (7.3%) had premature ventricular contractions, 7 (5.6%) had premature atrial contractions, 2 (1.6%) had right bundle branch block, and 1 (0.8%) had sinus arrhythmia. Of the 48 newly diagnosed AF patients, 29 (60.4%) underwent treatment. The prevalence of AF was 3.0% (95% CI: 2.4–3.8) and PPV of the SL-ECG was 58.9% (95% CI: 50.1–67.1) (Fig. 2). In the expanded study, of the 5,366 subjects, 289 had AF on the SL-ECG. Of those, 141 (48.8%, 95% CI: 43.1–54.5) were confirmed to have AF on the 12-lead ECG. The prevalence was 2.6% (95% CI: 2.2–3.1) and PPV was 48.8% (95% CI: 43.1–54.5) (Fig. 3).
Table 1 presents the baseline characteristics of participants according to AF status. Compared to the group without AF, the group with AF included a higher proportion of males, was older, had a higher prevalence of heart failure and valvular heart disease, and had a lower prevalence of smokers.
Fig. 4 shows the prevalence of AF according to age and sex. The prevalence of AF was higher in males and increased with age. The prevalence of AF was 4.5% in males and 2.3% in females. The prevalence of AF in men in their 60s, 70s, and 80s were 1.9%, 4.6%, and 6.3%, respectively, compared with 0.9%, 2.4%, and 4.4%, respectively, in women.
This study found that the prevalence of AF in Korean adults aged 60 years or more was 3.0%, and 65.7% of the subjects with AF were newly diagnosed. In our study, the predictive positive value (PPV) of the Kardia Mobile Heart Monitor was 58.9% (95% CI: 50.1–67.1). In the expanded study, the prevalence was 2.6% (95% CI: 2.2–3.1) and PPV was 48.8% (95% CI: 43.1–54.5). To our knowledge, this study was the first AF screening using an automated SL-ECG in Koreans. AF screening using the Kardia Mobile Heart Monitor was applicable in the community setting. In the preliminary study, in combination with a well-established community dementia screening program, AF screening programs could be efficiently implemented for residents aged 60 and older. In addition, in the expanded study, we were able to show that AF screening can be performed efficiently based on the elderly facilities throughout a metropolitan area.
The underdiagnosis of AF has been reported in different populations. The proportion of subjects newly diagnosed with AF at a screening in previous studies was 30.3–66.2%.8910 In our study, 65.8% of the AF patients were newly diagnosed by the screening. Given that paroxysmal AF can be significantly underdiagnosed in a single measurement,111213 AF is likely to be underdiagnosed much more often than reported here.
In previous studies, 20.3–34.2% of AF patients were treated with OAC.69 However, in a study population with high socioeconomic status, 85% of the AF patients were treated with OAC.12 In our study, 55.2% of the 29 patients with a history of AF were treated with OAC, which was higher than the 46% treatment rate reported by a study using data from the Korean National Health Insurance Service. 14 The reason for this difference is that our study population consisted of subjects voluntarily participating in a dementia screening program at the public health office.
In this study, 48 patients with newly diagnosed AF were advised to have the AF treated, and 29 of the 48 (60.4%) patients were treated within 1 month. Similar to our study, 60% of the people diagnosed with AF were prescribed OAC in a screening program for adults aged 65 years or older who visited pharmacies.6 By contrast, in the STROKESTOP study, 93% of the people newly diagnosed with AF were prescribed OAC.15 The treatment rate in the STROKESTOP study was likely high because the AF patients diagnosed at the screening center in the hospital were referred directly to a cardiologist.
In this study, the PPV of SL-ECG was 58.9%, which was lower than that of previous studies. Chan et al.7 and Chan et al.8 reported PPVs of 64.9% and 77.2%, respectively. This difference in PPV may be due to differences in the method of confirmation of AF. In these two previous studies, atrial fibrillation was confirmed by reviewing the SL-ECG stored at the screening by a cardiologist. However, in this study, a cardiologist confirmed AF with a 12-lead ECG measured after SL-ECG. Due to the time interval between the measurement of SL-ECG and the measurement of the 12-lead ECG, some paroxysmal atrial fibrillation may not have been diagnosed.
This study had several limitations. First, the validity of the SL-ECG was not assessed fully because the 12-lead ECG was performed only on the subjects in whom the SLECG detected AF. However, some studies have reported that Kardia Mobile Heart Monitor's detection rates are acceptable. Lau et al.16 and Lowres et al.6 reported that the sensitivity was 98% and 98.5%, and the specificity was 97% and 91.4%. Second, asymptomatic paroxysmal AF may not have been diagnosed because AF was diagnosed with a single measurement.17 Third, the benefit of AF screening was not evaluated fully in our study. The decrease in cerebrovascular mortality or incidence of stroke attributable to the screening program could not be evaluated due to the limitations of the study's design. Additionally, the cost-effectiveness of the AF screening was not evaluated. Some studies have reported that AF screening is cost-effective,610 but the cost-effectiveness should be reassessed in the Korean medical setting.
In conclusion, we showed that AF screening was applicable to Korean adults. Of the subjects diagnosed with AF, 65.8% were newly diagnosed. Because AF is underdiag-nosed in Korea and nearly half of AF patients are not adequately treated, early detection and treatment of AF are needed. Future research should determine the appropriate interval between screenings, the groups at high risk for this condition, and the cost-effectiveness of AF screening.
Figures and Tables
FIG. 2
Flow chart of the preliminary study. SL-ECG: single-lead electrocardiogram, AF: atrial fibrillation, NSR: normal sinus rhythm, PVC: premature ventricular contractions, PAC: premature atrial contractions, RBBB: right bundle branch block.

References
1. Vital Statistics Division, Statistics Korea. Shin HY, Lee JY, Kim JE, Lee S, Youn H, et al. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018; 61:573–584.

2. Son MK, Lim NK, Kim HW, Park HY. Risk of ischemic stroke after atrial fibrillation diagnosis: a national sample cohort. PLoS One. 2017; 12:e0179687.

3. Son MK, Lim NK, Park HY. Trend of prevalence of atrial fibrillation and use of oral anticoagulation therapy in patients with atrial fibrillation in South Korea (2002-2013). J Epidemiol. 2018; 28:81–87.



4. Jonas DE, Kahwati LC, Yun JDY, Middleton JC, Coker-Schwimmer M, Asher GN. Screening for atrial fibrillation with electrocardiography: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018; 320:485–498.


5. Willits I, Keltie K, Craig J, Sims A. WatchBP Home A for opportunistically detecting atrial fibrillation during diagnosis and monitoring of hypertension: a NICE Medical Technology Guidance. Appl Health Econ Health Policy. 2014; 12:255–265.



6. Lowres N, Neubeck L, Salkeld G, Krass I, McLachlan AJ, Redfern J, et al. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. The SEARCH-AF study. Thromb Haemost. 2014; 111:1167–1176.


7. Chan PH, Wong CK, Poh YC, Pun L, Leung WW, Wong YF, et al. Diagnostic performance of a smartphone-based photoplethysmographic application for atrial fibrillation screening in a primary care setting. J Am Heart Assoc. 2016; 5:e003428.

8. Chan NY, Choy CC, Chan CK, Siu CW. Effectiveness of a nongovernmental organization-led large-scale community atrial fibrillation screening program using the smartphone electrocardiogram: an observational cohort study. Heart Rhythm. 2018; 15:1306–1311.


9. Meschia JF, Merrill P, Soliman EZ, Howard VJ, Barrett KM, Zakai NA, et al. Racial disparities in awareness and treatment of atrial fibrillation: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2010; 41:581–587.



10. Proietti M, Mairesse GH, Goethals P, Scavee C, Vijgen J, Blankoff I, et al. A population screening programme for atrial fibrillation: a report from the Belgian Heart Rhythm Week screening programme. Europace. 2016; 18:1779–1786.


11. Engdahl J, Andersson L, Mirskaya M, Rosenqvist M. Stepwise screening of atrial fibrillation in a 75-year-old population: implications for stroke prevention. Circulation. 2013; 127:930–937.


12. Tveit A, Abdelnoor M, Enger S, Smith P. Atrial fibrillation and antithrombotic therapy in a 75-year-old population. Cardiology. 2008; 109:258–262.


13. Fitzmaurice DA, Hobbs FD, Jowett S, Mant J, Murray ET, Holder R, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ. 2007; 335:383.

14. Lee SR, Choi EK, Han KD, Cha MJ, Oh S, Lip GYH. Temporal trends of antithrombotic therapy for stroke prevention in Korean patients with non-valvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants: a nationwide population-based study. PLoS One. 2017; 12:e0189495.

15. Svennberg E, Engdahl J, Al-Khalili F, Friberg L, Frykman V, Rosenqvist M. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Circulation. 2015; 131:2176–2184.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download