1. Morisseau C, Hammock BD. Annu Rev Pharmacol Toxicol. 2013; 53:37–58.
2. Morisseau C, Inceoglu B, Schmelzer K, Tsai HJ, Jinks SL, Hegedus CM, Hammock BD. J Lipid Res. 2010; 51:3481–3490.
3. Lin WK, Falck JR, Wong PY. Biochem Biophys Res Commun. 1990; 167:977–981.
4. Inceoglu B, Jinks SL, Schmelzer KR, Waite T, Kim IH, Hammock BD. Life Sci. 2006; 79:2311–2319.
5. Yu Z, Xu F, Huse LM, Morisseau C, Draper AJ, Newman JW, Parker C, Graham L, Engler MM, Hammock BD, Zeldin DC, Kroetz DL. Circ Res. 2000; 87:992–998.
6. Kim JH, Tai BH, Yang SY, Kim JE, Kim SK, Kim YH. Bull Korean Chem Soc. 2015; 36:300–304.
7. Kim JH, Cho CW, Tai BH, Yang SY, Choi GS, Kang JS, Kim YH. Molecules. 2015; 20:21405–21414.
8. Jo AR, Kim JH, Yan XT, Yang SY, Kim YH. J Enzyme Inhib Med Chem. 2016; 31:70–78.
9. Lee GY, Kim JH, Choi SK, Kim YH. Bioorg Med Chem Lett. 2015; 25:5097–5101.
10. Kim JH, Morgan AMA, Tai BH, Van DT, Cuong NM, Kim YH. J Enzyme Inhib Med Chem. 2016; 31:640–644.
11. Khanh PN, Duc HV, Huong TT, Son NT, Ha VT, Van DT, Tai BH, Kim JE, Jo AR, Kim YH, Cuong NM. Fitoterapia. 2016; 109:39–44.
12. Thokchom R, Mandal GJ. Agric Eng Food Technol. 2017; 4:27–30.

13. Beninca JP, Montanher AB, Zucolotto SM, Schenkel EP, Frode TS. Food Chem. 2007; 104:1097–1105.
14. Ichimura T, Yamanaka A, Ichiba T, Toyokawa T, Kamada Y, Tamamura T, Maruyama S. Biosci Biotechnol Biochem. 2006; 70:718–721.
15. Lourith N, Kanlayavattanakul M. J Oleo Sci. 2013; 64:235–240.
16. Puricelli L, Dell'Aica I, Sartorb L, Garbisa S, Caniato R. Fitoterapia. 2003; 74:302–304.
17. Coleta M, Campos MG, Cotrim MD, Proenca da. Pharmacopsychiatry. 2001; 34:S20–S21.
18. Pelegrini PB, Noronha EF, Muniz MA, Vasconcelos IM, Chiarello MD, Oliveira JT, Franco OL. Biochim Biophys Acta. 2006; 1764:1141–1146.
19. Matsui Y, Sugiyama K, Kamei M, Takahashi T, Suzuki T, Katagata Y, Ito T. J Agric Food Chem. 2010; 58:11112–11118.
20. Bombardelli E, Bonati A, Gabetta B, Martinelli EM, Mustich G, Danieli G. Phytochemisty. 1975; 14:2661–2665.
21. Mareck U, Herrmann K, Galensa R, Wray V. Phytochemistry. 1991; 30:3486–3487.
22. Seigler DS, Pauli GF, Nahrstedt A, Leen R. Phytochemistry. 2002; 60:873–882.
23. Pereira CA, Yariwake JH, Lancas FM, Wauters JN, Tits M, Angenot L. Phytochem Anal. 2004; 15:241–248.
24. Sano S, Sugiyama K, Ito T, Katano Y, Ishihata A. J Agric Food Chem. 2011; 59:6209–6213.
25. Piombo G, Barouh N, Barea B, Boulanger R, Brat P, Pina M, Villeneuve P. OCL. 2006; 13:195–199.
26. Mattivi F, Reniero F, Korhammer S. J Agric Food Chem. 1995; 43:1820–1823.
27. Mathi P, Das S, Nikhil K, Roy P, Yerra S, Ravada SR, Bokka VR, Botlagunta M. Int J Prev Med. 2015; 6:101.
28. Kukreja A, Wadhwa N, Tiwari A. J Blood Disord Transfus. 2014; 5:240.
29. Gaur R, Kumar S, Trivedi P, Bhakuni RS, Bawankule DU, Pal A, Shanker K. Nat Prod Commun. 2010; 5:1243–1246.
30. Júnior GMV, Sousa CMM, Cavalheiro AJ, Lago JHG, Chaves MH. Helv Chim Acta. 2008; 91:2159–2167.
31. Lee DS, Jeong GS, Li B, Park H, Kim YC. Int Immunopharmacol. 2010; 10:850–858.
32. Lee KW, Chung KS, Seo JH, Yim SV, Park HJ, Choi JH, Lee KT. J Cell Biochem. 2012; 113:2835–2844.
33. Pariyar R, Lamichhane R, Jung HJ, Kim SY, Seo J. Int J Mol Sci. 2017; 18:E2753.
34. Li JL, Li N, Xing SS, Zhang N, Li BB, Chen JG, Ahn JS, Cui L. Arch Pharm Res. 2017; 40:1265–1270.
35. Esposito T, Sansone F, Franceschelli S, Del Gaudio P, Picerno P, Aquino RP, Mencherini T. Int J Mol Sci. 2017; 18:E392.
36. Boğa M, Yilmaz PK, Cebe DB, Fatima M, Siddiqui BS, Kolak U. Z Naturforsch C J Biosci. 2014; 69:381–390.
37. Lim SY, Subedi L, Shin D, Kim CS, Lee KR, Kim SY. Biomol Ther. 2017; 25:519–527.
38. Baba K, Kido T, Taniguchi M, Kozawaqa M. Phytochemistry. 1994; 36:1509–1513.
39. Bunluepuech K, Wattanapiromsakul C, Tewtrakul S. Songklanakarin J Sci Technol. 2013; 35:665–669.
40. Tran HHT, Nguyen MC, Le HT, Nguyen TL, Pham TB, Chau VM, Nguyen HN, Nguyen TD. Pharm Biol. 2014; 52:74–77.
41. Yuenyongsawad S, Bunluepuech K, Wattanapiromsakul C, Tewtrakul S. Songklanakarin J Sci Technol. 2014; 36:189–194.
42. Buscató E, Büttner D, Brüggerhoff A, Klingler FM, Weber J, Scholz B, Zivković A, Marschalek R, Stark H, Steinhilber D, Bode HB, Proschak E. ChemMedChem. 2013; 8:919–923.
43. Sun YN, Li W, Kim JH, Yan XT, Kim JE, Yang SY, Kim YH. Arch Pharm Res. 2015; 38:998–1004.
44. Broadwell RD, Sofroniew MV. Exp Neurol. 1993; 120:245–263.
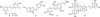
 +16.3° (c 0.05, MeOH); 1H-NMR (500MHz, Methanol-d4) δH: 9.60 (1H, d, J = 8.0 Hz, H-9′), 7.61 (1H, d, J = 15.5 Hz, H-7′), 7.31 (1H, s, H-6′), 7.25 (1H, s, H-2′), 6.97 (1H, s, H-2), 6.85 (1H, d, J = 8.0 Hz, H-5), 6.80 (1H, d, J = 8.0, H-6), 6.70 (1H, dd, J = 15.5, 8.0 Hz, H-8′), 5.63 (1H, d, J = 6.5 Hz, H-7), 3.92 (3H, s, 3′-OCH3), 3.91-3.87 (2H, m, H-9), 3.84 (3H, s, 3-OCH3), 3.59 (1H, q, J = 6.5 Hz, H-8); 13C-NMR (125 MHz, Methanol-d4) δC (ppm): 196.1 (C-9′), 156.8 (C-4′), 156.1 (C-3′), 152.9 (C-4), 149.2 (C-3), 146.0 (C-7′), 133.9 (C-1), 131.3 (C-5), 129.6 (C-1′), 127.1 (C-8′), 120.0 (C-6), 119.8 (C-6′), 116.2 (C-5), 114.3 (C-2′), 110.6 (C-2), 90.1 (C-7), 64.5 (C-9), 56.8 (3-OCH3), 56.4 (3′-OCH3), 54.6 (C-8); ESI-MS m/z: 357.14 [M+H]+ (Calcd. for C20H20O6).
+16.3° (c 0.05, MeOH); 1H-NMR (500MHz, Methanol-d4) δH: 9.60 (1H, d, J = 8.0 Hz, H-9′), 7.61 (1H, d, J = 15.5 Hz, H-7′), 7.31 (1H, s, H-6′), 7.25 (1H, s, H-2′), 6.97 (1H, s, H-2), 6.85 (1H, d, J = 8.0 Hz, H-5), 6.80 (1H, d, J = 8.0, H-6), 6.70 (1H, dd, J = 15.5, 8.0 Hz, H-8′), 5.63 (1H, d, J = 6.5 Hz, H-7), 3.92 (3H, s, 3′-OCH3), 3.91-3.87 (2H, m, H-9), 3.84 (3H, s, 3-OCH3), 3.59 (1H, q, J = 6.5 Hz, H-8); 13C-NMR (125 MHz, Methanol-d4) δC (ppm): 196.1 (C-9′), 156.8 (C-4′), 156.1 (C-3′), 152.9 (C-4), 149.2 (C-3), 146.0 (C-7′), 133.9 (C-1), 131.3 (C-5), 129.6 (C-1′), 127.1 (C-8′), 120.0 (C-6), 119.8 (C-6′), 116.2 (C-5), 114.3 (C-2′), 110.6 (C-2), 90.1 (C-7), 64.5 (C-9), 56.8 (3-OCH3), 56.4 (3′-OCH3), 54.6 (C-8); ESI-MS m/z: 357.14 [M+H]+ (Calcd. for C20H20O6). −56.4° (c 0.12, MeOH); 1H-NMR (500 MHz, Methanol-d4) δH (ppm): 7.15 (1H, d, J = 2.0 Hz, H-2), 7.09 (1H, dd, J = 8.5, 2.0 Hz, H-6), 6.99 (1H, d, J = 16.0 Hz, H-7), 6.96 (1H, d, J = 8.5 Hz, H-5), 6.88 (1H, d, J = 16.0 Hz, H-8), 6.68 (1H, d, J = 2.0 Hz, H-2′), 6.67 (1H, d, J = 8.5 Hz, H-5′), 6.50 (1H, dd, J = 8.5, 2.0 Hz, H-6′), 6.48 (2H, overlap, H-12/H-12′), 6.19 (1H, t, J = 2.0 Hz, H-14′), 6.17 (1H, t, J = 2.0 Hz, H-10′), 6.12 (2H, d, J = 2.0 Hz, H-10/H-14), 4.75 (2H, d, J = 2.5 Hz, H-7′/H-8′); 13C-NMR (125 MHz, Methanol-d4) δC (ppm): 159.6 (C-11/C-11′), 159.2 (C-13/C-13′), 146.6 (C-4′), 146.1 (C-3′), 145.4 (C-4), 145.0 (C-3), 141.0 (C-9), 140.1 (C-9′), 132.6 (C-1), 129.4 (C-7), 129.0 (C-1′), 128.4 (C-8), 121.0 (C-6′), 120.7 (C-6), 118.1 (C-5), 115.9 (C-2), 115.8 (C-5′), 115.6 (C-2′), 107.4 (C-10′/C-14′), 105.9 (C-10/C-14), 103.6 (C-12′), 102.9 (C-12), 82.2 (C-8′), 81.8 (C-7′); ESI-MS m/z: 487.13 [M+H]+ (Calcd. for C28H22O8).
−56.4° (c 0.12, MeOH); 1H-NMR (500 MHz, Methanol-d4) δH (ppm): 7.15 (1H, d, J = 2.0 Hz, H-2), 7.09 (1H, dd, J = 8.5, 2.0 Hz, H-6), 6.99 (1H, d, J = 16.0 Hz, H-7), 6.96 (1H, d, J = 8.5 Hz, H-5), 6.88 (1H, d, J = 16.0 Hz, H-8), 6.68 (1H, d, J = 2.0 Hz, H-2′), 6.67 (1H, d, J = 8.5 Hz, H-5′), 6.50 (1H, dd, J = 8.5, 2.0 Hz, H-6′), 6.48 (2H, overlap, H-12/H-12′), 6.19 (1H, t, J = 2.0 Hz, H-14′), 6.17 (1H, t, J = 2.0 Hz, H-10′), 6.12 (2H, d, J = 2.0 Hz, H-10/H-14), 4.75 (2H, d, J = 2.5 Hz, H-7′/H-8′); 13C-NMR (125 MHz, Methanol-d4) δC (ppm): 159.6 (C-11/C-11′), 159.2 (C-13/C-13′), 146.6 (C-4′), 146.1 (C-3′), 145.4 (C-4), 145.0 (C-3), 141.0 (C-9), 140.1 (C-9′), 132.6 (C-1), 129.4 (C-7), 129.0 (C-1′), 128.4 (C-8), 121.0 (C-6′), 120.7 (C-6), 118.1 (C-5), 115.9 (C-2), 115.8 (C-5′), 115.6 (C-2′), 107.4 (C-10′/C-14′), 105.9 (C-10/C-14), 103.6 (C-12′), 102.9 (C-12), 82.2 (C-8′), 81.8 (C-7′); ESI-MS m/z: 487.13 [M+H]+ (Calcd. for C28H22O8).



 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download