METHODS
Study population and data collection
We used and analyzed the data of the Korean PCI (K-PCI) registry. The K-PCI registry is a retrospective multicenter registry of coronary artery disease (CAD) patients treated with PCI enrolled from 92 hospitals in Korea. This study was an all-comer registry without specific exclusion criteria. Data on the baseline medical history, laboratory findings, medications, revascularization procedures and in-hospital outcome were collected by a trained study coordinator using a standardized case report form and web-based reporting system. This registry was co-sponsored by the Korean Society of Interventional Cardiology and the Korean Society of Cardiology. A total of 44,967 patients were finally enrolled in this registry from January 2014 through December 2014. Among the total population from this registry, we analyzed 8,282 patients with STEMI treated with primary PCI. A total of 373 operators who performed primary PCI were analyzed in this study.
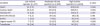
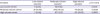
The study population was divided into 3 groups according to operator volume: high-volume operators (n=4,509), moderate-volume operators (n=3,302), and low-volume operators (n=471). We divided operator volume into high, moderate, and low-volume operators, respectively according to the operators with annual primary PCI volumes above 30 cases (n=93) (above the 75th percentile), between 10 and 30 cases (n=180) (between the 75th percentile and 25th percentile), and less than 10 cases (n=100) (less than the 25th percentile).
The study protocol conforms to the ethical guideline of the 1975 Declaration of Helsinki. The Institutional Review Board (IRB No. 2015-10-026-006) at each participant hospital approved this study and waived the requirement for patient-informed consent because of the study's retrospective nature.
PCI procedure
Primary PCI is the immediate revascularization procedure for patients with STEMI within 12 hours from symptom onset, or the PCI for patients with any symptoms of recurrent or persistent ischemia, symptoms of heart failure, or electrical instability more than 12 hours after symptom onset. The PCI procedures were performed using the current conventional technique. Artery access sites for PCI and type of stent depended on the discretion of the attending physicians.
Definition and study outcomes
STEMI was defined as persistent chest discomfort or other symptoms suggestive of acute ischemia and ST-segment elevation in at least 2 contiguous leads or new onset left bundle branch block not documented to be resolved within 20 minutes were defined as STEMI.
10) ST-segment elevation was defined by new or presumed new sustained ST-segment elevation at the J-point in 2 contiguous electrocardiogram (ECG) leads with the cut-off points: ≥0.2 mV in men or ≥0.15 mV in women in leads V2-V3 and/or ≥0.1 mV in other leads and lasting greater than or equal to 20 minutes. The definition of STEMI included patients whose cardiac biomarkers (CK-MB, Troponin T or I) exceeded the upper limit of normal according to the individual hospital's laboratory parameters together with a clinical presentation which was consistent with or suggestive of acute ischemia.
The primary endpoint was major adverse cardiovascular and cerebrovascular events (MACCEs) during hospitalization, defined as a composite of cardiac death, MI, stent thrombosis or stroke, based on Academic Research Consortium.
12) Cardiac death was defined as any death due to proximate cardiac cause, such as MI, low-output failure, or fatal arrhythmia. Deaths without an explicable non-cardiac cause were considered cardiac death. MI was indicated by the new occurrence of a biomarker elevation after PCI: the prost-procedure cardiac troponin must rise by >20% following new ischemic ECG changes.
13) Stent thrombosis was defined as the presence of a thrombus that originated in the stent or in the segment 5 mm proximal or distal to the stent and the presence of at least 1 of the following criteria within a 48-hour time window: 1) acute onset of ischemic symptom(s) at rest, 2) new ischemic ECG changes that suggest acute ischemia, and 3) typical rise and fall in cardiac biomarkers. Stroke was defined as a sudden focal neurologic deficit of presumed cerebrovascular etiology that persisted beyond 24 hours and was not due to another identifiable cause.
The secondary endpoints were adverse in-hospital outcomes defined as composed of primary endpoint and all-cause mortality, urgent repeat PCI, and transfusion of whole blood or packed red blood cells. Urgent repeat PCI was defined as necessity for repeat procedure due to PCI complications or hemodynamic instability.
Statistical analysis
Baseline characteristics and angiographic/procedural data are expressed as number (%) for categorical data or mean±standard deviation for continuous data. Continuous variables were compared using Student's t-test, analysis of variance, and comparisons of categorical data were performed using the χ2 test (or Fisher's exact). We calculated odds ratio (OR) for MACCE among the 3 groups using multivariate logistic-regression analyses. To reduce the impact of differences in baseline characteristics, we adjusted confounding factors, such as age, sex, hypertension, diabetes, family history of premature CAD, prior PCI, and renal failure. Inverse probability weighted (IPW) analysis was also performed to adjust for baseline differences between the 3 groups. Statistical analyses were performed with SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). The p value<0.05 was considered statistically significant.
DISCUSSION
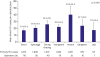
Our study is the first representative study to analyze in-hospital outcomes after primary PCI for STEMI patients in Korea. One important aspect of this study was the determination of the geographic differences in mean primary PCI cases by operator and of the relationship between clinical outcome and operator volume. The major findings are as follows: 1) baseline characteristics, such as age distribution, renal failure, reduced LVEF, and cardiac arrest before PCI, were significantly different depending on operator volume, 2) PCI techniques, such as trans-radial approach and IVUS usage, showed significant differences between groups of operators with varying experience, and 3) operator volume was not associated with MACCEs and in-hospital adverse outcomes.
Current international and national guidelines recommend a certain minimum operator PCI volume. American College of Cardiology Foundation/American Heart Association/Society for Cardiovascular Angiography and Interventions guideline recommended primary PCI for STEMI should be performed by experienced operators who perform at least 11 PCI procedures for STEMI per year.
6) The European Society of Cardiology/European Association of PCI guidelines recommended minimum 75 procedures per year for operator volume, but there was no definite minimum number of recommended primary PCI.
7) However, the evidence of any relationship between volume of procedures and outcomes of primary PCI at operator level was limited. One previous study on the volume-outcome relationship for PCI in the stent era reported that higher-volume (with an operator volume threshold of 75) was associated with better risk-adjusted PCI outcomes.
1) However, this data was derived from the period when bare metal stents were widely used. Another study using the New York State PCI registry evaluated the relationship between volume and outcomes focusing on primary PCI.
14) In this study, the positive relationship between operator volumes and better clinical outcomes was only observed in the case of high-volume operators. However, this data was also based on the 2000 to 2002 PCI reporting system, before current generation thin strut DES were introduced. This study categorized physician volume categories into ≤10 cases/year, 10 to 20 cases/year, and >20 cases/year, respectively.
14) However, our data showed average primary PCIs performed by 373 operators was 22.2 cases, which might be categorized as high-operator volume according to previous research criteria. It is important for us to define a new operator volume classification, because most of the data available on the relationship between operator volume and outcomes was from the early generation stent era in the Western population. Our study offers the new practical categorization in Korean interventional cardiology, which splits the patient cohort into: primary PCI operator volume above the 75th percentile (>30 cases), between the 75th percentile and 25th percentile (10–30 cases), and less than 25th percentile (<10 cases), respectively. Our data showed geographic differences in primary PCI cases, which were higher in Honam province than other provinces. This data suggests that policymakers need to address these geographic differences to improve access to primary PCI for patients with STEMI.
Our data showed that conventional cardiovascular risk factors, such as old age (≥75 years), dyslipidemia, renal failure, and reduced left ventricular function, were more frequently observed in high-volume operators than low-/moderate-volume operators. Furthermore, multi-vessel disease was more frequently observed in high-volume operators than in low-/moderate-volume operators. However, patients who sustained cardiac arrest were more frequently treated by low-volume operators than by moderate-/high-volume operators. During the procedures, low-volume operators more frequently used IVUS and high-volume operators preferred trans-radial approach. These differences reflect real-life clinical practice in Korean interventional cardiology. Although several baseline characteristics were different among the 3 groups, in-hospital outcomes, including all-cause death, cardiac death, non-fatal MI, and stent thrombosis were similar in the 3 groups. However, the incidence of stroke was slightly higher in high-volume operators than low-/moderate-volume operators, which might be related to underlying patient risk factors. The multivariate analysis-adjusted conventional risk factors also showed that in-hospital outcomes were not associated with primary PCI operator volume. The recent study using data from the Japanese PCI registry, which included 19.3% STEMI PCI also showed no clear association between annual operator volume and clinical outcomes.
8) Another recent observational cohort study using the British Cardiovascular Intervention Society PCI database from 2013 to 2014 also showed no direct relationship between mortality and operator volume.
9) In the new generation DES era, clinical outcomes of STEMI patients are not dependent on the operator volume, because operator PCI skill has been much improved, and concrete evidence of the efficacy of primary PCI for STEMI patients is widely accepted. This finding required further study to evaluate this hypothesis.
In this study, most of the patient-oriented risk factors, such as age, diabetes, prior MI, renal failure, cardiogenic shock, cardiac arrest, and involvement of arteries such as the left main or proximal LAD, were identified as independent predictors for MACCEs. On the other hand, trans-radial approach and IVUS usage were associated with a reduced rate of MACCEs. Use of the radial artery for diagnostic and interventional coronary procedures was associated with significant reduction in access site complications compared to the femoral artery approach. The Radial versus Femoral Access for Coronary Angiography and Intervention in Patients with Acute Coronary Syndrome (RIVAL) trial demonstrated that the radial approach may be associated with significant reduction in access site complications and in mortality versus a femoral access approach especially in patients presenting with STEMI (HR, 0.60; 95% CI 0.38–0.94; p=0.026).
15) Our study also suggested that the radial access approach might be associated with a reduced rate of adverse in-hospital outcomes in primary PCI for STEMI patients. Another procedural factor related to reduced rate of adverse in-hospital outcomes is IVUS usage. Several recent randomized clinical trials which included patients with acute MI also demonstrated that IVUS-guided DES implantation significantly improved clinical outcomes.
16)17) It is possible that stent optimization after primary PCI is one of the most important factors that improves clinical outcomes in STEMI. Further studies should be undertaken to examine the role of IVUS in primary PCI. However, our data showed that IVUS is used in only 21.5% of primary PCI. This infrequent application of the IVUS method of access should be enhanced as a matter of policy in the treatment of STEMI.
Our study had several limitations that should be taken into account. First, our population included only those patients and hospitals that participated in the K-PCI registry, and it did not reflect all Korean PCI procedures. However, our data consisted of 92 PCI-capable hospitals which included the majority of high-volume centers, so it might represent the overall pattern of Korean primary PCI. Second, the present study was based on a non-randomized observational registry and it had intrinsic limitations related to nature of observations made. For this reason, the K-PCI registry did not have some important data related to the mortality of patients with STEMI, such as door-to-balloon time or exact symptom onset time. Some experienced operators may not be directly involved in primary PCI depending on individual hospitals. In addition, the number of PCI cases per year might be reduced in hospitals with many operators. For this reason, the PCI pattern might manifest a distorted picture due to differences between individual regions and hospitals. Our study results should be interpreted with caution, because high-volume operators were not equal to experienced operators. Furthermore, some definitions of clinical variables might be different depending on the particular centers, although strict definition of clinical terminology was stipulated before patient enrollment. However, on-site monitoring was conducted for the accuracy of data. Third, our data only reflected clinical outcomes during first hospitalization for PCI over 1 year and information on the long-term clinical outcome classified by operator volume was limited. It is necessary to perform a future study to evaluate the relationship between the operator volume and long-term clinical outcome.
In conclusion, our study is the first representative study to evaluate the relationship between operator volume and in-hospital clinical outcomes after primary PCI for patients with STEMI using K-PCI registry. Our data showed that in-hospital outcomes after primary PCI for STEMI were not associated with operator volume. Further research is required to evaluate long-term clinical outcomes in relation to operator volume after primary PCI for STEMI.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download