2. Cosselman KE, Navas-Acien A, Kaufman JD. Environmental factors in cardiovascular disease. Nat Rev Cardiol. 2015; 12:627–642. PMID:
26461967.

3. Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, et al. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ. 2015; 350:h1295. PMID:
25810496.

4. Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax. 2014; 69:660–665. PMID:
24706041.
5. Karakis I, Kordysh E, Lahav T, Bolotin A, Glazer Y, Vardi H, et al. Life prevalence of upper respiratory tract diseases and asthma among children residing in rural area near a regional industrial park: cross-sectional study. Rural Remote Health. 2009; 9:1092. PMID:
19645525.

6. Wu J, Ren C, Delfino RJ, Chung J, Wilhelm M, Ritz B. Association between local traffic-generated air pollution and preeclampsia and preterm delivery in the south coast air basin of California. Environ Health Perspect. 2009; 117:1773–1779. PMID:
20049131.

7. Takeda K, Tsukue N, Yoshida S. Endocrine-disrupting activity of chemicals in diesel exhaust and diesel exhaust particles. Environ Sci. 2004; 11:33–45. PMID:
15746887.
8. Wang J, Xie P, Kettrup A, Schramm KW. Inhibition of progesterone receptor activity in recombinant yeast by soot from fossil fuel combustion emissions and air particulate materials. Sci Total Environ. 2005; 349:120–128. PMID:
16198674.

9. Yauk C, Polyzos A, Rowan-Carroll A, Somers CM, Godschalk RW, Van Schooten FJ, et al. Germ-line mutations, DNA damage, and global hypermethylation in mice exposed to particulate air pollution in an urban/industrial location. Proc Natl Acad Sci U S A. 2008; 105:605–610. PMID:
18195365.

10. Gao H, Ma MQ, Zhou L, Jia RP, Chen XG, Hu ZD. Interaction of DNA with aromatic hydrocarbons fraction in atmospheric particulates of Xigu District of Lanzhou, China. J Environ Sci (China). 2007; 19:948–954. PMID:
17966851.

11. Maluf M, Perin PM, Foltran Januário DA, Nascimento Saldiva PH.
In vitro fertilization, embryo development, and cell lineage segregation after pre- and/or postnatal exposure of female mice to ambient fine particulate matter. Fertil Steril. 2009; 92:1725–1735. PMID:
18950758.
12. Perin PM, Maluf M, Czeresnia CE, Nicolosi Foltran Januário DA, Nascimento Saldiva PH. Effects of exposure to high levels of particulate air pollution during the follicular phase of the conception cycle on pregnancy outcome in couples undergoing
in vitro fertilization and embryo transfer. Fertil Steril. 2010; 93:301–303. PMID:
19631320.
13. Mohallem SV, de Araújo Lobo DJ, Pesquero CR, Assunção JV, de Andre PA, Saldiva PH, et al. Decreased fertility in mice exposed to environmental air pollution in the city of Sao Paulo. Environ Res. 2005; 98:196–202. PMID:
15820725.

14. Rocha E Silva IR, Lichtenfels AJ, Amador Pereira LA, Saldiva PH. Effects of ambient levels of air pollution generated by traffic on birth and placental weights in mice. Fertil Steril. 2008; 90:1921–1924. PMID:
18222432.

15. Missmer SA, Pearson KR, Ryan LM, Meeker JD, Cramer DW, Hauser R. Analysis of multiple-cycle data from couples undergoing
in vitro fertilization: methodologic issues and statistical approaches. Epidemiology. 2011; 22:497–504. PMID:
21558857.
16. Maity A, Williams PL, Ryan L, Missmer SA, Coull BA, Hauser R. Analysis of
in vitro fertilization data with multiple outcomes using discrete time-to-event analysis. Stat Med. 2014; 33:1738–1749. PMID:
24317880.
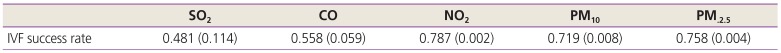
17. Choe SA, Jun YB, Lee WS, Yoon TK, Kim SY. Association between ambient air pollution and pregnancy rate in women who underwent IVF. Hum Reprod. 2018; 33:1071–1078. PMID:
29659826.

18. Han EJ, Kim SK, Lee JR, Jee BC, Suh CS, Kim SH. Multiple pregnancy after single or multiple embryo transfer performed according to Korean guidelines. Clin Exp Reprod Med. 2015; 42:169–174. PMID:
26816876.

19. de Boor C. A practical guide to splines. New York (NY): Springer-Verlag;1978.
20. Carré J, Gatimel N, Moreau J, Parinaud J, Leandri R. Influence of air quality on the results of
in vitro fertilization attempts: a retrospective study. Eur J Obstet Gynecol Reprod Biol. 2017; 210:116–122. PMID:
28012404.
21. Wood S, Quinn A, Troupe S, Kingsland C, Lewis-Jones I. Seasonal variation in assisted conception cycles and the influence of photoperiodism on outcome in
in vitro fertilization cycles. Hum Fertil (Camb). 2006; 9:223–229. PMID:
17190668.
22. Stolwijk AM, Reuvers MJ, Hamilton CJ, Jongbloet PH, Hollanders JM, Zielhuis GA. Seasonality in the results of
in-vitro fertilization. Hum Reprod. 1994; 9:2300–2305. PMID:
7714148.
23. Kirshenbaum M, Ben-David A, Zilberberg E, Elkan-Miller T, Haas J, Orvieto R. Influence of seasonal variation on
in vitro fertilization success. PLoS One. 2018; 13:e0199210. PMID:
29975717.
24. Tamura H, Nakamura Y, Korkmaz A, Manchester LC, Tan DX, Sugino N, et al. Melatonin and the ovary: physiological and pathophysiological implications. Fertil Steril. 2009; 92:328–343. PMID:
18804205.

25. Nobles CJ, Schisterman EF, Ha S, Buck Louis GM, Sherman S, Mendola P. Time-varying cycle average and daily variation in ambient air pollution and fecundability. Hum Reprod. 2018; 33:166–176. PMID:
29136143.

26. Legro RS, Sauer MV, Mottla GL, Richter KS, Li X, Dodson WC, et al. Effect of air quality on assisted human reproduction. Hum Reprod. 2010; 25:1317–1324. PMID:
20228391.

27. Mao L, Hu M, Pan B, Xie Y, Petersen EJ. Biodistribution and toxicity of radio-labeled few layer graphene in mice after intratracheal instillation. Part Fibre Toxicol. 2016; 13:7. PMID:
26864058.

28. Lee CH, Shim HE, Song L, Moon HG, Lee K, Yang JE, et al. Efficient and stable radiolabeling of polycyclic aromatic hydrocarbon assemblies:
in vivo imaging of diesel exhaust particulates in mice. Chem Commun (Camb). 2019; 55:447–450. PMID:
30474665.
29. Dejmek J, Jelínek R, Solansky' I, Benes I, Srám RJ. Fecundability and parental exposure to ambient sulfur dioxide. Environ Health Perspect. 2000; 108:647–654. PMID:
10903619.

30. Murphy KP. Machine learning: a probabilistic perspective. Cambridge (MA): MIT press;2012.
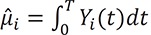 , and the error variance, determined by ˆ?2=∑Ni=1∫T0(Yi(t)-ˆµi)2dt/N
, and the error variance, determined by ˆ?2=∑Ni=1∫T0(Yi(t)-ˆµi)2dt/N . We then computed.
. We then computed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 .
. XML Download
XML Download