Abstract
Background
Several factors had been suggested to contribute to the development of hypertension in chronic glomerulonephritis (GN). This study was conducted to find the association of baseline blood pressure (BP) with pathophysiologic findings and later renal progression in chronic GN.
Methods
Clinico-pathological findings including serum creatinine (Cr), proteinuria, pathological findings, and urinary Na excretion were analyzed in a total of 233 patients with IgA nephropathy from The Kyung-Hee Cohort of GN. Glomerular surface area (GSA) was measured by imaging analysis and urine angiotensinogen (AGT) concentrations by human ELISA kits.
Results
Systolic BP was ≥130mmHg in 124 patients (53%). Systolic BP was negatively correlated with follow-up eGFR (r=−0.32, p<0.0001) and positively serum uric acid concentrations, while it had no significant relationships with initial serum Cr and eGFR. As compared with patients with systolic BP<130 mmHg, those with ≥130 mmHg were older and showed higher serum Cr, proteinuria, 24 hr urinary Na excretion, mean GSA, and T-I fibrosis, lower follow-up eGFR, and steeper decline in slope of eGFR. The results in patients with normal serum Cr concentrations were comparable to those in whole group. Systolic BP was positively correlated with age, baseline and follow-up proteinuria, serum uric acid concentrations and IgM deposit and negatively with follow-up eGFR. In subgroup analysis, systolic BP was also positively correlated with mean GSA and urinary AGT concentrations.
Hypertension is a frequent finding in patients with chronic kidney diseases. Renal parenchymal hypertension develops in the setting of acute glomerulonephritis (GN), chronic GN, diabetic nephropathy, polycystic kidney disease and hypertensive nephrosclerosis12). The high prevalence of hypertension in chronic GN including IgA nephropathy is related to the declining renal function1345). Almost all patients develop hypertension when the glomerular filtration rate (eGFR) declines. There may be main factors contributing to the development of hypertension in patients with chronic GN, which may be similar to those in essential hypertension, but more accentuated678). Sodium retention is of primary importance. Increased activity of renin-angiotensin-aldosterone system(RAAS) is responsible for the hypertension. Renal ischemia induced by microvascular damage is a potent stimulus of RAAS as well as of sympathetic nervous activity in renal disease. It has been suggested that hypertension in IgA nephropathy is primarily volume dependent, and that this increase in blood volume may not be related to the deterioration of renal function6). Even in the early stages of chronic GN, the pathological findings such as glomerular sclerosis, interstitial fibrosis/tubular atrophy, and arteriosclerosis can be observed and may be associated with sodium sensitivity8910). This comprehensive study was conducted to find the association of baseline blood pressure (BP) with many patho-physiologic findings and renal progression in the clinical settings of chronic GN.
We reviewed the data of The Glomerulonephritis (GN) Cohort at Kyung Hee University Medical Center and clinico-pathological findings were analyzed in a total of 233 patients with IgA nephropathy (IRB no.2018090601). The patients underwent renal biopsy from January 2001 to December 2006. This study was approved by the Ethics Committee of Kyung Hee University Medical Center.
Clinical parameters assessed at the time of renal biopsy included age, sex, BP, body mass index, urine protein creatinine ratio (PCR), hematuria, estimated GFR(eGFR), and serum creatinine (Cr), uric acid, triglyceride, and total cholesterol. We used the Modification of Diet in Renal Disease (MDRD) formula when calculating the eGFR11). The MDRD study equation is the most commonly used estimation equation and reasonably accurate in non-hospitalized patients known to have CKD. CKD-EPI is superior when GFR is normal or mildly reduced. By contrast, the MDRD study equation performs better at lower levels of GFR1213).
The primary outcome in this study was the follow-up eGFR at last visit and the rate of renal function decline that was expressed as the slope of eGFR(mL/min/1.73m2/month). Progressive or nonprogressive patients were defined as those who reached the rate of renal function decline or not.
The extent of hematuria was classified into 5 categories by red blood cell numbers observed under high-power field microscopy (0, 0–1; 1, 2–4; 2, 5–9; 3,10–29; 4, >30). The angiotensinogen (AGT) concentrations of urine were measured with human enzyme-linked immunosorbent assay (ELISA) kits (Immuno-Biological Laboratories Co., Ltd.) and adjusted by urinary Cr concentrations.
All kidney tissue specimens were obtained by percutaneous needle biopsy. The tissues were embedded in paraffin, cut into 3- to 4-µm sections, and then stained with hematoxylin and eosin, periodic acid-Schiff, Masson's trichrome, and periodic acid-methenamine. The histologic severity of glomerular lesions was graded by H. S. Lee's glomerular grading system14). According to this system, lesions were classified as follows: Grade I, normal or focal mesangial cell proliferation; Grade II, diffuse mesangial cell proliferation or <25% of glomeruli with crescent (Cr)/segmental sclerosis (SS)/global sclerosis (GS); Grade III, 25–49% of glomeruli with Cr/SS/GS; Grade IV, 50–74% of glomeruli with Cr/SS/GS; Grade V, ≥75% of glomeruli with Cr/SS/GS. Tubulointerstitial (T-I) fibrosis, T-I inflammation, and tubular atrophy ere also divided into Stages 0 through 4 depending on severity (0, none; 1, focal; 2, diffuse and mild; 3, diffuse and moderate; 4, diffuse and severe). The GSA was determined using imaging analysis software (BIOQUANT, TN, USA). The GSA was defined as the area described by the outer capillary loops of the tuft. The mean GSA was calculated by averaging the areas of all glomeruli without global sclerosis except for those with <40% of the maximum glomerular area within each specimen to avoid measuring a cross-section far from the maximal planar area. This is based on the fact that the planar cross-section of trichotomy of a sphere is equivalent to 40% of the maximal cross-sectional area. For each specimen, we also assessed the maximal GSA of maximally hypertrophied glomeruli identified in serial sections.
The results are expressed as the mean±SD and were statistically compared using an independent t-test or Man-Whitney test as required. We conducted Pearson and Spearman correlation analyses for parametric and nonparametric data, respectively. Categorical variables were compared using the χ2-test. Values of p<0.05 were considered to be statistically significant. All statistical analyses were performed using the SPSS program, version 15.0.
The mean duration of follow-up was 49.2±39.4 months. The mean serum Cr concentration in patients of this study was 1.18±0.75mg/dL and eGFR 89.2±69.7mL/min/1.73m2. Systolic BP was <130mmHg in 109 patients (47%) and ≥130mmHg in 124 patients (53%) and ≥ 140mmHg in 77 patients (33%). The mean spot urine PCR was 2.17±4.99 (Table 1). At last visit, the serum Cr concentration was 1.90±2.82mg/dL and eGFR 83.5±44.7mL/min/1.73m2.
When we examined the relationships of baseline BP with clinical data including renal function, systolic BP was negatively correlated with follow-up eGFR(r=−0.32, p<0.0001) (Fig. 1) and positively serum uric acid concentrations (r=0.49, p=0.0041), while it had no significant relationships with initial serum Cr concentrations and eGFR and the slope of change in eGFR.
As compared with patients (n=109) with systolic BP <130mmHg, those (n=124) with ≥130mmHg were older and showed higher levels of baseline and follow-up serum Cr and proteinuria, and 24 hr urinary Na excretion, lower follow-up eGFR, and steeper decline in slope of eGFR.
When we examined the relationships of baseline BP with pathological findings, systolic BP was positively C3 (r=0.18; p=0.015). Patients with systolic BP ≥130 mmHg as compared with those <130mmHg also showed higher level of T-I fibrosis (Table 2).
The urinary AGT concentrations and the mean GSA were examined in 36 among the total patients. Systolic BP was positively correlated with the mean GSA(r=0.35; p=0.041). The patients with systolic BP ≥130mmHg as compared with those <130mmHg showed higher level of mean GSA(Table 2). Systolic BP was positively correlated with the urinary AGT concentrations (r=0.37, p=0.03). The urinary AGT concentrations tended to be higher in patients with systolic BP ≥130mmHg, but without significance.
We examined the role of BP in 163 patients who had baseline normal serum Cr concentrations (Table 3). The results were comparable to those in the whole group of this study. Systolic BP was ≥130mmHg in 72 patients (44%) and ≥140mmHg in 42 (26%). Systolic BP was positively correlated with age, baseline and follow-up proteinuria, serum uric acid concentrations and IgM deposit and negatively with follow-up eGFR. Patients with systolic BP ≥130mmHg as compared with those <130mmHg showed worse follow-up clinical findings including higher serum Cr concentrations, larger amount of proteinuria, lower levels of eGFR and steeper decline in slope of eGFR, while there were no significant differences of T-I fibrosis and 24 hr urinary Na excretion.
Systolic BP was ≥130mmHg in 124 patients (53%) and ≥140mmHg in 77 (33%) in our study. Our results showed that systolic BP in the beginning may reflect clinico-pathological findings as well as later decline in renal function in patients with IgA nephropathy.
IgA nephropathy is characterized by the deposit of IgA in the glomerular mesangium. Many patients with IgA nephropathy show hematuria and/or proteinuria and develop chronic renal failure after long-term follow-up. Especially, hypertension is suggested to be one of main factors leading to the renal progression in IgA nephropathy345).
Our study showed that initial systolic BP was negatively correlated with follow-up eGFR, while it had no significant relationships with initial serum Cr concentrations and eGFR. As compared with patients systolic BP <130 mmHg, those with ≥130mmHg were older and showed severer clinical findings and poorer renal prognosis; higher levels of baseline and follow-up serum Cr and proteinuria, and the follow-up decline in renal function. Increased 24 hour urinary Na excretion observed in those with ≥130mmHg of this study may indicate the increased salt intake leading to high blood volume. It was earlier reported that the blood volume was high in patients with IgAN, and that mean arterial pressure was correlated with blood volume6).
Our study observed that systolic BP was positively correlated with pathological findings, including mean GSA and the degree of T-I fibrosis and deposits of IgM and C3. Patients with systolic BP ≥130 mmHg as compared with those <130mmHg showed more severe pathological findings of glomerulomegaly and T-I fibrosis. Systolic BP may cause the derangement of normal renal structure such as glomerular hypertrophy and T-I fibrosis observed in these patients. Also it was reported in patients with IgA nephropathy that the sodium sensitivity index was significantly correlated with glomerular sclerosis and T-I damage and the increased sodium sensitivity appeared before hypertension8). Resulting renal ischemia induced by microvascular damage is a potent stimulus of RAAS as well as of sympathetic nervous system in chronic GN7910). Eventually, almost all patients develop hypertension when the eGFR declines.
In subgroup patients with normal serum Cr concentrations, those with systolic BP ≥130mmHg as compared with <130mmHg also showed worse follow-up clinical findings of serum Cr concentration, amount of proteinuria and levels of eGFR. Baseline systolic BP was related to the later lower eGFR also in this subgroup. All results are the same as those in whole group patients except that 24hr urinary Na excretion, mean GSA, T-I fibrosis or urinary AGT concentrations tended to be higher, but not statistically significantly evident yet.
The pathophysiology in the development of hypertension can be understood in relation to several factors or stages in patients with chronic GN. According to experimental studies, systemic hypertension directly causes the glomerular hypertension by preglomerular autoregulatory impairment to the dynamic glomerular BP transmission through the afferent arterioles and/or by the absence of compensated efferent arteriolar vasodilation owing to activation of RAAS15). Glomerular hypertension may mediate progressive renal damage by leading to glomerular hyperfiltration and glomerular enlargement1617). Glomerular enlargement may reflect functional adaptation of glomeruli in patients with low glomerular density or a small number of functioning nephrons. Large glomeruli are a common finding in the early stage of renal disease and more susceptible to subsequent renal injury. Maximal glomerular diameter was proposed as a 10-year prognostic indicator for IgA nephropathy18). Our results showed that systolic BP was related to glomerulomegaly in patients with IgA nephropathy. Therefore, both factors may lead to the acceleration of loss of renal function. Glomerular capillary wall stretch due to glomerular hypertension or glomerular enlargement increases tensile stress on podocyte foot processes that cover the capillary resulting in podocyte injury, loss of glomerular barrier function leading to proteinuria, glomerulosclerosis and gradual loss of renal function19). This may in turn exacerbate the rise in systemic BP. Therefore, hypertension may be both a cause and a consequence of renal injury.
The Importance of intrarenal RAAS activation has been emphasized in the development of renal injury in renal diseases. We and others suggested that urinary AGT is speculated as a powerful tool for determining intrarenal RAAS status in patients with IgAN2021). This study showed that systolic BP was positively correlated with the urinary AGT concentrations, reflecting increased activity of intrarenal RAAS system in the process of chronic GN. This, however, is not evident in those with normal serum Cr concentrations, suggesting that intrarenal RAAS may be obviously activated as eGFR declines.
Our data also showed that systolic BP was positively correlated with serum uric acid concentrations, while the serum uric acid concentrations tended to be higher, but without significance in those with ≥130mmHg, as compared with patients systolic BP <130mmHg. Several studies have suggested the role of uric acid but whether it truly represents an independent risk factor for the development of cardiovascular diseases is still controversial. An animal study showed that hyperuricemia induces arteriolopathy of preglomerular vessels, which impairs the autoregulatory response of afferent arterioles, resulting in glomerular hypertension22). Lumen obliteration induced by vascular wall thickening produces severe renal hypoperfusion. The resulting ischemia is a potent stimulus that induces tubulointerstitial inflammation and fibrosis, as well as arterial hypertension. Serum uric acid concentrations increase in chronic kidney disease and may lead to tubular injury, endothelial dysfunction, oxidative stress, and intrarenal inflammation. Therefore, serum uric acid concentration is suggested to be an independent risk factor for kidney failure in earlier stages of chronic kidney disease and has a J-shaped relationship with all-cause mortality in chronic kidney disease23). Others suggested that hyperuricemia is independently associated with a decline in renal function and especially hypertension may mediate the association between serum uric acid and chronic kidney disease24).
It has been suggested that many factors may influence the renal progression of chronic GN. Although our study had several limitations, it helped the comprehensive understanding of relationships of baseline systolic BP with many clinico-pathological findings in the clinical settings of IgA nephropathy. This study showed that baseline systolic BP could be associated with proteinuria, urinary Na excretion, glomerulomegaly, T-I fibrosis and furthermore renal progression. If the baseline renal function were normal or decreased, as compared with patients with initial systolic BP <130mmHg, those with ≥130mmHg showed lower follow-up eGFR and steeper decline in slope of eGFR.
This is not a prospective well-controlled, but observational study. Our study could not explain the complex and diverse mechanisms operating in these processes. We could not examine the role of systolic BP during the follow-up and at final visit because of the use of anti-hypertensive medications.
Figures and Tables
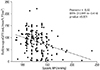 | Fig. 1Relationships between systolic BP and the follow-up eGFR. BP, blood pressure; CI, confidence interval; eGFR, estimated glomerular filtration rate. |
Table 2
Clinico-pathological findings according to systolic BP

*The extent of hematuria was converted into scores according to the number of red blood cells/high-power field as follows: none–1/0, 2–4/1, 5–9/2, 10–29/3, and ≥30/4.
†The histologic severity of glomerular lesions was graded by H. S. Lee's glomerular grading system
BP, blood pressure; eGFR, estimated glomerular filtration rate; F, female; GSA, glomerular surface area; M, male; yr, years Data expressed as mean±S.D. or %.
References
1. Orofino L, Quereda C, Lamas S, et al. Hypertension in primary chronic glomerulonephritis: analysis of 288 biopsied patients. Nephron. 1987; 45:22–26.

2. Glassock RJ AS, Ward HJ, Cohen AH. The kidney. 4 ed. 1991.
3. Berthoux F, Mohey H, Laurent B, Mariat C, Afiani A, Thibaudin L. Predicting the risk for dialysis or death in IgA nephropathy. J Am Soc Nephrol. 2011; 22:752–761.

4. Csiky B, Kovacs T, Wagner L, Vass T, Nagy J. Ambulatory blood pressure monitoring and progression in patients with IgA nephropathy. Nephrol Dial Transplant. 1999; 14:86–90.

5. Reich HN, Troyanov S, Scholey JW, Cattran DC, Toronto Glomerulonephritis R. Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol. 2007; 18:3177–3183.

6. Valvo E, Gammaro L, Bedogna V, et al. Hypertension in primary immunoglobulin A nephropathy (Berger’s disease): hemodynamic alterations and mechanisms. Nephron. 1987; 45:219–223.

7. Joles JA, Koomans HA. Causes and consequences of incresed sympathetic activity in renal disease. Hypertension. 2004; 43:699–706.

8. Konishi Y, Okada N, Okamura M, et al. Sodium sensitivity of blood pressure appearing before hypertension and related to histological damage in immunoglobulin a nephropathy. Hypertension. 2001; 38:81–85.

9. Bazzi C, Stivali G, Rachele G, Rizza V, Casellato D, Nangaku M. Arteriolar hyalinosis and arterial hypertension as possible surrogate markers of reduced interstitial blood flow and hypoxia in glomerulonephritis. Nephrology (Carlton). 2015; 20:11–11.

10. Abdi-Ali A, Mann MC, Hemmelgarn BR, et al. IgA nephropathy with early kidney disease is associated with increased arterial stiffness and renin-angiotensin system activity. J Renin Angiotensin Aldosterone Syst. 2015; 16:521–528.

11. Levey AS, Coresh J, Greene T, et al. Expressing the Modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007; 53:766–772.

12. Stevens LA, Schmid CH, Greene T, et al. Comparative performance of the CKD epidemiology collaboration (CKD-EPI) and the modification of diet in renal disease (MDRD) study equations for estimating GFR levels above 60mL/min/1.73m2. Am J Kidney Dis. 2010; 56:486–489.
13. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–612.

14. Lee HS, Lee MS, Lee SM, et al. Histological grading of IgA nephropathy predicting renal outcome: revisiting H. S. Lee’s glomerular grading system. Nephrol Dial Transplant. 2005; 20:342–348.

15. Kanetsuna Y, Hirano K, Nagata M, et al. Characterization of diabetic nephropathy in a transgenic model of hypoinsulinemic diabetes. Am J Physiol Renal Physiol. 2006; 291:F1315–F1322.

16. Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW. Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol. 2012; 8:293–300.

17. Neuringer JR, Brenner BM. Glomerular hypertension: cause and consequence of renal injury. J Hypertens Suppl. 1992; 10:S91–S97.
18. Kataoka H, Ohara M, Honda K, Mochizuki T, Nitta K. Maximal glomerular diameter as a 10-year prognostic indicator for IgA nephropathy. Nephrol Dial Transplant. 2011; 26:3937–3943.

19. Rennke HG, Klein PS. Pathogenesis and significance of nonprimary focal and segmental glomerulosclerosis. Am J Kidney Dis. 1989; 13:443–456.

20. Nishiyama A, Konishi Y, Ohashi N, et al. Urinary angiotensinogen reflects the activity of intrarenal renin-angiotensin system in patients with IgA nephropathy. Nephrol Dial Transplant. 2011; 26:170–177.

21. Kim YG, Song SB, Lee SH, et al. Urinary angiotensinogen as a predictive marker in patients with immunoglobulin A nephropathy. Clin Exp Nephrol. 2011; 15:720–726.

22. Sanchez-Lozada LG, Tapia E, Santamaria J, et al. Mild hyperuricemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int. 2005; 67:237–247.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download