Abstract
Gastric xanthoma is frequently an incidental finding on upper endoscopy in adults. Gastric xanthomas (GX) can be mistaken for malignancies and warrant prompt histologic diagnosis. The underlying etiology is not fully understood; however, it has been linked to Helicobacter pylori gastritis and gastric cancer. GX in the pediatric population is largely unreported in the literature. Because of the relative rarity, documentation with case reports are essential to provide as much data as possible to see if there is a correlation between GX and malignant potential in the pediatric population. Our group is reporting two cases, a 10-year-old male and a 7-year-old male, both who presented with chronic dysphagia, upper abdominal pain, nausea, vomiting, and loss of appetite. Upper endoscopies for both patients revealed small polypoid lesions located in the antrum with foamy histiocytes on histology, leading to the diagnosis of gastric xanthoma.
Go to : 
Gastric xanthomas (GX) are yellow-white nodules or polypoid lesions found in the gastric mucosa [1]. Although previously considered to be benign, newer studies suggest there may be progression to malignant pathology. Histologically, GX consist of a localized accumulation of lipids in foamy histiocytes in the lamina propria. Appearance is slightly variable and GX are typically less than 3 mm but have been described as large as 10 mm [12]. The etiology of GX is not clear, however, there is a close association between GX formation and Helicobacter pylori infections, atrophic gastritis, and malignancy [234]. The presence of GX is a positive indicator of H. pylori infection and may persist even after the completion of triple therapy [5]. GX cases have been reported in the adult population [3], but GX is rare in the pediatric population. Gastric xanthoma after H. pylori eradication was recently discovered to be a predictive marker for early gastric cancer in adults [4], but the potential malignancy risk in pediatric GX is currently unknown. We report a series of GX in two pediatric patients, one 7-years-of-age and the other 10-years-of-age, who presented with chronic vague upper abdominal pain, nausea, vomiting, dysphagia, and loss of appetite.
Go to : 
Patient 1 is a 10-year-old male presenting with complaints of nausea, vomiting, upper abdominal pain, loss of appetite, and progressive dysphagia for 2 months. The patient's family denies recent altered bowel patterns, hematemesis, or hematochezia. Previous attempts at treatment included a trial of Omeprazole 40 mg once daily, which failed to alleviate the symptoms. The patient has a medical history of prematurity born at 32 weeks gestation, anxiety disorder, attention deficit hyperactivity disorder, Tourette's Syndrome, and a seizure disorder. Surgical history is notable for an appendectomy. The patient's history was also notable for previous treatment of H. pylori gastritis at 6 years of age, which was diagnosed through endoscopy. The helicobacter eradication regimen previously used consisted of triple antibiotic therapy with omeprazole, amoxicillin, and clarithromycin twice daily for 14 days.
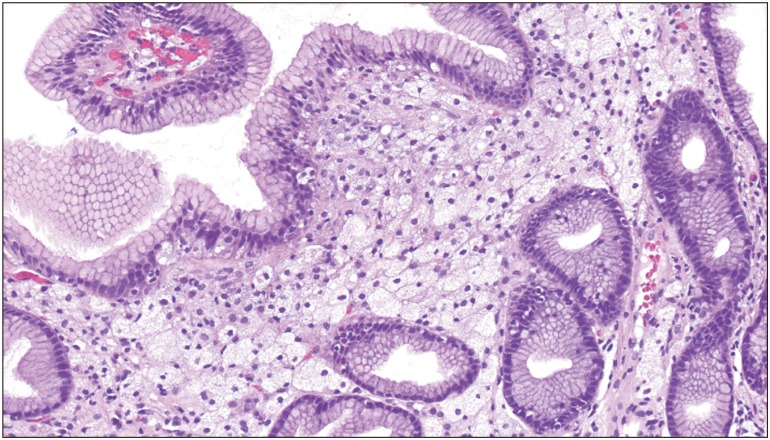
Current upper endoscopy showed mild gastritis, and a small, 3 mm pale yellow, plaque-like polypoid lesion located near the antrum of the stomach. Gastric biopsies revealed mild, chronic, non-specific gastritis and esophagitis. Lesion biopsies revealed chronic inflammatory infiltrate with lymphoplasmacytic predominance, leading to patchy areas of expansion within the lamina propria and subsequent destruction of isolated glands. Pathology confirmed lipid-laden histiocytes in the lamina propria, leading to the diagnosis of a gastric xanthoma. A rapid urease test for H. pylori was negative. The patient was lost to follow-up of biopsy results after endoscopy.
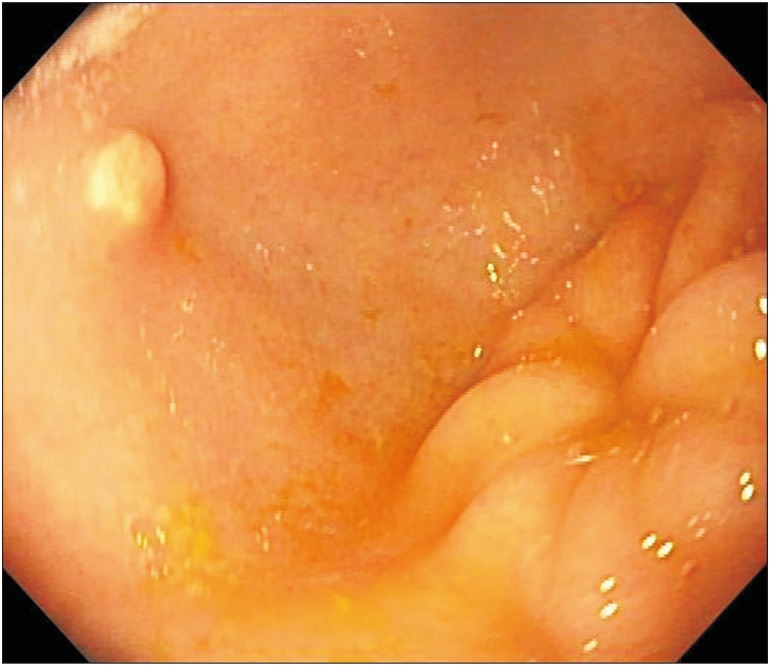
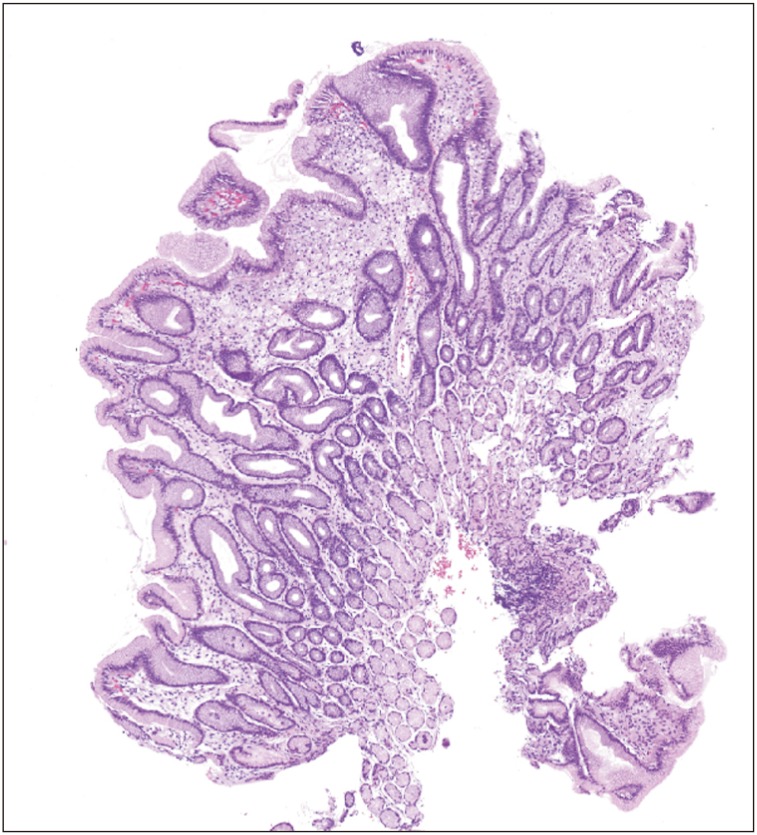
Patient 2 is a 7-year-old male who presented with a 3-month history of intermittent abdominal pain, vomiting, and loss of appetite. The patient has a medical history of constipation and a family history of a father with diverticulitis. Physical exam, along with labs, X-ray, and ultrasound ordered by the pediatrician were normal. Upper endoscopy revealed a small, plaque-like polypoid noted on the antrum (Fig. 1). Histology revealed the lipid-laden GX but no evidence of active H. pylori infection (Figs. 2 and 3). No serologic testing for H. pylori was performed.
No malignant histological changes were seen in either case.
Go to : 
The exact etiology of GX is not clinically clear, however, there is a close association between GX formation and H. pylori infections [234]. Formation has been speculated to occur during the healing process, with foamy transformation of the histiocytes caused by bacteria infiltration of the lamina propria [4]. Patient 1 was treated for H. pylori at 6-years of age and was found to have a GX four years later, but the patient was subsequently lost to follow-up.
Patient 2 did not have evidence of current H. pylori infection, but past H. pylori infection could not be excluded. Patient 2 is scheduled for routine endoscopic follow-up.
Multifocal atrophic gastritis, hypercholesterolemia, cholestasis, and malignancy have also been suspected to play a role in the formation of GX [34]. In addition, the presence of GX was reported to be significantly associated with gastric cancer in adults as an independent factor [34]. Another study reported the presence of GX post H. pylori infection should be considered a predictive marker for metachronous and synchronous gastric cancer, when matched with atrophy [3]. This same study also concluded that male sex, atrophy, presence of intestinal metaplasia, and GX were all independent predictive markers for early gastric cancer after H. pylori infection and eradication [3].
GX in the pediatric population are extremely rare and traditionally thought to be benign. This may result in underreporting of gastric xanthoma in literature [5678]. GX are typically asymptomatic and discovered as an incidental finding during an upper endoscopic procedure. GX are much more common in adults than in children, leading to the original thought that they were the sign of aging gastric mucosa, lipid dysregulation, and potential malignancy [1]. The long-term effects of GX in children are unknown. The presence of GX after H. pylori infection in pediatric patients need improved reporting with further study of long-term patient outcomes to determine whether GX may be linked to malignant pathology in children.
In conclusion, here we report a series of two cases of children with GX. GX are rare lesions in the pediatric population. GX are isolated and well-demarcated polyps that consist of lipid-laden histiocytes. Typically thought of as a benign lesion in an aging population, newer studies suggest that GX are linked to a more serious underlying pathology in adults. Some authors suggest GX diagnosed post H. pylori eradication should be treated as an independent predictive marker for gastric cancer in adults [3]. More studies are needed to determine the malignant potential of GX diagnosed during childhood. Due to the rarity and under-reporting of GX in the pediatric population, a longitudinal multi-center approach is recommended for further study.
Go to : 
References
1. Basyigit S, Kefeli A, Asilturk Z, Sapmaz F, Aktas B. Gastric xanthoma: a review of the literature. Shiraz E Med J. 2015; 16.

2. Alzahrani M, Alqunaitir A, Alsohaibani M, Al-Rikabi AC. Gastric xanthelasma associated with hyperplastic polyp and mucosal erosions: report of an unusual case and literature review. Oxf Med Case Reports. 2018; 2018:omy051. PMID: 30151218.

3. Shibukawa N, Ouchi S, Wakamatsu S, Wakahara Y, Kaneko A. Gastric xanthoma is a predictive marker for metachronous and synchronous gastric cancer. World J Gastrointest Oncol. 2017; 9:327–332. PMID: 28868113.

4. Shibukawa N, Ouchi S, Wakamatsu S, Wakahara Y, Kaneko A. Gastric xanthoma is a predictive marker for early gastric cancer detected after helicobacter pylori eradication. Intern Med. 2019; 58:779–784. PMID: 30449773.
5. Gasparetto M, Mara C, Graziella G, Gianmaria P, Francesca G. A rare case of pediatric gastric xanthoma: diagnosis and follow-up. J Gastroenterol Hepatol Res. 2013; 2:607–608.
6. Halabi I, Yaseen M, Vesoulis Z, Nostrant TT. Multiple gastric xanthomas in a 3-year-old patient. Gastroenterol Hepatol. 2010; 6:181–184.
7. Collins MH, Olazagasti JC, Fitzgerald J. Gastric xanthomas in a child. J Pediatr Gastroenterol Nutr. 1994; 19:444–447. PMID: 7877001.

8. Wetzler G, Felix AA, Lipton JF. Gastric xanthelasma. J Pediatr Gastroenterol Nutr. 2010; 51:1. PMID: 20543717.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download