1. Youssef NN, Di Lorenzo C. Childhood constipation: evaluation and treatment. J Clin Gastroenterol. 2001; 33:199–205. PMID:
11500607.
2. Southwell BR, King SK, Hutson JM. Chronic constipation in children: organic disorders are a major cause. J Paediatr Child Health. 2005; 41:1–15. PMID:
15670216.

3. Poenaru D, Roblin N, Bird M, Duce S, Groll A, Pietak D, et al. The pediatric Bowel Management Clinic: initial results of a multidisciplinary approach to functional constipation in children. J Pediatr Surg. 1997; 32:843–848. PMID:
9200083.

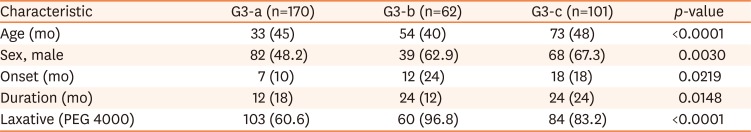
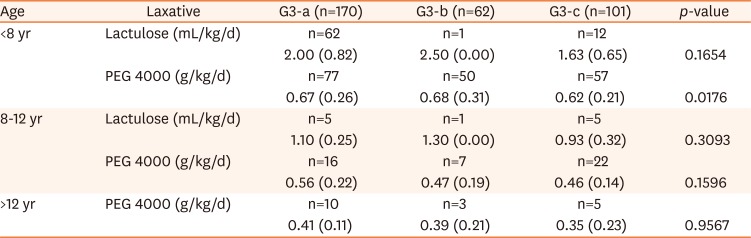
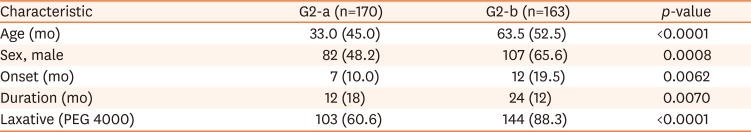
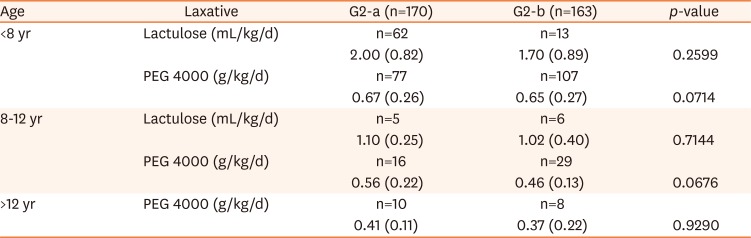
4. Chanpong A, Osatakul S. Laxative choice and treatment outcomes in childhood constipation: clinical data in a longitudinal retrospective study. Pediatr Gastroenterol Hepatol Nutr. 2018; 21:101–110. PMID:
29713607.

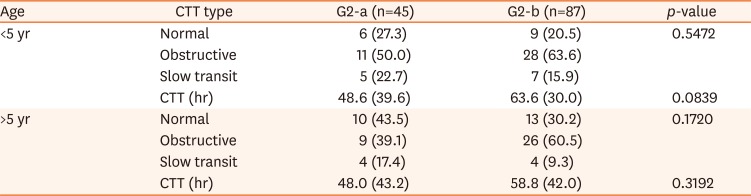
5. Bae SH, Kim MR. Subtype classification of chronic functional childhood constipation with a colon transit time test: therapeutic perspective. Paper presented at: 5th World Congress of Pediatric Gastroenterology, Hepatology and Nutrition. 2016 Oct 5–8; Montreal, Canada. 252.
6. Treepongkaruna S, Simakachorn N, Pienvichit P, Varavithya W, Tongpenyai Y, Garnier P, et al. A randomised, double-blind study of polyethylene glycol 4000 and lactulose in the treatment of constipation in children. BMC Pediatr. 2014; 14:153. PMID:
24943105.

7. Kim MR, Park HW, Son JS, Lee R, Bae SH. Correlation between colon transit time test value and initial maintenance dose of laxative in children with chronic functional constipation. Pediatr Gastroenterol Hepatol Nutr. 2016; 19:186–192. PMID:
27738600.

8. Metcalf AM, Phillips SF, Zinsmeister AR, MacCarty RL, Beart RW, Wolff BG. Simplified assessment of segmental colonic transit. Gastroenterology. 1987; 92:40–47. PMID:
3023168.

9. Clayden GS, Keshtgar AS, Carcani-Rathwell I, Abhyankar A. The management of chronic constipation and related faecal incontinence in childhood. Arch Dis Child Educ Pract. 2005; 90:ep58–67.

10. Biggs WS, Dery WH. Evaluation and treatment of constipation in infants and children. Am Fam Physician. 2006; 73:469–477. PMID:
16477894.
11. Felt B, Wise CG, Olson A, Kochhar P, Marcus S, Coran A. Guideline for the management of pediatric idiopathic constipation and soiling. Multidisciplinary team from the University of Michigan Medical Center in Ann Arbor. Arch Pediatr Adolesc Med. 1999; 153:380–385. PMID:
10201721.

12. Voderholzer WA, Schatke W, Mühldorfer BE, Klauser AG, Birkner B, Müller-Lissner SA. Clinical response to dietary fiber treatment of chronic constipation. Am J Gastroenterol. 1997; 92:95–98. PMID:
8995945.
13. Rao SS. Constipation: evaluation and treatment of colonic and anorectal motility disorders. Gastroenterol Clin North Am. 2007; 36:687–711. PMID:
17950444.

14. Knowles CH, Scott SM, Wellmer A, Misra VP, Pilot MA, Williams NS, et al. Sensory and autonomic neuropathy in patients with idiopathic slow-transit constipation. Br J Surg. 1999; 86:54–60. PMID:
10027360.

15. Knowles CH, Martin JE. Slow transit constipation: a model of human gut dysmotility. Review of possible aetiologies. Neurogastroenterol Motil. 2000; 12:181–196. PMID:
10877606.

16. Tzavella K, Riepl RL, Klauser AG, Voderholzer WA, Schindlbeck NE, Müller-Lissner SA. Decreased substance P levels in rectal biopsies from patients with slow transit constipation. Eur J Gastroenterol Hepatol. 1996; 8:1207–1211. PMID:
8980942.

17. Cortesini C, Cianchi F, Infantino A, Lise M. Nitric oxide synthase and VIP distribution in enteric nervous system in idiopathic chronic constipation. Dig Dis Sci. 1995; 40:2450–2455. PMID:
7587830.

18. Rao SSC, Parkman HP, McCallum RW. Handbook of gastrointestinal motility and functional disorders. Thorofare: SLACK Incorporated;2015.
19. Saad MRJ. Slow transit constipation. In : Rao SSC, Parkman HP, McCallum RW, editors. Handbook of gastrointestinal motility and functional disorders. Thorofare: SLACK Incorporated;2015. p. 241–252.
20. Attaluri A, Jackson M, Valestin J, Rao SS. Methanogenic flora is associated with altered colonic transit but not stool characteristics in constipation without IBS. Am J Gastroenterol. 2010; 105:1407–1411. PMID:
19953090.

21. Kim K, Jeon HJ, Bae SH. Value of fluoroscopic defecography in constipated children with abnormal colon transit time test results. J Neurogastroenterol Motil. 2019; DOI:
10.5056/jnm18201. [Epub ahead of print].

22. Lee G, Jeon HJ, Bae SH. Pelvic floor dysfunction in chronic constipated children. Paper presented at: The 68th Fall Conference, The Korean Pediatric Society. 2018 Oct 18; Seoul, Korea.
23. Nelson RL. Epidemiology of fecal incontinence. Gastroenterology. 2004; 126(1 Suppl 1):S3–S7. PMID:
14978632.

24. Lembo AJ. Constipation. In : Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger and Fordtran's gastrointestinal and liver disease. 10th ed. Amsterdam: Elsevier Inc.;2016. p. 270–296.
25. Rajindrajith S, Devanarayana NM, Benninga MA. Review article: faecal incontinence in children: epidemiology, pathophysiology, clinical evaluation and management. Aliment Pharmacol Ther. 2013; 37:37–48. PMID:
23106105.

26. Griffiths DM. The physiology of continence: idiopathic fecal constipation and soiling. Semin Pediatr Surg. 2002; 11:67–74. PMID:
11973758.

27. Whitehead WE, Chiarioni G. Fecal incontinence. In : Rao SSC, Parkman HP, McCallum RW, editors. Handbook of gastrointestinal motility and functional disorders. Thorofare: SLACK Incorporated;2015. p. 265–278.
28. Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM. Nelson textbook of pediatrics. 21th ed. Philadelphia: Elsevier;2019. p. 2045.
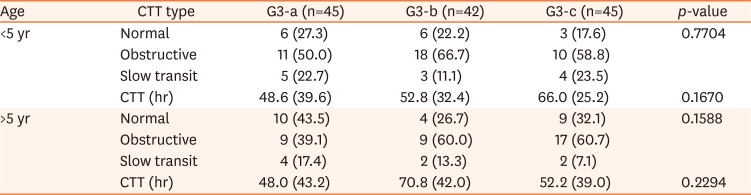
29. Yoo HY, Kim MR, Park HW, Son JS, Bae SH. Colon transit time test in Korean children with chronic functional constipation. Pediatr Gastroenterol Hepatol Nutr. 2016; 19:38–43. PMID:
27064388.

30. Benninga MA, Büller HA, Tytgat GN, Akkermans LM, Bossuyt PM, Taminiau JA. Colonic transit time in constipated children: does pediatric slow-transit constipation exist? J Pediatr Gastroenterol Nutr. 1996; 23:241–251. PMID:
8890073.

31. Wagener S, Shankar KR, Turnock RR, Lamont GL, Baillie CT. Colonic transit time--what is normal? J Pediatr Surg. 2004; 39:166–169. discussion 166-9. PMID:
14966733.

32. Lee-Robichaud H, Thomas K, Morgan J, Nelson RL. Lactulose versus Polyethylene Glycol for chronic constipation. Cochrane Database Syst Rev. 2010; (7):CD007570. PMID:
20614462.

33. Dupont C, Leluyer B, Maamri N, Morali A, Joye JP, Fiorini JM, et al. Double-blind randomized evaluation of clinical and biological tolerance of polyethylene glycol 4000 versus lactulose in constipated children. J Pediatr Gastroenterol Nutr. 2005; 41:625–633. PMID:
16254521.

34. Voskuijl W, de Lorijn F, Verwijs W, Hogeman P, Heijmans J, Mäkel W, et al. PEG 3350 (Transipeg) versus lactulose in the treatment of childhood functional constipation: a double blind, randomised, controlled, multicentre trial. Gut. 2004; 53:1590–1594. PMID:
15479678.

35. Lee SH, Bae SH. Maintenance dose of electrolyte free polyethylene glycol (PEG) 4000 in Korean children with chronic functional constipation. Korean J Pediatr. 2007; 50:1212–1216.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download