1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014; 311:806–814. PMID:
24570244.

2. Shan XY, Xi B, Cheng H, Hou DQ, Wang Y, Mi J. Prevalence and behavioral risk factors of overweight and obesity among children aged 2-18 in Beijing, China. Int J Pediatr Obes. 2010; 5:383–389. PMID:
20233154.

3. Kang KS. Nutritional counseling for obese children with obesity-related metabolic abnormalities in Korea. Pediatr Gastroenterol Hepatol Nutr. 2017; 20:71–78. PMID:
28730130.

4. Sharma V, Coleman S, Nixon J, Sharples L, Hamilton-Shield J, Rutter H, et al. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev. 2019; 20:1341–1349. PMID:
31342672.
5. Sagar R, Gupta T. Psychological aspects of obesity in children and adolescents. Indian J Pediatr. 2018; 85:554–559. PMID:
29150753.

6. Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003; 111(4 Pt 1):851–859. PMID:
12671123.

7. Sawyer MG, Harchak T, Wake M, Lynch J. Four-year prospective study of BMI and mental health problems in young children. Pediatrics. 2011; 128:677–684. PMID:
21930536.

8. Yi DY, Kim SC, Lee JH, Lee EH, Kim JY, Kim YJ, et al. Clinical practice guideline for the diagnosis and treatment of pediatric obesity: recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition. Korean J Pediatr. 2019; 62:3–21. PMID:
30589999.

9. Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010; 67:220–229. PMID:
20194822.
10. Abou Abbas L, Salameh P, Nasser W, Nasser Z, Godin I. Obesity and symptoms of depression among adults in selected countries of the Middle East: a systematic review and meta-analysis. Clin Obes. 2015; 5:2–11. PMID:
25504829.

11. Roberts RE, Duong HT. Obese youths are not more likely to become depressed, but depressed youths are more likely to become obese. Psychol Med. 2013; 43:2143–2151. PMID:
23298458.

12. Burke NL, Storch EA. A meta-analysis of weight status and anxiety in children and adolescents. J Dev Behav Pediatr. 2015; 36:133–145. PMID:
25706514.

13. Roohafza H, Kelishadi R, Sadeghi M, Hashemipour M, Pourmoghaddas A, Khani A. Are obese adolescents more depressed? J Educ Health Promot. 2014; 3:74. PMID:
25077167.
14. Whitaker BN, Fisher PL, Jambhekar S, Com G, Razzaq S, Thompson JE, et al. Impact of degree of obesity on sleep, quality of life, and depression in youth. J Pediatr Health Care. 2018; 32:e37–44. PMID:
29455855.

15. Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel AW. Are obese adolescents and young adults at higher risk for mental disorders? A community survey. Obes Res. 2002; 10:1152–1160. PMID:
12429879.

16. Mannan M, Mamun A, Doi S, Clavarino A. Prospective associations between depression and obesity for adolescent males and females- a systematic review and meta-analysis of longitudinal studies. PLoS One. 2016; 11:e0157240. PMID:
27285386.

17. Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev. 2017; 18:742–754. PMID:
28401646.

18. Esposito M, Gallai B, Roccella M, Marotta R, Lavano F, Lavano SM, et al. Anxiety and depression levels in prepubertal obese children: a case-control study. Neuropsychiatr Dis Treat. 2014; 10:1897–1902. PMID:
25336955.
19. Sheinbein DH, Stein RI, Hayes JF, Brown ML, Balantekin KN, Conlon RPK, et al. Factors associated with depression and anxiety symptoms among children seeking treatment for obesity: a social-ecological approach. Pediatr Obes. 2019; 14:e12518. PMID:
30990254.

20. Wang S, Sun Q, Zhai L, Bai Y, Wei W, Jia L. The prevalence of depression and anxiety symptoms among overweight/obese and non-overweight/non-obese children/adolescents in China: a systematic review and meta-analysis. Int J Environ Res Public Health. 2019; 16:E340. PMID:
30691096.

21. Reeves GM, Postolache TT, Snitker S. Childhood obesity and depression: connection between these growing problems in growing children. Int J Child Health Hum Dev. 2008; 1:103–114. PMID:
18941545.
22. Anderson SE, Cohen P, Naumova EN, Jacques PF, Must A. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. 2007; 69:740–747. PMID:
17942847.

23. Sanderson K, Patton GC, McKercher C, Dwyer T, Venn AJ. Overweight and obesity in childhood and risk of mental disorder: a 20-year cohort study. Aust N Z J Psychiatry. 2011; 45:384–392. PMID:
21500955.

24. Rancourt D, McCullough MB. Overlap in eating disorders and obesity in adolescence. Curr Diab Rep. 2015; 15:78. PMID:
26303593.

25. Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012; 14:406–414. PMID:
22644309.

26. Veses AM, Martínez-Gómez D, Gómez-Martínez S, Vicente-Rodriguez G, Castillo R, Ortega FB, et al. AVENA. AFINOS Study Groups. Physical fitness, overweight and the risk of eating disorders in adolescents. The AVENA and AFINOS studies. Pediatr Obes. 2014; 9:1–9. PMID:
24449515.

27. Pasold TL, McCracken A, Ward-Begnoche WL. Binge eating in obese adolescents: emotional and behavioral characteristics and impact on health-related quality of life. Clin Child Psychol Psychiatry. 2014; 19:299–312. PMID:
23749140.

28. Carriere C, Michel G, Féart C, Pellay H, Onorato O, Barat P, et al. Relationships between emotional disorders, personality dimensions, and binge eating disorder in French obese adolescents. Arch Pediatr. 2019; 26:138–144. PMID:
30898314.

29. Decaluwé V, Braet C, Fairburn CG. Binge eating in obese children and adolescents. Int J Eat Disord. 2003; 33:78–84. PMID:
12474202.

30. Brechan I, Kvalem IL. Relationship between body dissatisfaction and disordered eating: mediating role of self-esteem and depression. Eat Behav. 2015; 17:49–58. PMID:
25574864.

31. Byrne ME, LeMay-Russell S, Tanofsky-Kraff M. Loss-of-control eating and obesity among children and adolescents. Curr Obes Rep. 2019; 8:33–42. PMID:
30701372.

32. Barlow SE. Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007; 120(Suppl 4):S164–S192. PMID:
18055651.

33. Sönmez AÖ, Yavuz BG, Aka S, Semiz S. Attention-deficit hyperactivity disorder symptoms and conduct problems in children and adolescents with obesity. The Medical Bulletin of SISLI ETFAL Hospital. 2019; 53:300–305.
34. Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2016; 173:34–43. PMID:
26315982.

35. Erhart M, Herpertz-Dahlmann B, Wille N, Sawitzky-Rose B, Hölling H, Ravens-Sieberer U. Examining the relationship between attention-deficit/hyperactivity disorder and overweight in children and adolescents. Eur Child Adolesc Psychiatry. 2012; 21:39–49. PMID:
22120761.

36. Leib S, Gilon Mann T, Stein D, Vusiker I, Tokatly Latzer I, Ben-Ami M, et al. High prevalence of attention-deficit/hyperactivity disorder in adolescents with severe obesity seeking bariatric surgery. Acta Paediatr. 2019; [Epub ahead of print]. DOI:
10.1111/apa.15039.

37. Martins-Silva T, Vaz JDS, Hutz MH, Salatino-Oliveira A, Genro JP, Hartwig FP, et al. Assessing causality in the association between attention-deficit/hyperactivity disorder and obesity: a Mendelian randomization study. Int J Obes (Lond). 2019; 43:2500–2508. PMID:
31000774.

38. Kalarchian MA, Marcus MD. Psychiatric comorbidity of childhood obesity. Int Rev Psychiatry. 2012; 24:241–246. PMID:
22724645.

39. Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013; 13:6–13. PMID:
23200634.

40. Rupp K, McCoy SM. Bullying perpetration and victimization among adolescents with overweight and obesity in a nationally representative sample. Child Obes. 2019; 15:323–330. PMID:
31062988.

41. Koyanagi A, Veronese N, Vancampfort D, Stickley A, Jackson SE, Oh H, et al. Association of bullying victimization with overweight and obesity among adolescents from 41 low- and middle-income countries. Pediatr Obes. 2020; 15:e12571. PMID:
31389204.

42. Pont SJ, Puhl R, Cook SR, Slusser W. Section on Obesity; Obesity Society. Stigma experienced by children and adolescents with obesity. Pediatrics. 2017; 140:e20173034. PMID:
29158228.
43. Amaya-Hernández A, Ortega-Luyando M, Bautista-Díaz ML, Alvarez-Rayón GL, Mancilla-Díaz JM. Children with obesity: peer influence as a predictor of body dissatisfaction. Eat Weight Disord. 2019; 24:121–127. PMID:
28271455.

44. Gouveia MJ, Frontini R, Canavarro MC, Moreira H. Quality of life and psychological functioning in pediatric obesity: the role of body image dissatisfaction between girls and boys of different ages. Qual Life Res. 2014; 23:2629–2638. PMID:
24817248.

45. Phan TT, Chen FF, Pinto AT, Cox C, Robbins J, Kazak AE. Impact of psychosocial risk on outcomes among families seeking treatment for obesity. J Pediatr. 2018; 198:110–116. PMID:
29628410.

46. World Health Organization. Report of the commission on ending childhood obesity. Geneva: World Health Organization;2016.
47. Peirson L, Fitzpatrick-Lewis D, Morrison K, Warren R, Usman Ali M, Raina P. Treatment of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ Open. 2015; 3:E35–46.

48. Kamath CC, Vickers KS, Ehrlich A, McGovern L, Johnson J, Singhal V, et al. Clinical review: behavioral interventions to prevent childhood obesity: a systematic review and metaanalyses of randomized trials. J Clin Endocrinol Metab. 2008; 93:4606–4615. PMID:
18782880.
49. Shaw K, O'Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005; (2):CD003818. PMID:
15846683.

50. Chu DT, Minh Nguyet NT, Nga VT, Thai Lien NV, Vo DD, Lien N, et al. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab Syndr. 2019; 13:155–160. PMID:
30641689.

51. Brennan L, Walkley J, Fraser SF, Greenway K, Wilks R. Motivational interviewing and cognitive behaviour therapy in the treatment of adolescent overweight and obesity: study design and methodology. Contemp Clin Trials. 2008; 29:359–375. PMID:
17950046.

52. Brennan L, Walkley J, Wilks R, Fraser SF, Greenway K. Physiological and behavioural outcomes of a randomised controlled trial of a cognitive behavioural lifestyle intervention for overweight and obese adolescents. Obes Res Clin Pract. 2013; 7:e23–41. PMID:
24331680.

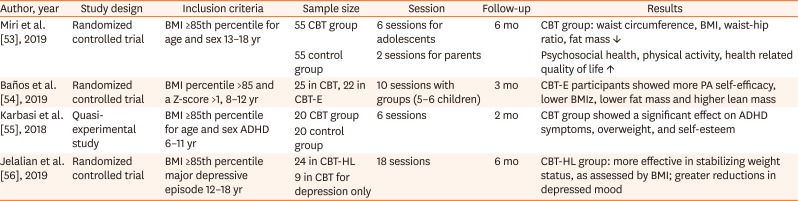
53. Miri SF, Javadi M, Lin CY, Griffiths MD, Björk M, Pakpour AH. Effectiveness of cognitive-behavioral therapy on nutrition improvement and weight of overweight and obese adolescents: a randomized controlled trial. Diabetes Metab Syndr. 2019; 13:2190–2197. PMID:
31235156.
54. Baños RM, Oliver E, Navarro J, Vara MD, Cebolla A, Lurbe E, et al. Efficacy of a cognitive and behavioral treatment for childhood obesity supported by the ETIOBE web platform. Psychol Health Med. 2019; 24:703–713. PMID:
30648879.

55. Karbasi Amel A, Karbasi Amel S, Erfan A. Effectiveness of parents-focused cognitive-behavioral therapy on attention deficit hyperactivity disorder symptoms, obesity and self-esteem of overweight children with attention deficient hyperactivity disorder. Adv Biomed Res. 2018; 7:73. PMID:
29862222.

56. Jelalian E, Jandasek B, Wolff JC, Seaboyer LM, Jones RN, Spirito A. Cognitive-behavioral therapy plus healthy lifestyle enhancement for depressed, overweight/obese adolescents: results of a pilot trial. J Clin Child Adolesc Psychol. 2019; 48(sup1):S24–S33. PMID:
27310418.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download