This article has been
cited by other articles in ScienceCentral.
Abstract
Klippel-Trenaunay syndrome (KTS) is a rare disorder characterized by a triad of abnormal bone and soft tissue growth, the presence of a port-wine stain, and venous malformations. Gastrointestinal (GI) manifestations of KTS are relatively common and generally do not cause significant problems. However, persistence can lead to chronic GI blood loss or even massive bleeding in rare cases. The majority of the severe GI manifestations associated with KTS present as vascular malformations around the GI tract and exposed vessels can lead to serious bleeding into the GI tract. Herein, we report a case of a 16-year-old boy with severe iron deficiency anemia who was previously misdiagnosed as hemorrhoid due to small amount of chronic bleeding. The actual cause of chronic GI bleeding was from an uncommon GI manifestation of KTS as rectal polyposis.
Keywords: Gastrointestinal hemorrhage, Polyps, Vascular malformations
INTRODUCTION
Klippel-Trenaunay syndrome (KTS) is a rare disorder characterized by a triad of abnormal bone and soft tissue, the presence of a port-wine stain, and venous malformations [
1]. The symptoms of KTS vary depending on the location of involved organs and the degree of involvement. KTS is one of the most important differential diagnosis for hemihypertrophy in children and can be readily diagnosed in patients that present with the characteristic pattern of abnormal bone and soft tissue growth at birth. The presence of a significant port-wine stain also raises suspicion for KTS and other capillary malformations and can lead to a prompt diagnosis. However, the diagnosis of KTS becomes difficult when these two features are not immediately apparent to the naked eye and when the patient presents with unusual organ involvement, such as the gastrointestinal (GI) tract.
GI involvement in KTS is often asymptomatic but can sometimes lead to significant complications such as chronic GI blood loss and massive GI bleeding [
12]. In this study, we present the case of a male pediatric patient with KTS who presented with severe iron deficiency anemia (IDA) secondary to chronic intestinal blood loss and other unusual GI manifestations.
CASE REPORT
A 16-year-old boy was referred for endoscopy due to severe IDA and recurrent hematochezia. He was noted to have mild intellectual disability at the level of elementary school but denied diarrhea, constipation, weight loss, or growth restriction. He initially denied hematochezia but later explained that he defecated feces stained with fresh blood 2 to 3 times a month for several years. His mother recalled that the patient had hematochezia at age 6 which led him to be misdiagnosed with hemorrhoids. The patient did not receive regular health care but visited the clinic for cellulitis treatment upon the diagnosis of IDA.
The patient had a height of 177.5 cm and a weight of 76.1 kg. His vital signs were stable and abdominal examinations were unremarkable. Vascular engorgement was observed around the anus but no fissures were seen. A blood test showed a white blood cell count of 4,590/mm3, a hemoglobin level of 5.9 g/dL, a hematocrit of 23.2%, and a platelet count of 305,000/mm3. Mean corpuscular volume was determined to be 64.4 fL while ferritin level was at 3 ng/mL; these findings were suggestive of IDA. All other laboratory parameters were unremarkable.
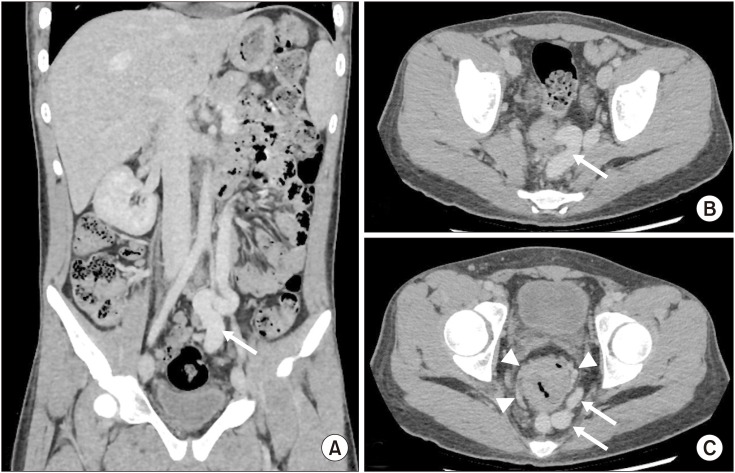
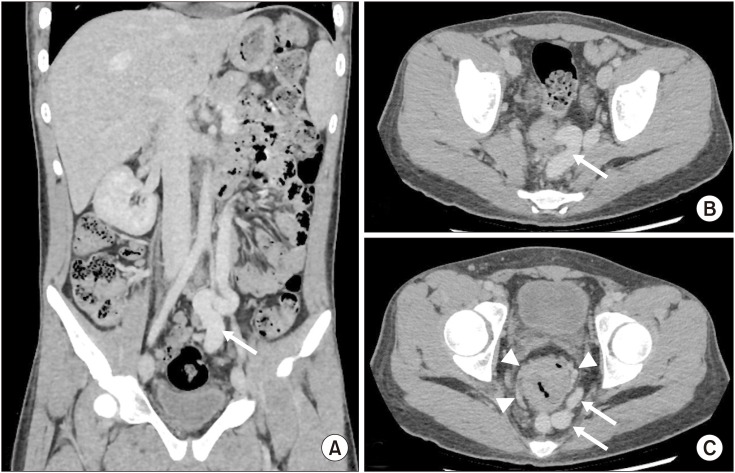
Abdominal computed tomography (CT) showed a huge, dilated aberrant vein that drained both the splenic and left internal iliac veins (
Fig. 1). This vein had developed most tortuously around the rectum. Congested small vessels around the rectum merged into the superior and middle rectal veins and drained into the left internal iliac vein. Additionally, the rectal mucosa showed prominent enhancement with associated thickening of the rectal walls. There was no evidence of arteriovenous malformations or fistulas. Doppler ultrasound of the liver demonstrated intact portal venous flow.
Fig. 1
Colonoscopy showing multiple numerous sessile and pedunculated (arrow) polyps (A, B) covered with diffuse fibrinous exudative materials in the rectum. Nearly the entire encircled luminal mucosa was affected. (C, D) Tortuous and dilated surface blood vessels are noted on the tip of the polyps.
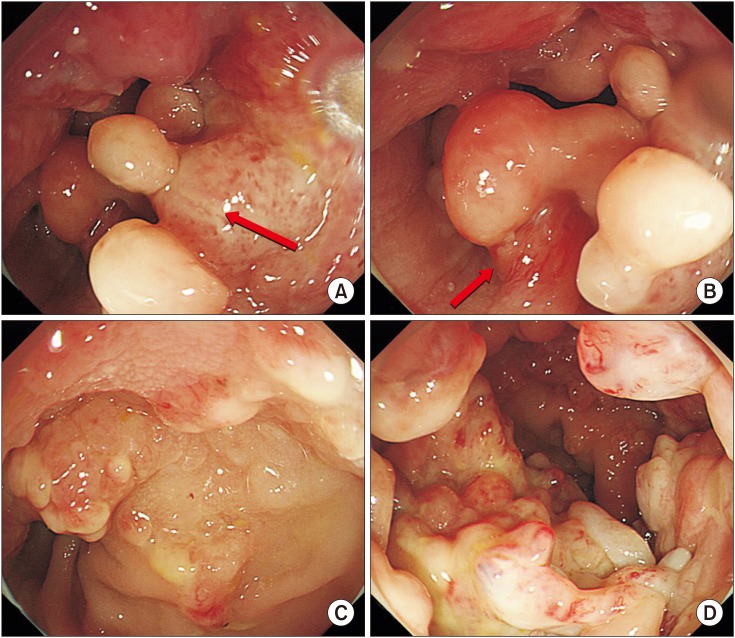
Colonoscopy was performed due to the suspicion of rectal varices based on the history and CT scan results. Colonoscopy showed numerous rectal polyps emerging up to 10 cm from the anus. Stalked or sessile polyps of various sizes were observed on the entire lumen of the rectum with some normal intervening mucosa. A few protruding vessels were identified. The polyp mucosa was covered with yellow-white fibrinous exudates and tortuous, dilated, superficial blood vessels were noted on their tips (
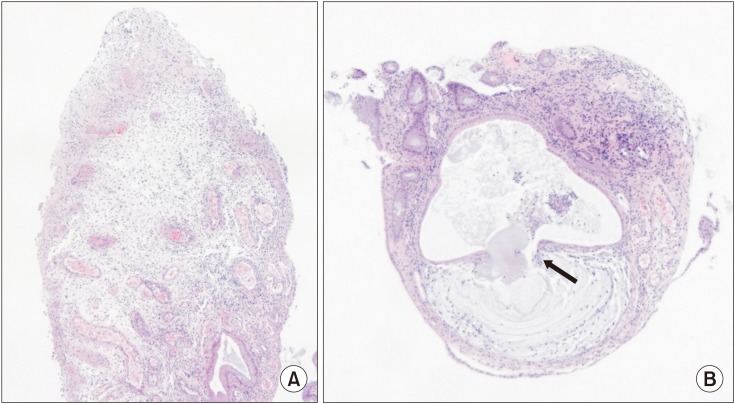
Fig. 2). The entire colon and terminal ileum, except the rectum, were unremarkable. Biopsy specimens obtained from the tip of a polyp revealed diffused lymphocytic infiltration, crypt dilatation, mucinous infiltration of the crypt, and surface ulcerations (
Fig. 3). These findings confirmed the cause of bleeding to be secondary to multiple rectal polyps.
Fig. 2
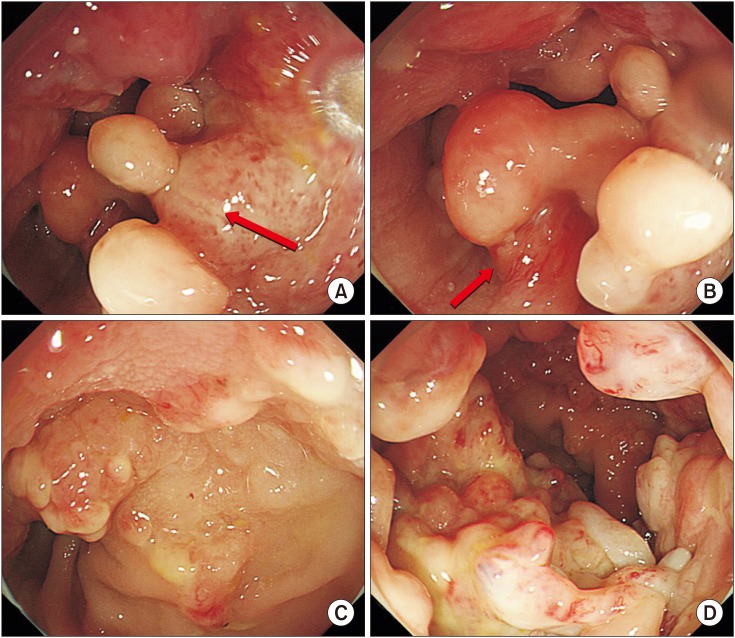
Diffuse, irregular, marginated, light-red capillary malformations on the trunk (A) and lateral aspect of the lower extremities (B), which are characteristic findings in Klippel-Trenaunay syndrome called port-wine stains. Hypertrophy of the right upper extremity (A) and macrodactyly of the right second toe (C) was also observed.

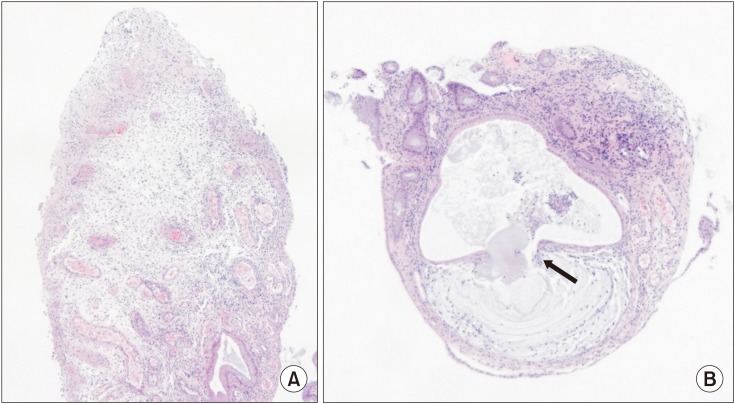
Fig. 3
(A) Histology of the rectal polyp showing diffuse lymphocytic infiltration, crypt dilatation, mucinous infiltration of the crypt, and surface ulcerations. (B) Mucus retained inside the expended crypt ruptured into the lamina propria (arrow) (H&E, ×40).
Although the hugely dilated aberrant vein in the abdomen was considered a venous malformation, other abnormal findings were also noted in the systematic physical examination including subtle hypertrophy of the right upper extremity and light red-colored port wine stains on the trunk and the lateral aspect of the lower extremities (
Fig. 4). Additionally, no prominent difference was observed in the thickness of the lower extremities despite macrodactyly on the right second toe. Taken together, the characteristic port wine stains, right upper extremity hypertrophy, and abdominal venous malformation meet the classic triad of KTS. Hence, KTS was diagnosed.
Fig. 4
(A) Coronal and (B, C) axial sections of contrast enhanced abdominal computed tomography showing a huge dilated vein (arrow), the upper portion of which drains into the splenic vein while the lower portion drains into the left internal ileac vein through the superior and middle rectal veins (A-C). (C) Congested small vessels are seen developing around the rectum (arrowhead). (B, C) Circumferential thickening of the rectum is observed along with irregularity and narrowing of the lumen.
Various kinds of interventions, including radiologic and surgical treatment, were considered for the treatment of the abnormal abdominal vascularity found in this patient. However, his parents opted to postpone aggressive treatment, and he was therefore prescribed oral iron supplementation. The patient continues to have intermittent hematochezia but his hemoglobin level is maintained at 15.5 mg/dL with intermittent oral iron supplementation.
DISCUSSION
KTS is a disease that affects the development of blood vessels, skin, muscles, and bones. The disease can affect all organs including the GI tract. Most KTS patients experience symptoms without major complications. However, depending on the location of the affected organs and the degree of involvement, KTS can give rise to serious complications such as pulmonary thromboembolism [
3] and heart failure secondary to the formation of large arteriovenous malformations characteristic of the disease [
4]. Most cases of GI involvement in KTS are either asymptomatic or mildly symptomatic; few reports of severe hematochezia and mortality exist [
156].
The majority of the GI manifestations associated with KTS present as vascular malformations around the GI tract. Occasionally, these exposed vessels erode and lead to serious bleeding into the GI tract [
1567]. However, bleeding can also occur from esophageal varices secondary to intraabdominal vascular malformations and thrombosis [
2].
In this case, majority of the lesions found were in the form of multiple rectal polyps, although a few small blood vessels were also observed protruding directly into the mucosa. The length of the polyps did not reach 10 cm, although hardly any normal mucosa was found in the affected region and nearly the entire lumen was covered in polyps and fibrinous exudates. Pathological examination of the polyp tip revealed diffuse mucosal ulceration, lymphocytic infiltration, and crypt dilation; these dilated crypts were filled with fibrinous mucin. Based on CT, endoscopic, and histopathologic findings, rectal polyposis in this patient seems to have been caused by chronic irritation of small, congested vessels protruding to the rectal mucosa; this finding is called cap polyposis and has been observed in several reported cases [
8910]. ‘Cap’ is the name given to the inflammatory granulation tissue attached to the polyp head. Typical endoscopic findings of cap polyposis include the presence of multiple polyps, often located in the rectum, covered by a thick layer of fibrinopurulent exudates [
9]. The pathogenesis of cap polyposis is still unclear as multiple mechanical, infectious, and inflammatory mechanisms can provide possible explanations for the phenomenon. Since polypectomy was not performed due to the suspicion of protruding vessels below the polyp, no histologic finding representative for the entire polyp was obtained. Nevertheless, considering the location of the lesions, as well as the typical endoscopic and histologic findings obtained, a diagnosis of cap polyposis appears reasonable.
The patient was thought to have bleeding secondary to multiple rectal polyps that arose from the direct protrusion of vessels or varices [
26]. Fortunately, this patient presented with severe IDA secondary to long term chronic blood loss without the presence of shock or massive bleeding. The patient's hemoglobin levels were stabilized with intermittent oral iron supplementation despite intermittent episodes of hematochezia. However, the persistence of the patient's vascular malformations and polyps may lead to further problems and require definitive treatment in the future.
In conclusion, KTS is a very rare disease with infrequent GI involvement. Symptoms can range from asymptomatic, obscure blood loss to massive, life-threatening bleeding. GI specialists should be able to diagnose KTS especially if there are findings of an unexplained vascular malformation in the GI tract or abdominal cavity. The symptoms of KTS are mostly caused by a direct vascular malformation in the GI tract, but may also arise secondary to vascular malformations as was the case in our patient. We hereby report a meaningful case of KTS that presented with rectal polyposis.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download