Abstract
Objectives
Methods
Results
Figures and Tables
Table 2
Multiple linear regression results by model
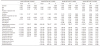
Model 1 was adjusted for age, sex, smoking, hypertension, diabetes mellitus, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens. Model 2 was adjusted for age, sex, smoking, hypertension, diabetes mellitus, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens, S. mitis, S. mutans, S. sobrinus, L. casei, and total bacterial load. Model 3 was adjusted for age, sex, smoking, number of cigarettes per a day, hypertension, diabetes mellitus, heart diseases, lung diseases, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens, S. mitis, S. mutans, S. sobrinus, L. casei, and total bacterial load. Model 4 was adjusted for age, sex, number of planned tooth extractions, smoking, number of cigarettes per a day, hypertension, diabetes mellitus, heart diseases, lung diseases, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens, S. mitis, S. mutans, S. sobrinus, L. casei, and total bacterial load.
SE, Standard error.
Table 3
Comparison of accuracy between convolutional neural network and multiple linear regression for each model
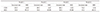
Model 1 was adjusted for age, sex, smoking, hypertension, diabetes mellitus, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens. Model 2 was adjusted for age, sex, smoking, hypertension, diabetes mellitus, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens, S. mitis, S. mutans, S. sobrinus, L. casei, and total bacterial load. Model 3 was adjusted for age, sex, smoking, number of cigarettes per a day, hypertension, diabetes mellitus, heart diseases, lung diseases, A. actinomycetemcomitans, P. gingivalis, T. forsythus, F. nucleatum, P. intermedia, and P. nigrescens, S. mitis, S. mutans, S. sobrinus, L. casei, and total bacterial load. Model 4 was adjusted for age, sex, number of planned tooth extractions, smoking, number of cigarettes per a day, hypertension, diabetes mellitus, heart diseases, lung diseases, A. actinomycetemcomitans, P. gingivalis, T. forsythus, P. intermedia, P. intermedia, and P. nigrescens, S. mitis, S. mutans, S. sobrinus, L. casei, and total bacterial load.
CNN, Convolutional neural network; MLR, Multi-variable linear regression; MSE, Mean squared error.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download