Abstract
Purpose
The purpose of this study was to find the factors affecting the decisional conflict of patients undergoing chemotherapy.
Methods
Participants were 137 patients undergoing chemotherapy in a hospital. The Quality Quantity Questionnaire, a distress thermometer and the Decisional Conflict Scale were used to gather self-reported data. The collected data were analyzed using descriptive statistics, t-tests, ANOVA, post-hoc Scheffe's tests, Pearson's correlations coefficients and stepwise multiple regression.
Results
The decisional conflict showed that the score for severe to high distress groups were higher than that of the mild distress group. The levels of distress and satisfaction of chemotherapy decisional conflict were positively correlated (p=.043). Decisional conflict was significantly affected by age (p=.041), the burden of treatment costs (p=.047), the support system(p=.049), the current feeling of health(p=.024), and comorbidity (p=.039). The significant predictors of decisional conflict were support system, current feeling of health, age, and the burden of treatment costs, which explained 15% of the variance.
Figures and Tables
Table 1
Differences in Attitudes Towards Treatment, Distress and Conflicts of Chemotherapy Decision-making by Demographic and Ilness-related Characteristics (N= 137)
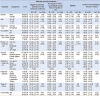
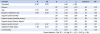
Table 2
Scores and Component Means of Attitudes Towards Treatment, Distress and Conflicts of Chemotherapy Decision Making (N= 137)

Table 3
Comparison of Attitudes Towards Treatment & Conflicts of Chemotherapy Decision Making between the Distress Groups (N= 137)

References
1. Statistics Korea. Cause of death statistics in 2018 [Internet]. Accessed November 18, 2019. Available from: http://kostat.go.kr/wnsearch/search.jsp.
2. Yarbro CH, Wujcik D, Gobel BH. Cancer nursing: principles and practice. 8th ed. Burlington, MA: Jones and Bartlett Learning;2016.
3. Meropol NJ, Egleston BL, Buzaglo JS, Benson AB 3rd, Cegala DJ, Diefenbach MA, et al. Cancer patient preferences for quality and length of life. Cancer. 2008; 113:3459–3466.

4. Kwon EJ, Yi M. Distress and quality of Life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012; 12:289–294.

5. Seo JY, Yi M. Distress and quality of life in cancer patients receiving chemotherapy. Asian Oncol Nurs. 2015; 15:18–27.

6. Kim GM, Kim SJ, Song SK, Kim HR, Kang BD, Noh SH, et al. Prevalence and prognostic implications of psychological distress in patients with gastric cancer. BMC Cancer. 2017; 17:283.

7. Whelan T, Levine M, Willan A, Gafni A, Sanders K, Mirsky D, et al. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery: a randomized trial. JAMA. 2004; 292:435–441.

8. Lee SM, Kim S, Lee HS. The process of medical decision-making for cancer patients. Korean J Med Ethics. 2009; 12:1–14.

9. Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012; 367:1616–1625.

10. Kim B, Hwang SK. Attitudes toward treatment and decisional conflict in cancer patients receiving chemotherapy in Korea. J Korean Data Anal Soc. 2016; 18:1829–1844.
11. Stiggelbout AM, Jansen SJ, Otten W, Baas-Thijssen MC, van Slooten H, van de Velde CJ. How important is the opinion of significant others to cancer patients' adjuvant chemotherapy decision-making? Support Care Cancer. 2007; 15:319–325.

12. Baek SK, Kim SY, Heo DS, Yun YH, Lee MK. Effect of advanced cancer patients' awareness of disease status on treatment decisional conflicts and satisfaction during palliative chemotherapy: a Korean prospective cohort study. Support Care Cancer. 2012; 20:1309–1316.

13. Lee HJ, Yang JH. Factors influencing older patients' participation in decision making regarding cancer surgery. J Korean Gerontol Nurs. 2013; 15:1–10.
14. Yoon YS, Kim MH, Park JH. Perception of shared decision-making and conflict decision-making related to surgery in elderly patients with cancer. J Korean Gerontol Nurs. 2014; 16:266–275.

15. Koo NY, Lee JH. Factors influencing conflicts of chemotherapy decision making among pre-operative cancer patients. Asian Oncol Nurs. 2017; 17:69–78.

16. Stiggelbout AM, de Haes JC, Kiebert GM, Kievit J, Leer JW. Tradeoffs between quality and quantity of life: development of the QQ Questionnaire for cancer patient attitudes. Med Decis Making. 1996; 16:184–192.
17. National Comprehensive Cancer Network. Distress management [Internet]. Accessed December 20, 2017. Available from: http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf.
18. O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995; 15:25–30.
19. Yun YH, Lee MK, Park S, Lee JL, Park J, Choi YS, et al. Use of a decision aid to help caregivers discuss terminal disease status with a family member with cancer: a randomized controlled trial. J Clin Oncol. 2011; 29:4811–4819.

20. Kim YJ, Kim KH, Yang SH, Kwak YH. Distress and resilience of lung cancer patient receiving chemotherapy. J Korea Soc Wellness. 2016; 11:289–302.

21. Seo MH, Lim KH. The effects of fatigue and distress on self-efficacy among breast cancer survivors. Korean J Adult Nurs. 2016; 28:378–387.

22. Wi ES, Yong JS. Distress, depression, anxiety, and spiritual needs of patients with stomach cancer. Asian Oncol Nurs. 2012; 12:314–322.

23. Poe JK, Hayslip JW, Studts JL. Decision making and distress among individuals diagnosed with follicular lymphoma. J Psychosoc Oncol. 2012; 30:426–445.

24. Jabbour J, Dhillon HM, Shepherd HL, Sundaresan P, Milross C, Clark JR. The relationship between role preferences in decision-making and level of psychological distress in patients with head and neck cancer. Patient Educ Couns. 2018; 101:1736–1740.

25. Gopal N, Kozikowski A, Barginear MF, Fishbein J, Pekmezaris R, Wolf-Klein G. Reasons for chemotherapy refusal or acceptance in older adults with cancer. South Med J. 2017; 110:47–53.

26. Shin N, Kim JY. Experience of chemotherapy in ovarian cancer patients. Asian Oncol Nurs. 2017; 17:158–169.

27. Kim SI, Lee Y, Son Y, Jun SY, Yun S, Bae HS, et al. Assessment of breast cancer patients' knowledge and decisional conflict regarding tamoxifen use. J Korean Med Sci. 2015; 30:1604–1610.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download