I. Introduction
A ranula is a mucocele caused by extravasation of the sublingual gland on the floor of the mouth. The most common presentation is a cystic mass on the floor of the mouth. Ranulas can be induced by pooled mucin from ruptured acini of the sublingual gland or a ruptured duct of Rivinus. Because ranulas are lined with granulation tissue instead of epithelium, they are considered a type of pseudocyst
12.
In such conditions, there is a dehiscence in the mylohyoid muscle. A portion of the sublingual gland may herniate through this hiatus, and its extravasated mucin can spread along this hiatus into the submandibular and submental space. This phenomenon is called a plunging ranula
3. Although trauma is traditionally thought to be the cause of ranula development, only 2.8% of patients demonstrated the history of trauma in Zhao's study
2. A different study proposed ductal obstruction and congenital malformation as possible etiologies
4.
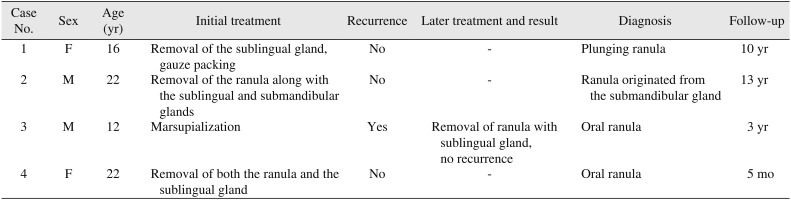
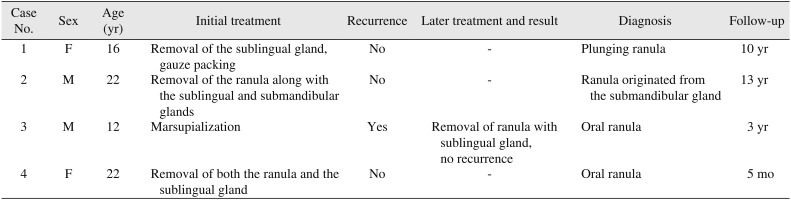
Various treatments for ranula have been suggested, and each treatment has shown a diverse success rate. Therefore, this article describes the cases of simple ranula and plunging ranula and discusses their appropriate management with reference to the literature.
Go to :

III. Discussion
Ranulas can be classified into three groups. Oral ranulas present with intraoral swelling only, while a pluning ranula exhibits cervical swelling without swelling of the mouth floor. A mixed ranula has both intraoral and cervical swelling
2.
Various treatments for ranulas have been suggested. These include sclerotherapy with OK-432, marsupialization, incision and drainage, aspiration of cystic fluid, ranula excision only, and excision of the sublingual gland with or without ranula excision
13567.
Yoshimura et al.
8 compared three different methods of ranula treatment. The recurrence rate was 25.0% for the excision of the ranula only, 36.4% for marsupialization, and 0% for excision of sublingual gland along with the ranula. Their study concluded that removal of the sublingual gland with the ranula was the most effective treatment modality.
Zhao et al.
2 compared the recurrence rates of 580 ranulas treated using different surgical methods. They showed that recurrence was not associated with the type of ranula, but was correlated with the surgical method; the recurrence rate was 66.7% for marsupialization, 57.69% for excision of the ranula, and 1.2% for excision of the sublingual gland either with or without the ranula. Their study stressed that transoral sublingual gland removal was a basic and essential measure required to reduce the recurrence of any type of ranula.
Harrison
3 surveyed the literature about the success rate of ranula treatments. In oral ranulas, the success rate was 100% for the removal of the sublingual gland, 99% for removal of both the sublingual gland and the ranula, 63% for the removal of the ranula only, 55% for marsupialization only, 82% for marsupialization with packing, 73% for injection of OK-432, and 0% for incision and drainage. In plunging ranulas, the success rate was 96% for the removal of the sublingual gland, 95% for removal of both the sublingual gland and the ranula, 38% for the removal of the ranula only, 38% for marsupialization only, 100% for marsupialization with packing, 59% for the injection of OK-432, and 4% for incision and drainage. For plunging ranulas, excision of the sublingual gland had an almost 100% success rate, and the addition of marsupialization with packing could further reduce the failure rate. In the case of excision of the sublingual gland, the success rate was not 100% in all cases, which meant a sublingual gland that was source of extravasion had not been removed completely.
Shelley et al.
9 reported on patients with extensive plunging ranulas. The initial lesion was a simple ranula managed by marsupialization only. However, the lesion recurred as a massive plunging ranula. Although extensive plunging ranula may penetrate into peripheral areas, this type of ranula can still be managed by the transoral removal of the sublingual gland and drainage of the cystic fluid.
Several authors have reported that marsupialization has resulted in a high rate of recurrence: 66.76% by Zhao et al.
2, 61% by Crysdale et al.
7, 52.6% by Parekh et al.
4, and 20% by Patel et al.
10.
Marsupialization performed with unroofing drains the cystic fluid and causes the collapse of the cavity, which quickly heals the oral surface or roof of the ranula and isolates the ranula from the mucosa of the floor of the mouth. The causative extravasation is usually located in the deeper portion of the sublingual gland, so the source of leakage is not eliminated, and the ranula therefore has a tendency to recur within several weeks. To reduce the incidence of recurrence, a modified marsupialization including packing of the cavity with gauze has been introduced instead of leaving the unroofed ranula cavity open with subsequent collapse of the cystic cavity. Gauze packing can bring about the fibrosis of ruptured acini of the sublingual gland and seal the leaking area
11.
Morita et al.
12 reported that marsupialization can be a useful treatment method for small-sized oral ranulas. In a report of nine patients treated with marsupialization, the ranulas only recurred in three patients. Baurmash
13 was against sublingual gland removal for the treatment of oral ranula regardless of size and stressed that if the cyst is shallow and superficial, marsupialization with unroofing can be used to achieve low recurrence rates.
Marsupialization and simple cyst removal have varying success rates, but their recurrence rates are thought to depend on complete removal of the cyst along with the involved sublingual gland
2. Removal of the sublingual gland is the recommended primary treatment for plunging ranulas.
According to Crysdale et al.
7, when the ranula is excised along with the involved sublingual gland, the success rate is almost 100%; it is recommended that oral ranulas greater than 1 cm in diameter and plunging ranulas should be treated by excision of the ranula along with the sublingual gland as a primary therapy. If the ranula recurs after marsupialization, the involved sublingual gland must be removed
1.
Instead of total removal of the sublingual gland, Chung et al.
14 reported that partial sublingual glandectomy with ranula excision, which removes the feeding portion and degenerative acinar cells, yielded good outcomes. As a new conservative method, Chung et al.
14 recommended a partial removal of the affected sublingual gland. However, that study only included 10 patients, and 1 of these experienced a recurrence after partial removal. Therefore, further research will be needed.
Complications may occur due to damage to the lingual nerve and submandibular duct during excision of the sublingual gland. Careless manipulation of the distal lingual nerve may lead to paresthesia of the tongue and stenosis of the submandibular duct due to extensive scarring, which may further lead to obstructive submandibular sialadenitis. Baurmash
1113 insisted that to reduce the incidence of this complication, complete removal of the ranular component may not be necessary. In addition, ductal laceration may induce additional salivary leakage
11.
There is a dispute over the need for a transcervical incision when treating a plunging ranula. The most common cause of plunging ranula is a herniated portion of extravasated mucin that protrudes through the mylohyoid muscle from the sublingual gland. Plunging ranulas are also considered to be peusdocysts, which means there is no need for removal of the epithelial lining. So, if a problematic sublingual gland is to be excised transorally, there is no need for a transcervical approach except in the case of plunging from the submandibular gland
6.
In ranulas that originate from the submandibular gland, it is essential to excise the ranula along with the submandibular gland through a cervical approach. When the sublingual gland sticks to the ranula, it is wise to remove this sublingual gland along with the submandibular gland at the same time
6. Kim and Simental
15 also recommended that transoral removal of the sublingual gland with placement of a drain to the left of the residual ranula cavity for two weeks can avoid the morbidity associated with invasive therapy without requiring a transcervical approach.
Injection of a sclerosing agent such as OK-432 into the cavity of the ranula has been shown to be a highly effective treatment method for cystic lesions, including ranulas
11016. The cytokines released after an injection of OK-432 induce inflammation in the cystic wall, fibrosis, and eventual shrinkage of the cyst
16. According to Kono et al.
16, the result was a complete regression in 78.2% of patients and a partial regression in 13%. However, a 100% rate of recovery was not possible
10. Although they were not severe, fever and painful swelling after injection with OK-432 have been reported as side effects. Because no patients reported damage to the facial nerve and there were few complications compared to surgery, OK-432 may be the method of choice for treatment of ranulas, especially in pediatric populations1. For complete regression, however, multiple injections are sometimes required; if there is no response to OK-432, surgery should be carried out
10.
After reviewing several cases and the literature
236791114, our department established a strategy for the treatment of ranulas. Because the source of leakage of mucus into the surrounding tissue is the sublingual gland itself, ranulas should be excised together with the involved sublingual salivary gland except in the case of a superficial, small oral one. In very small, superficial oral ranulas, marsupialization can be considered. Transoral excision must be carried out along with preservation of the Wharton's duct and the lingual nerve. The ranula's cystic wall is fragile and difficult to remove completely; sometimes a portion remains following surgery. Because ranulas have no true epithelial lining, removal of the cystic component is not mandatory; the residual cystic wall does not cause any problem. In contrast, removal of the sublingual gland is of the utmost importance. In plunging ranulas, transoral excision of the sublingual gland is required, but it is not necessary to remove cystic wall completely. The transcervical approach might leave a noticeable scar without any prominent effects. In questionable cases, drain or gauze packing may also be helpful. Recurrent oral ranulas must be excised along with the sublingual gland. Ranulas that arise from the submandibular gland are difficult to remove transorally, so a transcervical approach should be used in those patients.
Go to :