INTRODUCTION
Uterine sarcoma is a rare malignant tumor with a poor prognosis, comprising 1% of all female genital tract malignancies and 3%–7% of all uterine cancers [
12]. In general, uterine sarcoma is diagnosed pathologically after surgery in postmenopausal women [
3]. According to World Health Organization (WHO) classification of tumors of the uterine corpus [
4], there are two main subgroups of uterine sarcoma: mesenchymal tumors and mixed epithelial and mesenchymal tumors. Malignant mesenchymal tumors can be further classified into leiomyosarcoma, endometrial stromal sarcoma with undifferentiated sarcoma, and miscellaneous tumors. Mixed tumors can be categorized as adenosarcoma and carcinosarcoma, along with malignant mixed Müllerian tumor (MMMT). Carcinosarcoma is currently considered as an endometrial carcinoma, but is still classified as uterine sarcoma in most retrospective studies, as well as in the WHO classification.
Uterine sarcomas are sometimes misdiagnosed as uterine fibroids and are not correctly diagnosed until after myomectomy or hysterectomy because of their rare prevalence and a lack of specific diagnostic techniques. Several studies and systemic reviews have revealed that the rate of unexpected uterine sarcomas among women who undergo surgery for presumed benign leiomyomas ranges from 0.1% (1 in 2,000) to 0.4% (1 in 278) [
56]. And one study reported that the risk of unsuspected uterine sarcoma increases with age to range from 1.74 in 1,000 for patients aged 25–29 years to 10.1 in 1,000 for patients aged 75–79 years [
7]. Although this frequency is low, when this pathology occurs, there is a risk of tumor seeding because of unplanned resection of sarcomas and delayed treatment. To prevent misdiagnosis of uterine sarcomas, many studies have described the clinical characteristics of uterine sarcomas as compared with uterine fibroids, suggesting that rapid growth and postmenopausal bleeding could be risk factors of uterine sarcomas [
8].
Based on several ultrasonographic findings, some studies have suggested that uterine sarcomas were likely to appear as solid masses with heterogeneous echogenicity that as well as enhanced vascularity [
9], and that Doppler measurement of the resistance index (RI) may be a useful diagnostic tool [
1011]. However, there have been few studies supporting those data. Moreover, there were no studies focused on the characteristics of pathologic proved uterine sarcomas preoperatively misdiagnosed as benign uterine leiomyomas.
Therefore, we analyzed the sonographic and clinical characteristics of uterine sarcoma that was misdiagnosed as uterine fibroid before surgery in late reproductive age.
Go to :

MATERIALS AND METHODS
A total of 61 patients with over 35 years old were preoperatively diagnosed with uterine fibroids by ultrasonography, and uterine sarcomas were later confirmed after myomectomy or hysterectomy at Asan Medical Center between January 2005 and December 2018. Medical records and sonographic results of the included patients were retrospectively reviewed. Pathology reports were searched in the electronic medical records using the terms “leiomyosarcoma,” “endometrial stromal sarcoma,” “adenosarcoma,” and “malignant mixed Müllerian tumor.” Patients in whom surgery was initially planned for suspected uterine sarcoma after further imaging studies, such as magnetic resonance imaging, computed tomography, or positron emission tomography, were excluded. The study protocol was approved by the Review Board for Human Research of Asan Medical Center (2019-0681).
Study parameters were classified into three categories: patient characteristics, pathologic characteristics, and ultrasound findings. Patients??characteristics included age at the time of diagnosis with pathologic confirmation, parity, menopausal status, history of taking hormonal therapy, preoperative serum CA-125 level, body mass index (BMI) on preoperative day, and clinical symptoms. Clinical symptoms were defined as patients??chief complaints, used in decision-making regarding surgical treatment, and included abnormal vaginal bleeding, dysmenorrhea, menorrhagia, increased mass size, pelvic pain, palpable mass, and no symptoms. Tumors were pathologically confirmed as leiomyosarcoma, endometrial stromal sarcoma (ESS), adenosarcoma, and MMMT. The 2018 International Federation of Gynecology and Obstetrics (FIGO) staging system was used for all uterine sarcomas. The most recent ultrasonography findings prior to surgery were reviewed and the number of masses, maximum diameter of the largest mass (mm), presence of secondary degeneration (cystic or calcified), margin (regular or irregular with/without lobular shape), echogenicity (homogeneous or heterogeneous), and vascularity on color Doppler (internal or circumferential) were extracted. Cystic wall irregularities and shadowing of masses were also evaluated, if present. All ultrasound images were obtained by transvaginal ultrasonography with or without a transabdominal approach to yield additional information of masses. All images were reviewed by two authors (K.J.H. and K.H.J.). Data of certain patients with Doppler measurement of the RI or pulsatility index of masses were analyzed and RI values were categorized as less than 0.4, 0.4–0.5, and more than 0.5.
Go to :

RESULTS
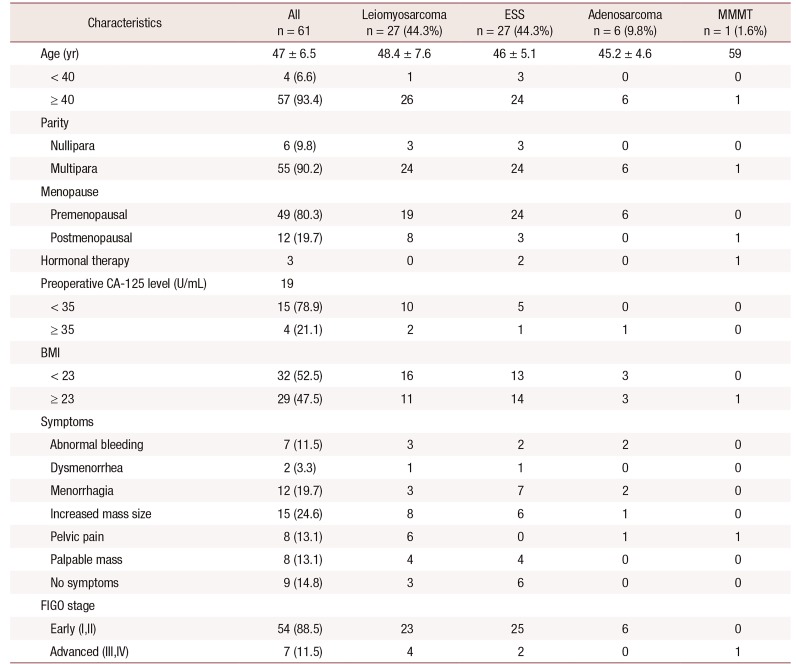
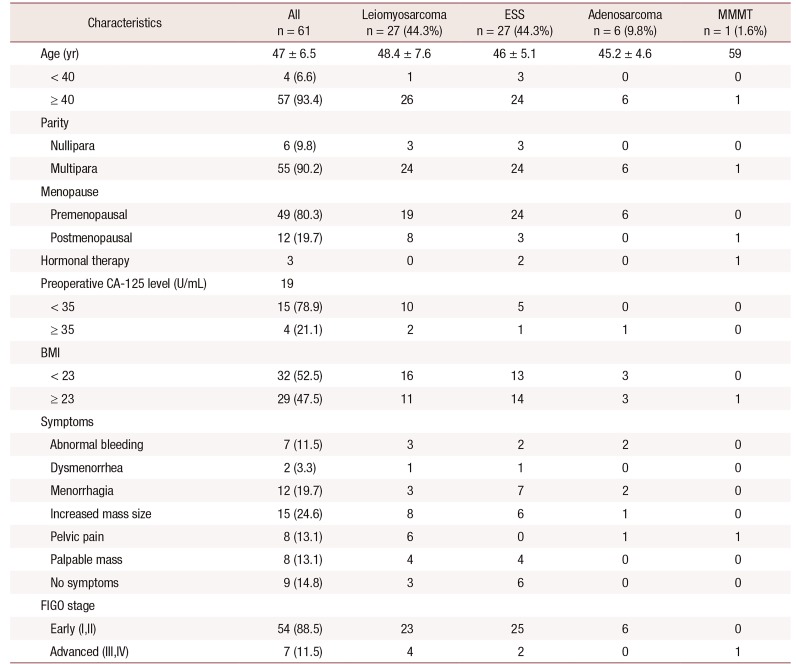
The average age of patients was 47 ± 6.5 (range, 35–66) years and most women were over 40 years old (57/61, 93.4%), multiparous (55/61, 90.2%), and premenopausal (49/61, 80.3%). Only 19 patients had laboratory examination of serum CA-125 level before surgery; of them, 4 patients had serum CA-125 levels over 35 U/mL. Another 42 patients underwent serum CA-125 level testing for the first time after pathologic confirmation of the uterine sarcoma. The proportion of women with BMI under 23 and over 23 was similar (32 patients, 52.5% and 29 patients, 47.5%, respectively). (
Table 1).
Table 1
Clinical characteristics of the patients
|
Characteristics |
All n = 61 |
Leiomyosarcoma n = 27 (44.3%) |
ESS n = 27 (44.3%) |
Adenosarcoma n = 6 (9.8%) |
MMMT n = 1 (1.6%) |
|
Age (yr) |
47 ± 6.5 |
48.4 ± 7.6 |
46 ± 5.1 |
45.2 ± 4.6 |
59 |
|
< 40 |
4 (6.6) |
1 |
3 |
0 |
0 |
|
≥ 40 |
57 (93.4) |
26 |
24 |
6 |
1 |
|
Parity |
|
|
|
|
|
|
Nullipara |
6 (9.8) |
3 |
3 |
0 |
0 |
|
Multipara |
55 (90.2) |
24 |
24 |
6 |
1 |
|
Menopause |
|
|
|
|
|
|
Premenopausal |
49 (80.3) |
19 |
24 |
6 |
0 |
|
Postmenopausal |
12 (19.7) |
8 |
3 |
0 |
1 |
|
Hormonal therapy |
3 |
0 |
2 |
0 |
1 |
|
Preoperative CA-125 level (U/mL) |
19 |
|
|
|
|
|
< 35 |
15 (78.9) |
10 |
5 |
0 |
0 |
|
≥ 35 |
4 (21.1) |
2 |
1 |
1 |
0 |
|
BMI |
|
|
|
|
|
|
< 23 |
32 (52.5) |
16 |
13 |
3 |
0 |
|
≥ 23 |
29 (47.5) |
11 |
14 |
3 |
1 |
|
Symptoms |
|
|
|
|
|
|
Abnormal bleeding |
7 (11.5) |
3 |
2 |
2 |
0 |
|
Dysmenorrhea |
2 (3.3) |
1 |
1 |
0 |
0 |
|
Menorrhagia |
12 (19.7) |
3 |
7 |
2 |
0 |
|
Increased mass size |
15 (24.6) |
8 |
6 |
1 |
0 |
|
Pelvic pain |
8 (13.1) |
6 |
0 |
1 |
1 |
|
Palpable mass |
8 (13.1) |
4 |
4 |
0 |
0 |
|
No symptoms |
9 (14.8) |
3 |
6 |
0 |
0 |
|
FIGO stage |
|
|
|
|
|
|
Early (I,II) |
54 (88.5) |
23 |
25 |
6 |
0 |
|
Advanced (III,IV) |
7 (11.5) |
4 |
2 |
0 |
1 |

The most common symptom among participants was increased mass size (15 patients, 24.6%), followed by menorrhagia (12 patients, 19.7%). As for other symptoms, 7 (11.5%), 8 (13.1%), and 8 (13.1%) women reported abnormal uterine bleeding, pelvic pain, and palpable mass, respectively. Only 2 (3.3%) patients complained of dysmenorrhea. Moreover, as many as 9 (14.8%) patients had no symptoms. Of the 61 patients, the most common histologic types were leiomyosarcoma and ESS (27 patients, 44.3% for both). Six patients (9.8%) had adenosarcoma and only 1 patient (1.6%) had MMMT. Most tumors were FIGO stage 1 and 2 (54 patients, 88.5%). When comparing leiomyosarcoma to ESS, 6 patients had pelvic pain in leiomyosarcoma, but none of the 27 patients of ESS experienced pelvic pain. But menorrhagia was more reported in ESS (7 patients in ESS, 3 patients in leiomyosarcoma) (
Table 1).
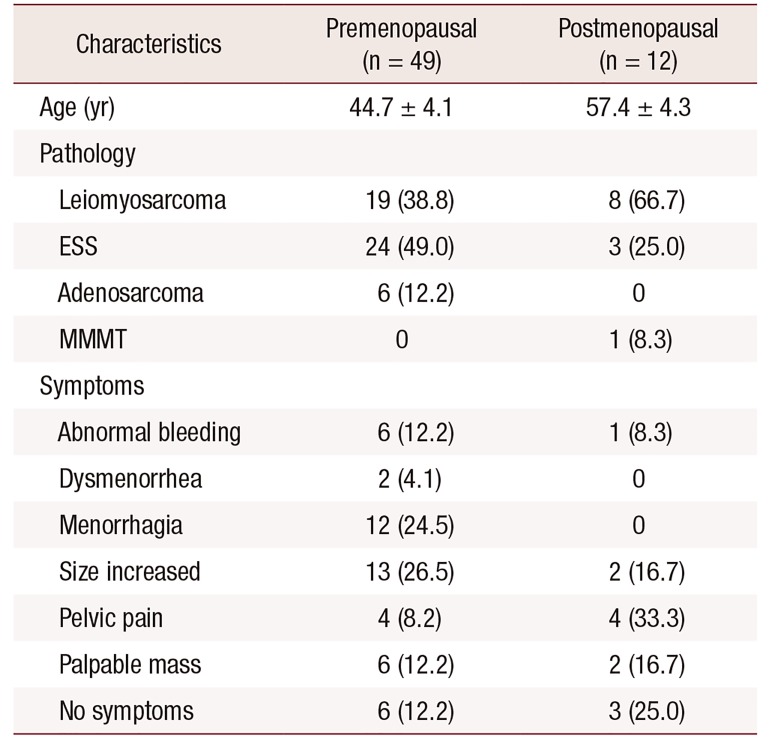
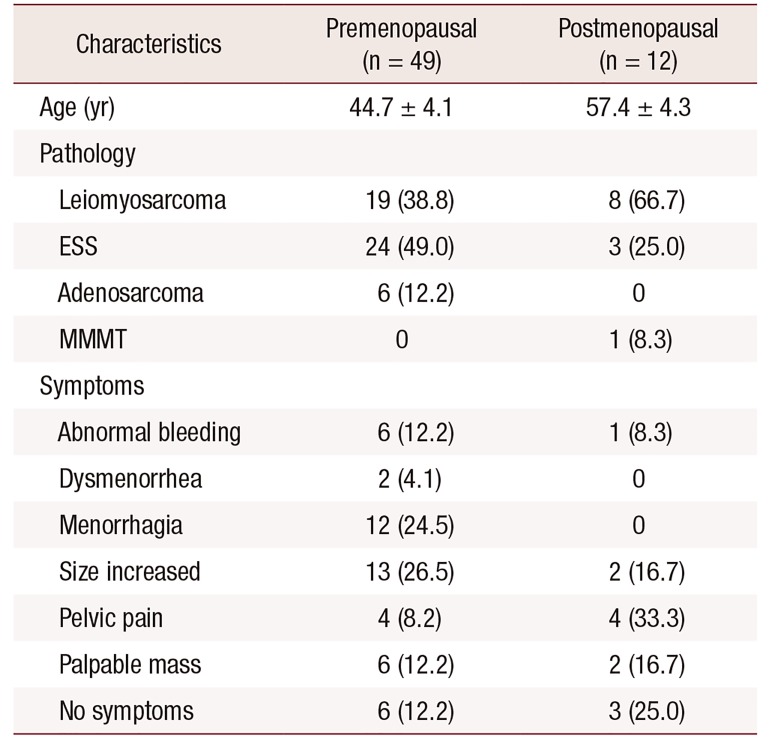
Only 12 patients (20%) were in postmenopausal status with average age of 57.4 ± 4.3 (range, 52–66) years. The most common histologic type was leiomyosarcoma (8/12 patients, 66.7%). The proportion of each symptoms was similar, but 3 patients had no symptoms. In otherwise women with premenopausal status (49 patients, 80.3%), ESS was the most common histologic type (24/49 patients, 49%), and most symptoms was increased mass size (13/49 patients, 26.5%), and menorrhagia (12/49 patients, 24.5%) (
Table 2).
Table 2
Pathology and symptoms of premenopausal and postmenopausal women
|
Characteristics |
Premenopausal (n = 49) |
Postmenopausal (n = 12) |
|
Age (yr) |
44.7 ± 4.1 |
57.4 ± 4.3 |
|
Pathology |
|
|
|
Leiomyosarcoma |
19 (38.8) |
8 (66.7) |
|
ESS |
24 (49.0) |
3 (25.0) |
|
Adenosarcoma |
6 (12.2) |
0 |
|
MMMT |
0 |
1 (8.3) |
|
Symptoms |
|
|
|
Abnormal bleeding |
6 (12.2) |
1 (8.3) |
|
Dysmenorrhea |
2 (4.1) |
0 |
|
Menorrhagia |
12 (24.5) |
0 |
|
Size increased |
13 (26.5) |
2 (16.7) |
|
Pelvic pain |
4 (8.2) |
4 (33.3) |
|
Palpable mass |
6 (12.2) |
2 (16.7) |
|
No symptoms |
6 (12.2) |
3 (25.0) |

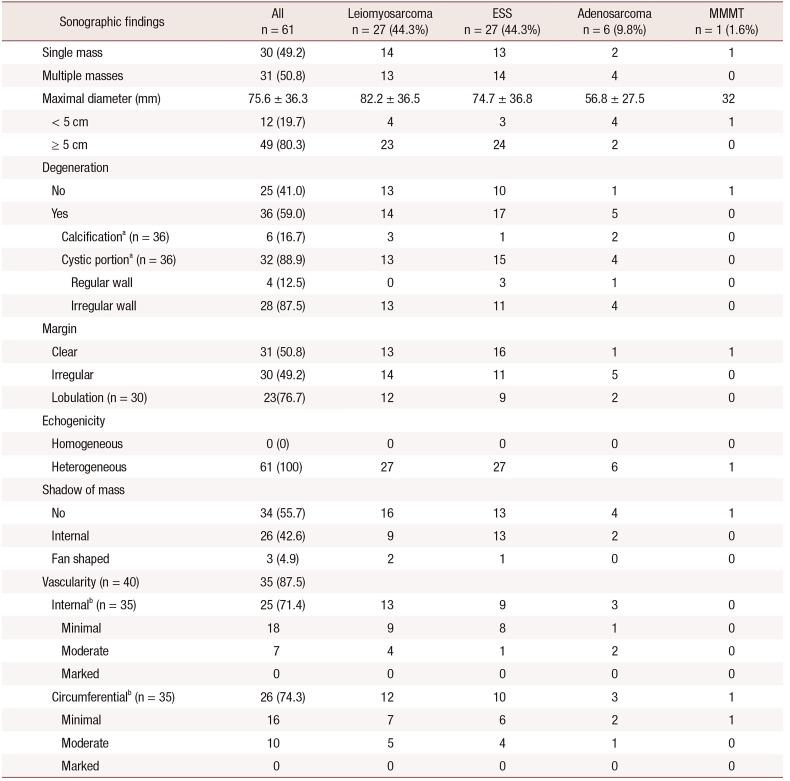
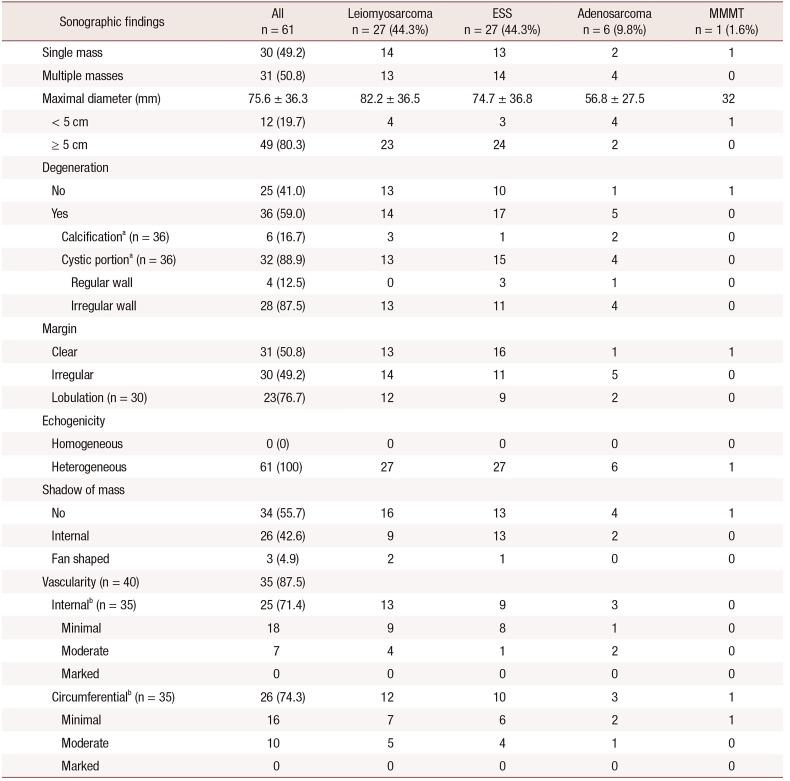
The sonographic findings of patients are shown in
Table 3. Approximately half of women had a single mass (30 patients, 49.2%). The maximum diameter of the largest sarcomas was over 5 cm (49 patients, 80.3%) and the average diameter was 75.6 ± 36.3 mm. The histologic types of sarcomas larger than 5 cm were mostly leiomyosarcoma and ESS, with similar proportions (23/49 patients, 46.9% and 24/49 patients, 49.0%, respectively). But there were no significant differences in sonographic findings among subtypes of uterine sarcoma.
Table 3
Sonographic findings of the included patients
|
Sonographic findings |
All n = 61 |
Leiomyosarcoma n = 27 (44.3%) |
ESS n = 27 (44.3%) |
Adenosarcoma n = 6 (9.8%) |
MMMT n = 1 (1.6%) |
|
Single mass |
30 (49.2) |
14 |
13 |
2 |
1 |
|
Multiple masses |
31 (50.8) |
13 |
14 |
4 |
0 |
|
Maximal diameter (mm) |
75.6 ± 36.3 |
82.2 ± 36.5 |
74.7 ± 36.8 |
56.8 ± 27.5 |
32 |
|
< 5 cm |
12 (19.7) |
4 |
3 |
4 |
1 |
|
≥ 5 cm |
49 (80.3) |
23 |
24 |
2 |
0 |
|
Degeneration |
|
|
|
|
|
|
No |
25 (41.0) |
13 |
10 |
1 |
1 |
|
Yes |
36 (59.0) |
14 |
17 |
5 |
0 |
|
Calcificationa (n = 36) |
6 (16.7) |
3 |
1 |
2 |
0 |
|
Cystic portiona (n = 36) |
32 (88.9) |
13 |
15 |
4 |
0 |
|
Regular wall |
4 (12.5) |
0 |
3 |
1 |
0 |
|
Irregular wall |
28 (87.5) |
13 |
11 |
4 |
0 |
|
Margin |
|
|
|
|
|
|
Clear |
31 (50.8) |
13 |
16 |
1 |
1 |
|
Irregular |
30 (49.2) |
14 |
11 |
5 |
0 |
|
Lobulation (n = 30) |
23 (76.7) |
12 |
9 |
2 |
0 |
|
Echogenicity |
|
|
|
|
|
|
Homogeneous |
0 (0) |
0 |
0 |
0 |
0 |
|
Heterogeneous |
61 (100) |
27 |
27 |
6 |
1 |
|
Shadow of mass |
|
|
|
|
|
|
No |
34 (55.7) |
16 |
13 |
4 |
1 |
|
Internal |
26 (42.6) |
9 |
13 |
2 |
0 |
|
Fan shaped |
3 (4.9) |
2 |
1 |
0 |
0 |
|
Vascularity (n = 40) |
35 (87.5) |
|
|
|
|
|
Internalb (n = 35) |
25 (71.4) |
13 |
9 |
3 |
0 |
|
Minimal |
18 |
9 |
8 |
1 |
0 |
|
Moderate |
7 |
4 |
1 |
2 |
0 |
|
Marked |
0 |
0 |
0 |
0 |
0 |
|
Circumferentialb (n = 35) |
26 (74.3) |
12 |
10 |
3 |
1 |
|
Minimal |
16 |
7 |
6 |
2 |
1 |
|
Moderate |
10 |
5 |
4 |
1 |
0 |
|
Marked |
0 |
0 |
0 |
0 |
0 |

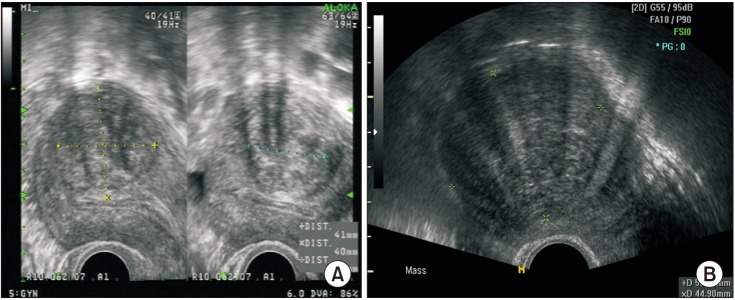
When the margin of masses was evaluated, half of patients had irregular margins (30 patients, 49.2%). Among the 30 patients with irregular margins of tumors, 23 (76.7%) had lobulated margins. All 61 patients showed heterogeneous echogenicity on sonographic imaging. Secondary degeneration of uterine masses was reported in 36 (59%) patients, and approximately 90% of them (32/36, 88.9%) presented with cystic changes. If masses showed cystic degeneration, they mostly had an irregular cystic wall (28 patients, 87.5%). When shadowing of the masses was evaluated, which is typically evident in benign leiomyomas, 34 patients (55.7%) did not show any shadowing patterns. Less than half of patients (27, 44.3%) had masses with internal and fanshaped shadowing (
Fig. 1).
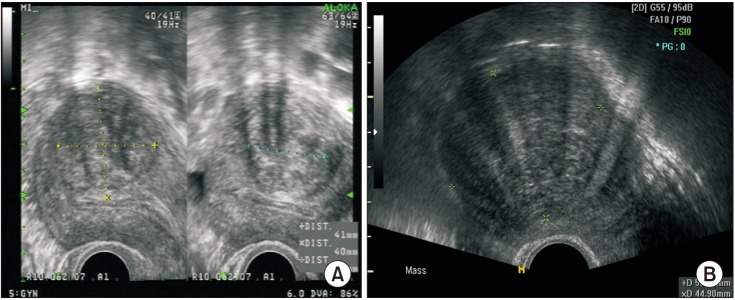 | Fig. 1(A) Internal shadowing of the mass and (B) fan-shaped shadowing.
|
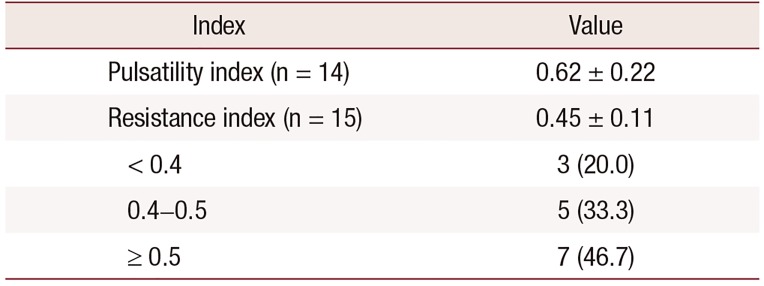
In 40 patients, the vascularity of sarcomas was evaluated, and 35 (87.5%) showed masses with increased vascularity. Vascularization was classified into two categories: internal and circumferential (
Fig. 2), with each type showing the similar proportion (25 patients, 71.4% and 26 patients, 74.3%). Both internal and circumferential vascularity were evident in only 8 patients. Vascularization was minimal to moderate in most patients, and cases of marked vascularity were absent (
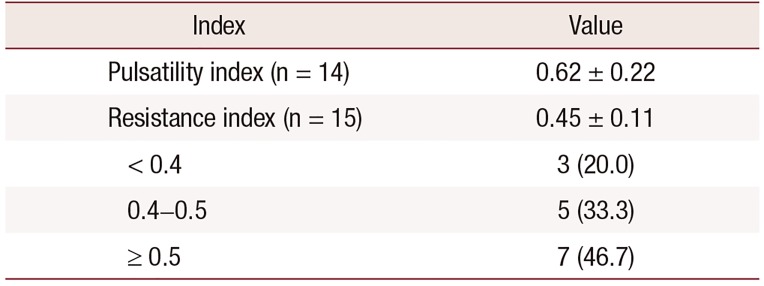
Table 3). As for Doppler indexes, RI was measured in 15 patients, and the mean RI was 0.45 ± 0.11; this was slightly higher than 0.4, which is the cut-off value reported in previous published studies [
11]. Only 3 patients (3/15, 20%) had an RI less than 0.4 (
Table 4).
 | Fig. 2(A) Vascularization on internal Doppler, (B) circumferential Doppler, and (C) both.
|
Table 4
Color Doppler indices
|
Index |
Value |
|
Pulsatility index (n = 14) |
0.62 ± 0.22 |
|
Resistance index (n = 15) |
0.45 ± 0.11 |
|
< 0.4 |
3 (20.0) |
|
0.4–0.5 |
5 (33.3) |
|
≥ 0.5 |
7 (46.7) |

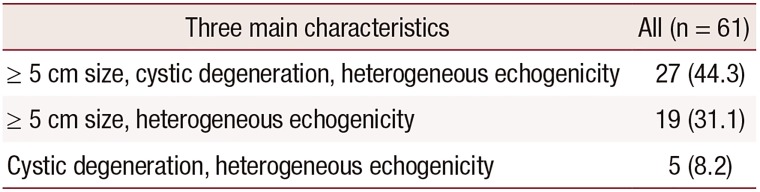
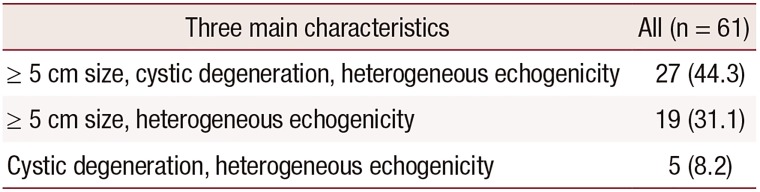
Additionally, subgroup analysis was performed according to three main characteristics of masses: diameter greater than 5 cm, heterogeneous echogenicity, and cystic degeneration. A total 27 (44.3%) patients had all three findings, 19 (31.1%) had both large-sized mass and heterogeneous echogenicity without cystic degeneration, and 5 (8.2%) had both cystic degeneration and heterogeneous echogenicity, but a mass diameter less than 5 cm (
Table 5).
Table 5
Subgroup analysis according to the three main characteristics of the masses
|
Three main characteristics |
All (n = 61) |
|
≥ 5 cm size, cystic degeneration, heterogeneous echogenicity |
27 (44.3) |
|
≥ 5 cm size, heterogeneous echogenicity |
19 (31.1) |
|
Cystic degeneration, heterogeneous echogenicity |
5 (8.2) |

Go to :

DISCUSSION
Here in, we described the sonographic and clinical findings of uterine sarcomas that were misdiagnosed as uterine fibroids in women with late reproductive age. Uterine sarcomas were found associated with increased tumor size (more than 5 cm), heterogeneous echogenicity, and cystic degeneration with irregular walls.
One meta-analysis study of unsuspected uterine sarcoma revealed that uterine sarcoma varies across age groups, and the risk is lower in patients aged under 35 years old [
7]. Hence, we limited the age over 35, considering that uterine sarcoma is common at postmenopausal age and risk of occurrence is elevated after the age of 35.
Regarding the clinical characteristics of uterine sarcomas, recent publications have reported that most patients are symptomatic, and the most common presenting symptom is abnormal vaginal bleeding (at a rate of about 50%) [
8912]. Our results are consistent with those of previous studies in the sense that most patients were symptomatic (52, 85.2%); however, abnormal vaginal bleeding was present in only 11.5% of included patients and increased mass size was the main symptom (24.6%) followed by menorrhagia (19.7%). Other symptoms, such as pelvic pain (13.1%), palpable mass (13.1%), and no symptoms (14.8%), were found in similar proportions. According to these results, we suggest that not only abnormal vaginal bleeding, but also various other symptoms can occur in uterine sarcomas, and patients without symptoms cannot be ignored.
A number of studies have reported that uterine sarcomas are mainly diagnosed in postmenopausal women with presence of tumor growth, abnormal vaginal bleeding and are associated with older age [
813]. Our study showed that most unexpected uterine sarcomas were found among premenopausal women (49/61 patients, 80.3%), and more than half of patients (37/61, 60.7%) were aged 40–49 years. Most of premenopausal patients show increased mass size (13/49, 26.5%) and menorrhagia (12/49, 24.5%). Only 12 patients (19.7%) were postmenopausal women, and 3 of them had no symptoms who were diagnosed uterine mass by accident with health checkup. This outcome means that we should diagnose patients carefully, so as not to miss uterine sarcomas in younger and premenopausal women, especially when they have the symptoms of menorrhagia or increased mass size. It could be same as in asymptomatic postmenopausal women.
On ultrasound, half of sarcomas appeared as isolated masses and the average maximum diameter was 7.56 ± 3.68 cm. One recent large population-based retrospective study of unexpected uterine sarcoma [
14] reported similar values (average diameter 7.16 ± 2.27 cm), but each pathologic type was not described separately. Some reports showed that leiomyosarcomas are larger than ESSs, with a mean diameter of 10 cm vs. 6.2 cm [
1415]. However, we found that most unexpected sarcomas were larger than 5 cm (49 patients, 80.3%), and leiomyosarcoma and ESS had similar mean diameters of 8.2 cm and 7.5 cm, respectively.
According to our results, when degeneration was present, about 90% (88.9%) of sarcomas exhibited cystic changes with irregular cystic walls (87.5%). Calcifications were found in only about 17% of cases. These results are similar to those of a recent multicenter retrospective study describing the ultrasound characteristics of uterine sarcomas. Ludovisi et al. [
9] reported that 87/195 (44.6%) of patients had cystic areas in sarcomas and most cystic areas had irregular walls (67/87, 77%); calcifications were present in 18/195 (9.2%) of cases.
Internal shadows or fan-shaped shadowing is considered important in the diagnosis of uterine fibroids and adenomyosis, but these are rare in sarcomas [
16]. In our study, more than half (34 patients, 55.7%) of sarcomas had no shadowing and only 3 patients exhibited fan-shaped shadowing. Internal shadowing was detected in 26 patients, which was more frequently than expected. This could be because our study was focused on misdiagnosed leiomyomas and not on patients with easily diagnosed sarcoma. Misdiagnosed patients had ultrasound findings that tended to indicate benign diseases.
Several studies have suggested that uterine sarcomas may show irregular vascularity, often with irregular anechoic areas owing to necrosis [
161718]. Ludovisi et al. [
9] reported that 35.5% of uterine sarcomas have minimal or absent vascularity. Exacoustos et al. [
17] found increased peripheral and central vascularity in seven out of eight patients. In the present study about 88% of patients showed increased vascularity, but this mostly involved minimal to moderate vascularity. Sarcomas with marked internal or circumferential vascularization are nonexistent among all types of sarcomas; we can presume that the misclassification was related to these characteristics. If patients exhibit marked increased vascularity, this is suggestive of malignancy and warrants further examination using other imaging methods.
We assessed RI using color Doppler, according to RI cut-off values of 0.4 and 0.5. In previous published studies, RI was lower in patients with sarcoma, and RI values below 0.4 or 0.5 tended to indicate uterine sarcomas. Kurjak et al. [
11] revealed that the RI in sarcomas is 0.37 ± 0.03, which is substantially lower than that detected in myomas (0.54 ± 0.08). Further, Szabó et al. [
10] noted a marked reduction of RI in sarcomas, and the detection rate for sarcoma was just 67% with a cut-off value of 0.5 for RI. However, our results showed that the detection rate of sarcomas was 20% (n = 3) and 53.3% (n = 8) when using cut-off values of 0.4 and 0.5, respectively; this rate was 46.7% (n = 7) with an RI over 0.5. In this study including a small sample size (n = 15), using RI seems to be a poor indicator for the diagnosis of uterine sarcomas.
According to our results, misdiagnosed uterine sarcomas had certain risk factors, such as large mass size over 5 cm, heterogeneous echogenicity, and secondary irregular cystic degeneration. The known benign features of lower vascularity and shadowing patterns were easily detected in included patients.
This study had certain limitations. First, it had no control with uterine fibroid. Hence, clinical and ultrasonographic characteristics found in this study may not specific in unexpected uterine sarcoma. But the characteristics of benign fibroid and uterine sarcoma have been reported in many studies [
916], and we could easily compare those as control group. Second, this study had a small number of enrolled patients. It made that there were no significant differences in clinical and sonographic characteristics among subtypes of uterine sarcoma. Finally, it had limitation of subjective interpretation of ultrasonography. Although two authors reviewed all cases separately and determined the results together, the interpretation of sonographic images might be subjective. Further studies will be needed to find specific characteristics of unexpected uterine sarcoma and differences among subtypes with larger numbers of cases.
In conclusion, our findings suggest that sarcomas initially misdiagnosed as uterine fibroids in women with late reproductive age are usually larger than 5 cm and with heterogeneous echogenicity and irregular cystic degeneration on ultrasonography. However, patients with uterine sarcoma may also exhibit benign features, such as no symptoms, internal shadowing, and low vascularity with an elevated RI index. Therefore, careful consideration is needed to detect more accurately uterine sarcomas before surgery.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download