1. Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 2000. 2014; 64:57–80. PMID:
24320956.

2. Taba M Jr, Kinney J, Kim AS, Giannobile WV. Diagnostic biomarkers for oral and periodontal diseases. Dent Clin North Am. 2005; 49:551–571. viPMID:
15978241.

3. Prasanna JS, Sumadhura C, Karunakar P. Neopterin as a diagnostic biomarker for diagnosis of inflammatory diseases like periodontitis. J Oral Res Rev. 2017; 9:45–49.

4. Ozmeriç N, Baydar T, Bodur A, Engin AB, Uraz A, Eren K, et al. Level of neopterin, a marker of immune cell activation in gingival crevicular fluid, saliva, and urine in patients with aggressive periodontitis. J Periodontol. 2002; 73:720–725. PMID:
12146530.

5. Wiebe CB, Putnins EE. The periodontal disease classification system of the American Academy of Periodontology--an update. J Can Dent Assoc. 2000; 66:594–597. PMID:
11253351.
6. Terheyden H, Stadlinger B, Sanz M, Garbe AI, Meyle J. Inflammatory reaction - communication of cells. Clin Oral Implants Res. 2014; 25:399–407. PMID:
23600659.

7. Silva N, Abusleme L, Bravo D, Dutzan N, Garcia-Sesnich J, Vernal R, et al. Host response mechanisms in periodontal diseases. J Appl Oral Sci. 2015; 23:329–355. PMID:
26221929.

8. Glick M. The curious life of the biomarker. J Am Dent Assoc. 2013; 144:126–128. PMID:
23372117.

9. Tomás I, Regueira-Iglesias A, López M, Arias-Bujanda N, Novoa L, Balsa-Castro C, et al. Quantification by qPCR of pathobionts in chronic periodontitis: development of predictive models of disease severity at site-specific level. Front Microbiol. 2017; 8:1443. PMID:
28848499.

10. Jafri Z, Bhardwaj A, Sawai M, Sultan N. Influence of female sex hormones on periodontium: a case series. J Nat Sci Biol Med. 2015; 6(Suppl 1):S146–S149. PMID:
26604605.

11. Markou E, Boura E, Tsalikis L, Deligianidis A, Konstantinidis A. The influence of sex hormones on proinflammatory cytokines in gingiva of periodontally healthy premenopausal women. J Periodontal Res. 2011; 46:528–532. PMID:
21501171.

12. Gordon CM, LeBoff MS, Glowacki J. Adrenal and gonadal steroids inhibit IL-6 secretion by human marrow cells. Cytokine. 2001; 16:178–186. PMID:
11814313.

13. Güncü GN, Tözüm TF, Cağlayan F. Effects of endogenous sex hormones on the periodontium--review of literature. Aust Dent J. 2005; 50:138–145. PMID:
16238210.
14. Mutneja P, Dhawan P, Raina A, Sharma G. Menopause and the oral cavity. Indian J Endocrinol Metab. 2012; 16:548–551. PMID:
22837914.
15. Cao M, Shu L, Li J, Su J, Zhang W, Wang Q, et al. The expression of estrogen receptors and the effects of estrogen on human periodontal ligament cells. Methods Find Exp Clin Pharmacol. 2007; 29:329–335. PMID:
17805434.

16. Minicucci EM, Pires RB, Vieira RA, Miot HA, Sposto MR. Assessing the impact of menopause on salivary flow and xerostomia. Aust Dent J. 2013; 58:230–234. PMID:
23713645.

17. Yalcin F, Gurgan S, Gul G. Oral health in postmenopausal Turkish women. Oral Health Prev Dent. 2006; 4:227–233. PMID:
17153644.
18. Scardina GA, Messina P. Oral microcirculation in post-menopause: a possible correlation with periodontitis. Gerodontology. 2012; 29:e1045–e1051. PMID:
22212114.

19. Cioffi M, Esposito K, Vietri MT, Gazzerro P, D'Auria A, Ardovino I, et al. Cytokine pattern in postmenopause. Maturitas. 2002; 41:187–192. PMID:
11886764.

20. Yasui T, Uemura H, Tomita J, Miyatani Y, Yamada M, Kuwahara A, et al. Association of interleukin-8 with hot flashes in premenopausal, perimenopausal, and postmenopausal women and bilateral oophorectomized women. J Clin Endocrinol Metab. 2006; 91:4805–4808. PMID:
17018658.

21. Su HI, Freeman EW. Hormone changes associated with the menopausal transition. Minerva Ginecol. 2009; 61:483–489. PMID:
19942836.
22. Malutan AM, Dan M, Nicolae C, Carmen M. Proinflammatory and anti-inflammatory cytokine changes related to menopause. Prz Menopauzalny. 2014; 13:162–168. PMID:
26327849.

23. Mittal S, Kumar A, Gupta RK, Kapoor S, Gulati P, Shukla DK. Comparison of bone mineral density and its variables between premenopausal and postmenopausal women. J Obstet Gynaecol India. 2011; 61:200–204.

24. Corstjens P, Malamud D. Point-of-care diagnostics for infectious diseases. In : Wong DT, editor. Salivary diagnostics. Ames: Wiley-Blackwell;2008. p. 136–149.
25. Farnaud SJ, Kosti O, Getting SJ, Renshaw D. Saliva: physiology and diagnostic potential in health and disease. ScientificWorldJournal. 2010; 10:434–456. PMID:
20305986.

26. Malamud D. Saliva as a diagnostic fluid. Dent Clin North Am. 2011; 55:159–178. PMID:
21094724.

27. Yoshizawa JM, Schafer CA, Schafer JJ, Farrell JJ, Paster BJ, Wong DT. Salivary biomarkers: toward future clinical and diagnostic utilities. Clin Microbiol Rev. 2013; 26:781–791. PMID:
24092855.

28. Barnes VM, Kennedy AD, Panagakos F, Devizio W, Trivedi HM, Jönsson T, et al. Global metabolomic analysis of human saliva and plasma from healthy and diabetic subjects, with and without periodontal disease. PLoS One. 2014; 9:e105181. PMID:
25133529.

29. Zhao HX, Yin SS, Fan JG. High plasma neopterin levels in Chinese children with autism spectrum disorders. Int J Dev Neurosci. 2015; 41:92–97. PMID:
25660944.

30. Yamamoto E, Hirata Y, Tokitsu T, Kusaka H, Tabata N, Tsujita K, et al. The clinical significance of plasma neopterin in heart failure with preserved left ventricular ejection fraction. ESC Heart Fail. 2016; 3:53–59. PMID:
27774267.

31. Raheja UK, Fuchs D, Lowry CA, Stephens SH, Pavlovich MA, Mohyuddin H, et al. Heritability of plasma neopterin levels in the Old Order Amish. J Neuroimmunol. 2017; 307:37–41. PMID:
28495136.

32. Kalantari S, Jafari A, Moradpoor R, Ghasemi E, Khalkhal E. Human urine proteomics: analytical techniques and clinical applications in renal diseases. Int J Proteomics. 2015; 2015:782798. PMID:
26693351.

33. Behringer V, Stevens JM, Leendertz FH, Hohmann G, Deschner T. Validation of a method for the assessment of urinary neopterin levels to monitor health status in non-human-primate species. Front Physiol. 2017; 8:51. PMID:
28220080.

34. Werner ER, Bichler A, Daxenbichler G, Fuchs D, Fuith LC, Hausen A, et al. Determination of neopterin in serum and urine. Clin Chem. 1987; 33:62–66. PMID:
3802497.

35. Murr C, Widner B, Wirleitner B, Fuchs D. Neopterin as a marker for immune system activation. Curr Drug Metab. 2002; 3:175–187. PMID:
12003349.

36. Pradeep AR, Kumar MS, Ramachandraprasad MV, Shikha C. Gingival crevicular fluid levels of neopterin in healthy subjects and in patients with different periodontal diseases. J Periodontol. 2007; 78:1962–1967. PMID:
18062118.

37. Arjunkumar R, Sudhakar U, Jayakumar P, Arunachalam L, Suresh S, Virupapuram P. Comparative analysis of gingival crevicular fluid neopterin levels in health and periodontal disease: a biochemical study. Indian J Dent Res. 2013; 24:582–586. PMID:
24355959.

38. Mahendra L, Mahendra J, Borra SK, Nagarajan A. Estimation of salivary neopterin in chronic periodontitis. Indian J Dent Res. 2014; 25:794–796. PMID:
25728116.

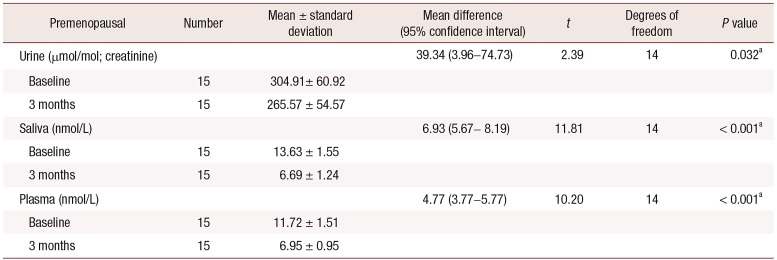
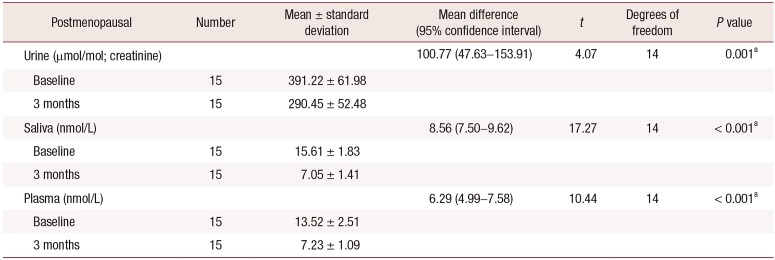
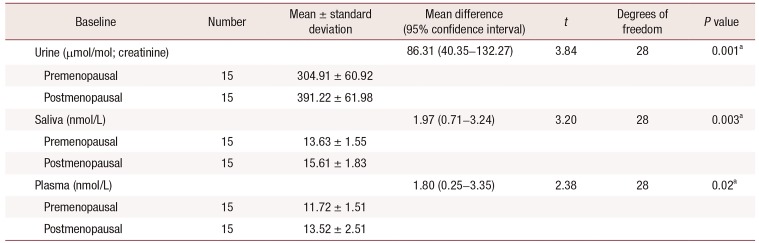
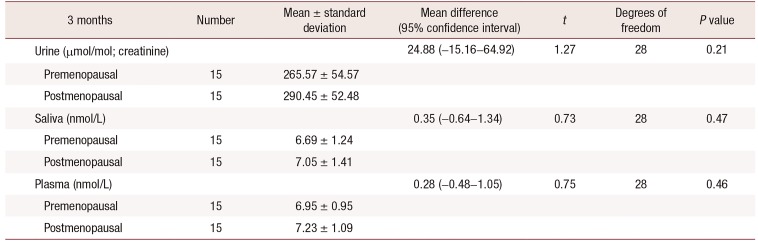
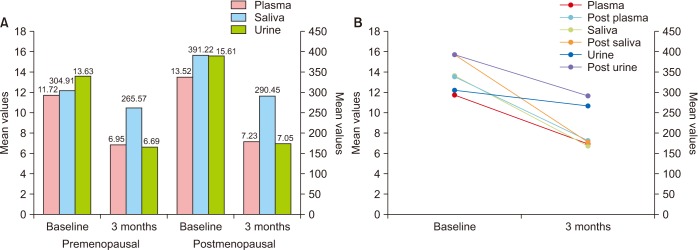
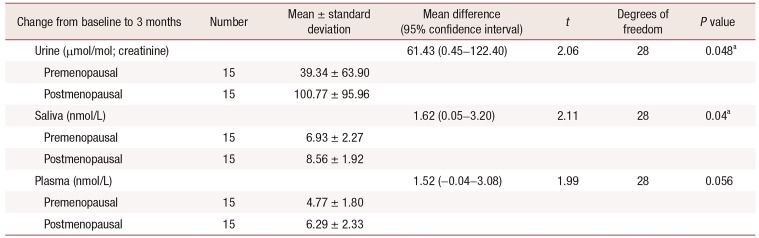
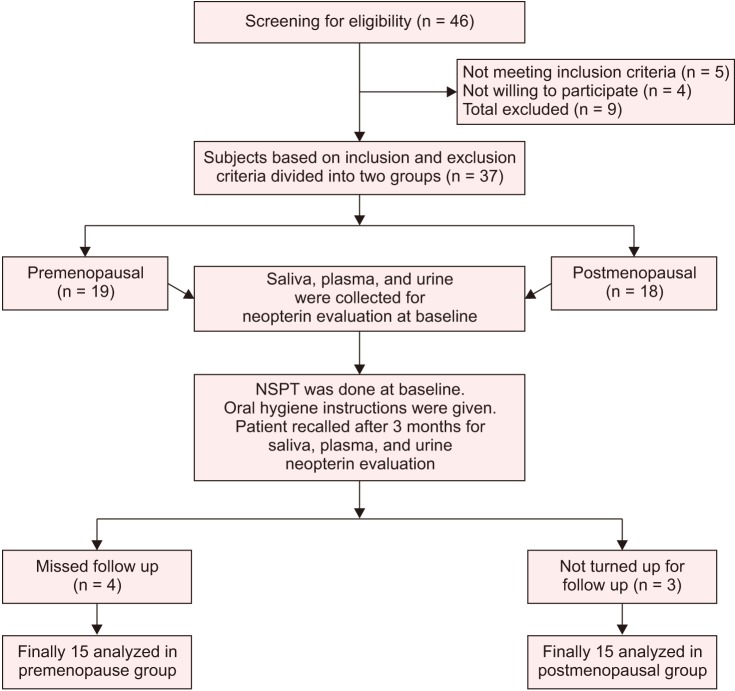
39. Prasanna JS, Sumadhura C, Karunakar P, Rohini N. Comparative evaluation of salivary neopterin levels and its effects to periodontal therapy in pre- and post-menopausal women. J Menopausal Med. 2017; 23:32–41. PMID:
28523257.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download