Abstract
Objectives
Female breast cancer patients generally have limited knowledge regarding issues related to preservation of ovarian function and fertility. The present study aimed to explore the change in the understanding of these issues when female breast cancer patients are educated and counseled about ovarian function and fertility after anticancer treatment.
Methods
One hundred nine young female breast cancer patients completed a questionnaire, which revealed their thoughts and opinions before and after receiving the education about ovarian function and fertility. Their responses were analyzed to determine the impact of the education on their perception and understanding of the aforementioned issues.
Results
The objective survey had four main themes: planning and desire for children, degree of baseline understanding of the effects of anticancer therapy on fertility and ovarian function, resultant change in cognition after education about cancer treatment and its relationship with fertility, and need for education regarding the types of therapies received and their effects on subsequent ovarian function and fertility before treatment.
Conclusions
The preservation of ovarian function and fertility is an important factor that must be included in the discussion prior to initiation of anticancer therapy. Although the study results do not have high educational effectiveness or a high satisfaction with education, there is a need for information and education regarding the impact of anticancer treatment on preservation of ovarian function and fertility.
Breast cancer is the most commonly diagnosed cancer in South Korean women [1]. Due to improvements in early diagnosis and treatment, the mortality rate has declined over the past few years. Approximately 93% of female breast cancer patients survive for more than 5 years [2]. The majority of women diagnosed are postmenopausal, but numbers of young women with breast cancer have been steadily increasing [3].
The prognosis for young women diagnosed with breast cancer appears to be less favorable than that for older women because many young patients tend to have more biologically aggressive forms of the disease [45]. However, if they are diagnosed in the early stages, young female patients are more likely to survive their disease because of improved treatment options. The majority of anticancer treatments, including surgery, chemotherapy, radiotherapy, and endocrine therapy, have substantial effects on gonadal function and may lead to loss of fertility and early menopause [6]. Many breast cancer patients younger than 40 years recover menses within one year from cessation of treatment. The incidence of permanent amenorrhea after anticancer treatment is estimated to be between 33% and 76% in women aged 50 years or younger [7]. Thus, many young female breast cancer survivors have concerns for fertility and ovarian function.
Unfortunately, premenopausal women with breast cancer are not well informed or fully aware of the adverse effects of breast cancer treatment on fertility and ovarian function [89]. Previous studies have demonstrated that patients' knowledge of options for preservation of fertility and ovarian function prior to consultation is generally poor [1011]. Some oncology professionals do not engage in discussion with cancer patients about the preservation of fertility and ovarian function after completion of cancer treatment or even before the onset of therapy, which would have allowed for the consideration of different treatment options [121314]. This may be because of insufficient knowledge of the options and time constraints with premenopausal patients.
In the context of efforts to improve the information provided after cancer diagnosis, the aim of our study is to measure the effects of education on topics of fertility and ovarian function among premenopausal women with breast cancer and to support strategies for delivering that information to young female breast cancer patients. Increased knowledge of the issues related to fertility may influence pre- and post-education decisions.
The study participants were under 35 years of age female patients with a biopsy-proven breast cancer diagnosis immediately. And they were going to be treated including surgical or medical therapy at Asan Medical Center between the years 2016 and 2017.
The participants were 119 patients and given a questionnaire (Supplementary Material 1, available online), which revealed their thoughts and opinions before and after receiving education. Because there were participants who have not completed or submitted the answers, the actual number of people who responded to the questions before and after the watching video is different. Before watching video, only 92 participants were expressed their opinions. After watching video, 109 participants were completed the questionnaire.
Most of the young female with breast cancer participants had a poor level of knowledge regarding preservation of fertility and ovary function [15]. They had had very little or no opportunity to communicate with health professionals regarding the impact of breast cancer treatment on ovarian function and subsequent challenges with fertility.
Before and after watching the audiovisual material each, participants expressed their opinions via survey questionnaires. The video for education of the young female with breast cancer was made by fertility specialist, radiologist, and oncologist at Asan Medical Center. This video was 15 minutes audiovisual material for education and training about overall breast cancer diagnosis and treatment. The complications of anticancer therapy, especially effects on ovarian function and fertility, were significant. To overcome these side effects, preserving therapies of ovarian function and fertility were presented in the video.
Topics covered in the questionnaires included: marital status and planning childbirth, degree of understanding about the side effects of anticancer treatment on ovarian function and fertility, cognitive change after receiving education on the above topic, and the need for information regarding the impact of cancer treatment on fertility and the preservation of ovarian function.
The questionnaire answer choices included yes or no, yes - absolutely, yes - maybe, no - not really, and no - not at all.
We analyzed the questionnaires and used descriptive statistics to calculate results. We have adapted a Microsoft Excel 2016 (Microsoft, Redmond, WA, USA) which reflected as a percentage of categorical data. This study was approved by the Institutional Review Board (IRB) of Asan Medical Center (No. 2019-0810).
Analysis of survey responses resulted in four main themes: 1) planning for children, 2) degree of baseline understanding of the effects anticancer therapy has on fertility and ovarian function, 3) resultant change in cognition after education about cancer treatment and its relationship to fertility, and 4) ascertaining the need for education regarding the types of therapy received and their effects on subsequent ovarian function and fertility.
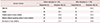
Before receiving video education about the impact of anticancer treatment on ovarian function and fertility, 92 young female breast cancer patients responded to the survey questionnaire which queried them to express their opinion about future plans for pregnancy. In total, 42.4% (n = 39) of participants reported a desire to have children in the future and 35.9% (n = 33) responded in the negative. A neutral attitude was taken by 21.7% (n = 20) of participants.
After viewing educational videos, likewise 109 young female breast cancer patients responded to the questions regarding a desire to have children in the future. Only 31.2% (n = 34) of participants reported a desire to have children in the future and 44.0% (n = 48) responded in the negative. A neutral attitude was taken by 24.8% (n = 27) of participants.
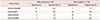
Prior to viewing educational videos, a total of 56.5% (52 out of 92) of patients answered that they had no knowledge of the impact of breast cancer therapy on ovarian function and fertility. But after viewing educational videos, only 1.8% (2 of 109) of patients responded that they had absolutely no knowledge of these effects.
Only 3.3% (n = 3) of uneducated patients answered that they had clear knowledge of the effect of breast cancer treatment on ovarian function and fertility. On the other hand, 22.0% (n = 24) of patients after education
by health professionals responded that they had good understanding of the impact of breast cancer treatment on ovarian function and fertility.
There are several ways to prevent ovarian function and reproductive deterioration that can occur with breast cancer therapy. The ways to ovarian function preservation are ovarian transposition (oophoropexy) and Gonadotropin-releasing hormone agonist before anticancer therapy. Embryo or oocyte of cryopreservation is a treatment for preserving fertility before anti-cancer therapy.
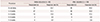
Before receiving education, 2.2% (2 of 92) of patients responded they absolutely did not wish to change anticancer therapy and 7.6% (n = 7) of patients did not; 45.6% (42 of 92) of patients responded that they would choose to change anticancer therapy and 16.3% (n = 15) of patients changes enough the therapy method for ovarian function.
After viewing educational videos, surveys by 109 young females with breast cancer reflected that 4.6% (n = 5) of patients responded that they absolutely would not choose to change the anticancer therapy and 16.5% (n = 18) of patients did not. 31.2% (n = 34) of patents responded that they would choose to change the anti-cancer therapy and 12.8% (n = 14) of patients changes enough the therapy method to preserve ovarian function.
Before receiving education, 92 participants expressed their opinion regarding the intention to change anti-cancer treatment in order to preserve fertility; 6.5% (n = 6) of patients chose that they did not want to change anticancer therapy absolutely; 12.0% (n = 11) of patients did not; 40.2% (n = 37) of patents chose that they could change anticancer therapy; and 16.3% (n = 15) of patients changes enough the therapy method for fertility.
One hundred nine young breast cancer women who got a video education express that 7.3% (n = 8) of patient choose that they do not change anticancer therapy absolutely and 22.0% (n = 24) of patient does not. On the other hand, 30.3% (n = 33) of patents choose that they can change anticancer therapy and 9.2% (n = 10) of patients changes enough the therapy method for fertility.
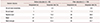
Before receiving education, 20.7% (19 of 92) of patients responded that that they would not wish to delay their breast cancer therapy to undergo a procedure which would preserve fertility. But after viewing educational videos, 44.0% (48 of 109) of patients responded that they would not delay treatment.
Before receiving education, 2.2% (2 of 92) of patients responded that they did not need education absolutely, 1.1% (1 of 92) of patients responded only that they did not. However, 81.5% (75 of 92) of patients responded that they did need education regarding therapeutic options to preserve ovarian function and fertility.
After viewing videos, 0.0% (n = 0) responded that they did not need education absolutely and 11.9% (13 of 109) of patients responded only that they did not. 61.5% (67 of 109) of patients responded that they did have a need for education regarding therapeutic options for preserving ovarian function and fertility.
Although these results do not adequately demonstrate the degree of satisfaction experienced when education is provided, it is inferred that young female breast cancer patients do not derive a great benefit and need from education and counseling with health professionals.
Concerns about ovarian function and fertility are key issues in young female breast cancer patients and have become more important over time as the numbers of breast cancer patients and survivors in that demographic increase.
In recent studies, the potential loss of ovarian function and fertility has been found to have a profound impact on young female cancer patients and in some ways may be more stressful than the cancer diagnosis itself [1617].
This study demonstrates that 36 persons of young breast cancer patient have not yet married and 39 participants have not completed their families out of 92 who have not had education. The 52 persons of young breast cancer patient have not yet married and 34 participants have not completed their families out of 109 who have had education. Most breast cancer treatments are gonadotoxic [18]. However, many young breast cancer patients are given little information or support around these issues.
This research aims to support the discussion between young breast cancer patients and health professionals about the impact of treatment on ovarian function and fertility prior to its initiation.
Before receiving education by health professionals, 56.5% of research participants did not have knowledge about the impact of breast cancer treatment on ovarian function and fertility. After viewing educational videos, only 1.8% of participants responded that they had no knowledge. Having knowledge and understanding of the impact of anticancer treatment on fertility is very important to many of the young breast cancer patients before planning to start multimodality treatment because they can then choose an appropriate course of therapy depending upon current life circumstances and plans for future children.
In addition to having a greater understanding of the effects of therapy, it certainly will help them to choose the most appropriate breast cancer treatment as well as the start time. Fertility preservation techniques require a period of the time to be accomplished, for example oocyte or embryo cryopreservation takes a couple of weeks from the beginning of the menstrual cycle, with the consequence that initiation of anticancer therapy can be delayed.
Before being educated, study participants who had no intention to change the therapeutic method to preserve ovarian function and fertility represented 9.8% and 18.5%. After viewing educational videos, participants who had no intention to change the therapeutic method in order to preserve ovarian function and fertility represented 21.1% and 29.3%. Participants' answers reflected their feeling that the importance of fertility concerns and preserving ovary function was secondary to survival. This result is meaningful that patients can understand the time, methods, and side effect required to performed anticancer treatment delay through education. In addition, the health professionals can actively consult the patient's opinions in the course of the treatment.
Also, the responses regarding the amount of time that patients would allow for the delaying of anticancer treatment in order to undergo a procedure to preserve fertility are different before and after receiving education. These changes reflect an attitude that may influence their treatment decisions.
A previous study showed that all participants answered that education was helpful and 73% made their decision about treatment after education [19].
In our study, none of participants who had video education responded that they did not need education absolutely. Only 2 participants who had not yet received training answered that they do not need education absolutely.
Though not considered in the interpretation of patient's satisfaction with and perceived helpfulness of information about cancer treatment related to the preservation of ovarian function, the majority of participants preferred as much information as possible. This result indicates that all patients with diagnosed breast cancer should receive an assessment and communication regarding risk of treatment related to ovarian function and fertility. This education should be given in association with a clinical expert with discussion of options for ovary and fertility preservation methods.
Most young female breast cancer patients are worried about their fertility, the impact of pregnancy on recurrence, and having a healthy future life. Therefore, patients should be directed to take a profound interest in their anticancer treatment. They should be given the opportunity to discuss with clinicians the various therapeutic methods and their impact on ovarian function. Our study indicates a need and opportunity to develop patient education material regarding the effects of treatment on fertility and help these young patients to make informed decisions about their future.
Figures and Tables
References
1. National Cancer Information Center. Incidence by cancer type. Il-san: National Cancer Information Center;cited 2016 Dec 27. Available from: https://www.cancer.go.kr/lay1/S1T639C641/contents.do.
2. National Cancer Information Center. 5-year relative cancer survival rate. Il-san: National Cancer Information Center;cited 2016 Dec 27. Available from: https://www.cancer.go.kr/lay1/S1T648C650/contents.do.
3. Merlo DF, Ceppi M, Filiberti R, Bocchini V, Znaor A, Gamulin M, et al. Breast cancer incidence trends in European women aged 20-39 years at diagnosis. Breast Cancer Res Treat. 2012; 134:363–370.
4. Anders CK, Johnson R, Litton J, Phillips M, Bleyer A. Breast cancer before age 40 years. Semin Oncol. 2009; 36:237–249.
5. Azim HA Jr, Partridge AH. Biology of breast cancer in young women. Breast Cancer Res. 2014; 16:427.
6. Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006; 24:2917–2931.
7. Hulvat MC, Jeruss JS. Maintaining fertility in young women with breast cancer. Curr Treat Options Oncol. 2009; 10:308–317.
8. Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013; 31:2500–2510.
9. Dizon DS, Suzin D, McIlvenna S. Sexual health as a survivorship issue for female cancer survivors. Oncologist. 2014; 19:202–210.
10. King L, Quinn GP, Vadaparampil ST, Gwede CK, Miree CA, Wilson C, et al. Oncology nurses' perceptions of barriers to discussion of fertility preservation with patients with cancer. Clin J Oncol Nurs. 2008; 12:467–476.
11. Quinn GP, Vadaparampil ST, King L, Miree CA, Wilson C, Raj O, et al. Impact of physicians' personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009; 77:338–343.
12. Ellis SJ, Wakefield CE, McLoone JK, Robertson EG, Cohn RJ. Fertility concerns among child and adolescent cancer survivors and their parents: a qualitative analysis. J Psychosoc Oncol. 2016; 34:347–362.
13. Zebrack BJ, Casillas J, Nohr L, Adams H, Zeltzer LK. Fertility issues for young adult survivors of childhood cancer. Psychooncology. 2004; 13:689–699.
14. Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009; 15:587–597.
15. Balthazar U, Fritz MA, Mersereau JE. Fertility preservation: a pilot study to assess previsit patient knowledge quantitatively. Fertil Steril. 2011; 95:1913–1916.
16. Schover LR. Patient attitudes toward fertility preservation. Pediatr Blood Cancer. 2009; 53:281–284.
17. Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004; 22:4174–4183.
18. Wallace WH, Smith AG, Kelsey TW, Edgar AE, Anderson RA. Fertility preservation for girls and young women with cancer: population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol. 2014; 15:1129–1136.
19. Kim J, Deal AM, Balthazar U, Kondapalli LA, Gracia C, Mersereau JE. Fertility preservation consultation for women with cancer: are we helping patients make high-quality decisions? Reprod Biomed Online. 2013; 27:96–103.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download