1. Al Kadri H, Hassan S, Al-Fozan HM, Hajeer A. Hormone therapy for endometriosis and surgical menopause. Cochrane Database Syst Rev. 2009; (1):CD005997. PMID:
19160262.

2. Niro J, Panel P. [Interest of hysterectomy with or without bilateral oophorectomy in the surgical treatment of endometriosis: CNGOF-HAS Endometriosis Guidelines]. Gynecol Obstet Fertil Senol. 2018; 46:314–318. PMID:
29530555.
3. Rotem M, Kushnir T, Levine R, Ehrenfeld M. A psycho-educational program for improving women's attitudes and coping with menopause symptoms. J Obstet Gynecol Neonatal Nurs. 2005; 34:233–240.

4. Marra AR, Puig-Asensio M, Edmond MB, Schweizer ML, Bender D. Infectious complications of laparoscopic and robotic hysterectomy: a systematic literature review and meta-analysis. Int J Gynecol Cancer. 2019; 29:518–530. PMID:
30833440.

5. Currie H. BMS Vision for menopause Care in the UK; is implementation achievable? Post Reprod Health. 2019; 25:5–6.

6. Tarvardi M, Shabani A. [Assessment of psychological problems in menopause women and relationship's between individual and social characteristic and menopausal symptoms in referred to tabriz educational hospitalS in 2005-2006]. J Urmia Nurs Midwifery Fac. 2007; 5:37–45.
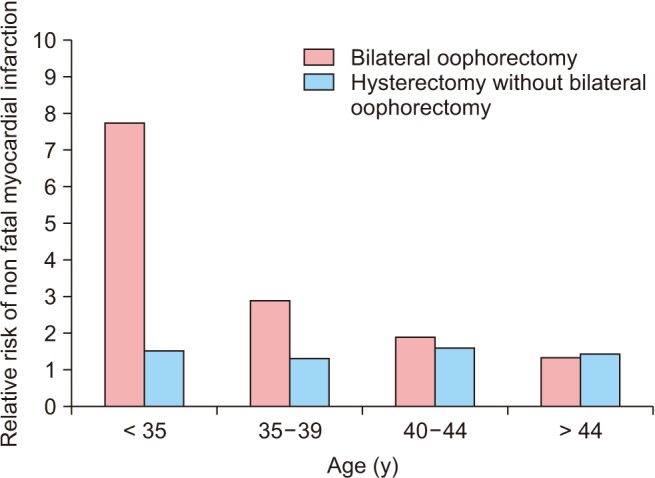
7. Erekson EA, Martin DK, Ratner ES. Oophorectomy: the debate between ovarian conservation and elective oophorectomy. Menopause. 2013; 20:110–114. PMID:
22929033.
8. Tsiligiannis S, Panay N, Stevenson JC. Premature ovarian insufficiency and long-term health consequences. Curr Vasc Pharmacol. 2019; 17:604–609. PMID:
30819073.

9. Lip GY, Blann AD, Jones AF, Beevers DG. Effects of hormonereplacement therapy on hemostatic factors, lipid factors, and endothelial function in women undergoing surgical menopause: implications for prevention of atherosclerosis. Am Heart J. 1997; 134:764–771. PMID:
9351746.

10. Simpson JS, Carlson LE, Trew ME. Effect of group therapy for breast cancer on healthcare utilization. Cancer Pract. 2001; 9:19–26. PMID:
11879269.

11. Li S, Ho SC, Sham A. Relationship between menopause status, attitude toward menopause, and quality of life in Chinese midlife women in Hong Kong. Menopause. 2016; 23:67–73. PMID:
26671191.

12. Elit L, Esplen MJ, Butler K, Narod S. Quality of life and psychosexual adjustment after prophylactic oophorectomy for a family history of ovarian cancer. Fam Cancer. 2001; 1:149–156. PMID:
14574171.
13. Hickey M, Trainer A, Braat S, Davey MA, Krejany E, Wark J. What Happens After Menopause? (WHAM): protocol for a prospective, multicentre, age-matched cohort trial of risk-reducing bilateral salpingo-oophorectomy in high-risk premenopausal women. BMJ Open. 2017; 7:e018758.

14. Kalkım A, Dağhan Ş. Theory-based osteoporosis prevention education and counseling program for women: a randomized controlled trial. Asian Nurs Res (Korean Soc Nurs Sci). 2017; 11:119–127. PMID:
28688497.

15. Sehhatie Shafaie F, Mirghafourvand M, Jafari M. Effect of education through support group on early symptoms of menopause: a randomized controlled trial. J Caring Sci. 2014; 3:247–256. PMID:
25709980.
16. Faraji K, Kamrani MA, Saeieh SE, Farid M. Could a midwife leading health behavior counseling improve self-care of women during perimenopause? A quasi-experimental study. J Midlife Health. 2018; 9:195–199. PMID:
30692815.
17. Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas. 2008; 61:107–121. PMID:
19434884.

18. Yazdkhasti M, Keshavarz M, Khoei EM, Hosseini A, Esmaeilzadeh S, Pebdani MA, et al. The effect of support group method on quality of life in post-menopausal women. Iran J Public Health. 2012; 41:78–84.
19. Nazarpour S, Simbar M, Ramezani Tehrani F, Alavi Majd H. Quality of life and sexual function in postmenopausal women. J Women Aging. 2018; 30:299–309. PMID:
29077541.

20. Direkvand-Moghadam A, Delpisheh A, Montazeri A, Sayehmiri K. Quality of life among Iranian infertile women in postmenopausal period: a cross-sectional study. J Menopausal Med. 2016; 22:108–113. PMID:
27617245.

21. Yazdkhasti M, Simbar M, Abdi F. Empowerment and coping strategies in menopause women: a review. Iran Red Crescent Med J. 2015; 17:e18944. PMID:
26019897.

22. Forouhari S, Safari Rad M, Moattari M, Mohit M, Ghaem H. [The effect of education on quality of life in menopausal women referring to Shiraz Motahhari clinic in 2004]. Birjand Univ Med Sci. 2009; 16:39–45.
23. Rostami A, Ghofrani Pour F, Ramezanzadeh F. The effect of education on quality of life in women [dissertation]. Tehran: Tarbiat Modares University;2001. 12:p. 25–29. [Persian].
24. Abdullah B, Moize B, Ismail BA, Zamri M, Mohd Nasir NF. Prevalence of menopausal symptoms, its effect to quality of life among Malaysian women and their treatment seeking behaviour. Med J Malaysia. 2017; 72:94–99. PMID:
28473671.
25. Yazdkhasti M, Keshavarz M, Khoei EM, Hosseini A, Esmaeilzadeh S, Pebdani MA, et al. The effect of support group method on quality of life in post-menopausal women. Iran J Public Health. 2012; 41:78–84.
26. Nosek M, Kennedy HP, Gudmundsdottir M. Distress during the menopause transition: a rich contextual analysis of midlife women's narratives. Sage Open. 2012; 2:2158–2440.
27. Bener A, Falah A. A measurement-specific quality-of-life satisfaction during premenopause, perimenopause and postmenopause in Arabian Qatari women. J Midlife Health. 2014; 5:126–134. PMID:
25316998.

28. Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015; 18:483–491. PMID:
25845383.

29. Karimy M, Aminshokravi F, Zareban E, Koohpayezadeh J, Baradaran H, Khoshdel A. [The effect of education based on individual empowerment model on the quality of life in the menopause women in Zarandieh]. Yafte. 2014; 16:80–90.
30. Kermode M, Herrman H, Arole R, White J, Premkumar R, Patel V. Empowerment of women and mental health promotion: a qualitative study in rural Maharashtra, India. BMC Public Health. 2007; 7:225. PMID:
17761003.

31. Khajavi D. Kanmohamadi R. The effect of “green exercise” on improving the sleep quality of female elderly without regular physical activity in Arak city. Journal of Woman and Family Studies. 2016; 3:7–32.
32. Camerini L, Schulz PJ, Nakamoto K. Differential effects of health knowledge and health empowerment over patients' self-management and health outcomes: a cross-sectional evaluation. Patient Educ Couns. 2012; 89:337–344. PMID:
22959333.

33. Parsa P, Ahmadinia Tabesh R, Soltani F, Karami M, Khorami N. Effects of group counseling on self-care behaviors in menopausal women with diabetes. J Menopausal Med. 2017; 23:108–116. PMID:
28951859.

34. Nappi RE, Martini E, Terreno E, Albani F, Santamaria V, Tonani S, et al. Management of hypoactive sexual desire disorder in women: current and emerging therapies. Int J Womens Health. 2010; 2:167–175. PMID:
21072309.

35. Meston CM, Frohlich PF. The neurobiology of sexual function. Arch Gen Psychiatry. 2000; 57:1012–1030. PMID:
11074867.

36. Nappi RE, Lello S, Melis GB, Albani F, Polatti F, Genazzani AR. LEI (Lack of tEstosterone Impact) survey in a clinical sample with surgical menopause. Climacteric. 2009; 12:533–540. PMID:
19905905.

37. Newton KM, Reed SD, LaCroix AZ, Grothaus LC, Ehrlich K, Guiltinan J. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy, or placebo: a randomized trial. Ann Intern Med. 2006; 145:869–879. PMID:
17179056.

38. Aloumanis K, Karras D, Drossinos V, Korelis E, Polydorakis A. Fracture incidence, quality of life, and back pain during 18-months treatment with teriparatide in Greek postmenopausal women with osteoporosis: results from the European forsteo observational study. J Osteoporos. 2011; 2011:510398. PMID:
21941680.

39. Babakhani N, Taravati M, Masoumi Z, Garousian M, Faradmal J, Shayan A. The effect of cognitive-behavioral consultation on sexual function among women: a randomized clinical trial. J Caring Sci. 2018; 7:83–88. PMID:
29977878.
40. Dhikav V, Karmarkar G, Gupta R, Verma M, Gupta R, Gupta S, et al. Yoga in female sexual functions. J Sex Med. 2010; 7(2 Pt 2):964–970. PMID:
19912493.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download