Abstract
An enlarged inferior turbinate is a predisposing factor for difficult nasotracheal intubation. We describe a case of successful nasotracheal intubation by induced outfracture of the inferior turbinate during maxillofacial surgery, and discuss the importance of adequate airway evaluation and anesthetic management for successful nasal intubation.
Nasotracheal intubation is commonly performed for maxillofacial surgery or dental procedures, to ensure visibility of the surgical field and ease of surgical manipulation [1]. However, passage of the tube through the nasal cavity can often lead to epistaxis. Intubation can be difficult due to various conditions such as septal deviation, enlarged turbinate, inflammation, or allergic hypertrophy [2].
Various methods such as thermo-softening of the tube, vasoconstrictor pretreatment, and guided intubation using a nasogastric tube, bougie, or fiberoptic bronchoscope have been used for effective nasotracheal intubation [345]. Inferior turbinate enlargement might be accompanied by mucosal or soft tissue hypertrophy, osseous hypertrophy of the bone itself or concha bullosa, a bullous change of the bone. Moreover, there might be structural variations such as medial transition of the turbinate and significant septal deviation.
Inferior turbinate outfracture is often performed alone or in combination with other treatments for severe nasal obstruction [6].
We report a case of successful nasotracheal intubation through an induced outfracture of the enlarged inferior turbinate, to prevent serious complications such as bleeding or obstruction.
A 49-year-old woman was hospitalized for planned dental surgery for a cystic lesion in the right maxilla. The patient had no nasal symptoms like nasal obstruction, rhinorrhea, or pain. Her height and weight were 155.5 cm and 49.9 kg, respectively. She was an active smoker, smoking one pack a day; there was no known coexisting disease. There were no specific findings on preoperative blood tests, chest radiograph, or electrocardiograms. She was not on any anticoagulants. The preoperative dental computed tomography (CT) scan showed a radicular cyst at the right maxilla and a mucocele at the left maxilla, with septal deviation and inferior turbinate hypertrophy (Fig. 1).
The anesthesiologist had planned nasotracheal intubation for the surgery. On the day of surgery, the patient's blood pressure was 118/67 mmHg, pulse was 78 /min, and oxygen saturation was 98%. During the anesthetic procedure, a 5% lidocaine spray was applied to both sides of the nose, and epinephrine-soaked cotton swabs were placed 5–7 cm deep into the nasal cavity for 5 minutes. A reinforced cuffed endotracheal tube of 6.5 mm internal diameter was selected for nasotracheal intubation and lubricated adequately with lidocaine jelly. After preoxygenation, propofol 120 mg, lidocaine 60 mg, and fentanyl 50 µg were administered intravenously. Following loss of consciousness, rocuronium 50 mg was administered and mask ventilation was performed with oxygen and desflurane 7%. After confirmation of full relaxation, nasotracheal intubation was attempted. The left nostril was chosen based on preoperative CT scan findings, and the endotracheal tube was carefully inserted into the nostril under fiberoptic bronchoscope guidance.
The nasal cavity of the patient was almost obstructed by a hard and enlarged inferior turbinate. The lubricated fiberoptic bronchoscope could be passed through the cavity; however, the reinforced tube could not be inserted. The size of the tube was serially reduced up to an internal diameter of 5.5 mm; however, the insertion failed. The patient developed epistaxis and despite continuous nasal suction, the bronchoscopic field remained unclear. The right nasal approach was attempted; however, once again only the fiberoptic bronchoscope could be inserted but not the endotracheal tube.
To prevent further mucosal edema or epistaxis, it was decided to perform outfracture and lateralization of the inferior turbinate. The malar elevator entered the nasal cavity and pushed the medially protruded enlarged inferior turbinate (= concha) upward and laterally until a greenstick fracture occurred. The crunching sound of the fracture was audible and the process was repeated several times to create more space. Nasotracheal intubation with size 6.0 cuffed endotracheal tube was attempted and the tube passed easily through the enlarged nasal cavity. There was no further bleeding or other complications. After fixing the nasotracheal tube to the desired depth, surgery was initiated. To prevent excessive edema in the nasal cavity, intravenous dexamethasone 5 mg was administered.
During surgery, the vital signs were stable and there was no significant bleeding. The maxillary radicular cyst was enucleated. The surgical time was 45 minutes. Muscle relaxation was completely reversed by intravenous sugammadex 200 mg and carefully extubated after the patient was awakened. There was no significant nasal bleeding or airway obstruction. After the patient regained consciousness, breathing through the mouth was advised, because her nose was packed with gauze. During the stay in post-anesthetic care unit, there was no hypoxic event or apnea. There was no pain or other complaints.
In the ward, the patient was positioned with head end of the bed elevated at approximately 30 degrees. An ice pack was applied to the surgical site and frequent gargling with normal saline was advised to prevent crust formation. A single dose of analgesic medication was administered. There was no further bleeding or nasal symptoms. On the day after surgery, the patient was discharged without any complications.
On her visit to the outpatient clinic one week later, she had no specific complications and appeared to recover well.
This was a case of successful nasotracheal intubation with induced outfracture of the inferior turbinate in a patient undergoing maxillofacial surgery.
There are two pathways for intubation through the nasal cavity: a lower pathway entering the nasal floor below the inferior turbinate and an upper pathway entering between the inferior and middle turbinate. The lower pathway is generally preferred because the upper pathway causes more epistaxis and complications such as cribriform plate damage and skull base fracture [7].
Nasal obstruction is present in approximately 25% of the population, and is accompanied by various morbidities.[89]. The causes of obstruction include nasal septal deviation, inferior and medial turbinate hypertrophy, nasal polyps, or pharyngeal tonsil hypertrophy. Of these, the most common cause is inferior turbinate hypertrophy. Compensatory hypertrophy of the inferior turbinate often occurs in patients with septal deviation [8].
Inferior turbinate enlargement might be due to mucosal hypertrophy, osseous hypertrophy, or concha bullosa, which is a bullous change in the bone that might cause unpredictable severe epistaxis or mucosal injury [29]. Tong et al [10] also reported that nasal pathologies such as inferior turbinate hypertrophy and septal deviation were found in 51% of asymptomatic patients during baseline rhinoscopic evaluation.
Our patient had mild septal deviation and chronic inflammation due to heavy smoking. The inferior turbinate was medially protruded and significantly enlarged, with mucosal hypertrophy. There was no osseous abnormality. However, only the fiberoptic bronchoscope could be inserted but not the endotracheal tube. Moreover, a conventional endotracheal tube with small diameter could not be used because its length could not reach the trachea.
Nasotracheal intubation was attempted under fiberoptic bronchoscopic guidance using a lubricated reinforced tube, and epinephrine soaked swab with topical local anesthetics; however, the attempt was unsuccessful. Repetitive forceful attempts to intubate could lead to further complications such as excessive edema or significant bleeding. A catastrophic tube obstruction due to accidental turbinectomy after multiple intubation attempts has been reported [11]. Hence, instead of multiple repeated attempts, an alternative method to expand the space in the nasal cavity was necessary.
Various options to reduce the size of the hypertrophied turbinate range from conservative methods such as laser vaporization and electrocautery, to surgical treatments such as partial turbinectomy and submucosal turbinoplasty [12]. However, during an acute event such as nasotracheal intubation, few options can be exercised. In such situations, the focus is on minimizing mucosal destruction to reduce adverse events such as pain, crust formation, and olfactory dysfunction while reducing the size of the turbinate.
Inferior turbinate outfracture is a method of lateralization of the concha that extends medially. It can be performed alone or in combination with another procedure. It is easy to perform, preserves the nasal epithelium and does not interfere with mucociliary movement; hence, it does not cause significant crusting, infection, bacteremia, or necrosis [13]. No universal method of performing the outfracture has yet been established. The traditional method of first infracture breaks the inferior turbinate into the septum with an upward and inward direction, and then outfractures again laterally. The other method is only outfracture by just pushing the turbinate laterally. The difference in safety between the two methods has not yet been demonstrated. In our case, we performed outfracture of the inferior turbinate, after which nasotracheal intubation was successful at the first attempt, and there was no bleeding or adverse effects after extubation.
There are few studies on the prognosis of outfracture of the inferior turbinate. It is possible that, the outfracture is not sustainable for a long duration and the lateralized inferior turbinate tends to return to its original position. However, several studies have reported that the effect of outfracture persisted for at least 6 months without serious chronic complications [6].
In conclusion, outfracture of the inferior turbinate might be a simple and safe method for widening the nasal cavity in patients with failed nasotracheal intubation due to bony and / or mucosal hypertrophy of inferior turbinate.
Figures and Tables
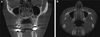 | Fig. 1Preoperative dental computed tomography showing a radicular cyst in the right maxilla and a mucocele in the left maxilla. The nasal septum appears mildly deviated and the inferior turbinate is enlarged with mucosal hypertrophy. Osseous hypertrophy or concha bullosa is not found (A; coronal view, B; axial view). |
Notes
References
1. Hall CE, Shutt LE. Nasotracheal intubation for head and neck surgery. Anaesthesia. 2003; 58:249–256.

2. Orhan I, Aydin S, Ormeci T, Yilmaz F. A radiological analysis of inferior turbinate in patients with deviated nasal septum by using computed tomography. Am J Rhinol Allergy. 2014; 28:e68–e72.

3. Lim CW, Min SW, Kim CS, Chang JE, Park JE, Hwang JY. The use of a nasogastric tube to facilitate nasotracheal intubation: a randomised controlled trial. Anaesthesia. 2014; 69:591–597.

4. Kwon MA, Song J, Kim S, Ji SM, Bae J. Inspection of the nasopharynx prior to fiberoptic-guided nasotracheal intubation reduces the risk epistaxis. J Clin Anesth. 2016; 32:7–11.

5. Seo KS, Kim JH, Yang SM, Kim HJ, Bahk JH, Yum KW. A new technique to reduce epistaxis and enhance navigability during nasotracheal intubation. Anesth Analg. 2007; 105:1420–1424.

6. Lee DC, Jin SG, Kim BY, Yoo S, Han S, Lee YJ, et al. Does the effect of inferior turbinate outfracture persist? Plast Reconstr Surg. 2017; 139:386e–391e.

7. Ahmed-Nusrath A, Tong JL, Smith JE. Pathways through the nose for nasal intubation: a comparison of three endotracheal tubes. Br J Anaesth. 2008; 100:269–274.

8. Berger G, Hammel I, Berger R, Avraham S, Ophir D. Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. Laryngoscope. 2000; 110:2100–2105.

9. Min HJ, Min SK, Hong YH, Kim KS. The potential significance of concha bullosa during nasotracheal intubation. J Craniofac Surg. 2016; 27:e153–e154.

10. Tong JL, Tung A. A randomized trial comparing the effect of fiberoptic selection and guidance versus random selection, blind Insertion, and direct laryngo scopy, on the incidence and severity of epistaxis after nasotracheal intubation. Anesth Analg. 2018; 127:485–489.

11. Cavusoglu T, Yazici I, Demirtas Y, Gunaydin B, Yavuzer R. A rare complication of nasotracheal intubation: accidental middle turbinectomy. J Craniofac Surg. 2009; 20:566–568.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download