1. Damlar İ, Altan A, Tatlı U, Arpağ OF. Retrospective Investigation of the Prevalence of Impacted Teeth in Hatay. Cukurova Med J. 2014; 39:559–565.
2. Polat HB, Ozan F, Kara I, Ozdemir H, Ay S. Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105:e41–e47.

3. Bataineh AB, Albashaireh ZS, Hazza'a AM. The surgical removal of mandibular third molars: a study in decision making. Quintessence Int. 2002; 33:613–617. PMID:
12238694.
4. Fuster Torres MA, Gargallo Albiol J, Berini Aytes L, Gay Escoda C. Evaluation of the indication for surgical extraction of third molars according to the oral surgeon and the primary care dentist. Experience in the Master of Oral Surgery and Implantology at Barcelona University Dental School. Med Oral Patol Oral Cir Bucal. 2008; 13:E499–E504. PMID:
18667984.
5. McGrath C, Comfort MB, Lo EC, Luo Y. Changes in life quality following third molar surgery--the immediate postoperative period. Br Dent J. 2003; 194:265–268. PMID:
12658303.
6. Shafer DM, Frank ME, Gent JF, Fischer ME. Gustatory function after third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:419–428. PMID:
10225623.

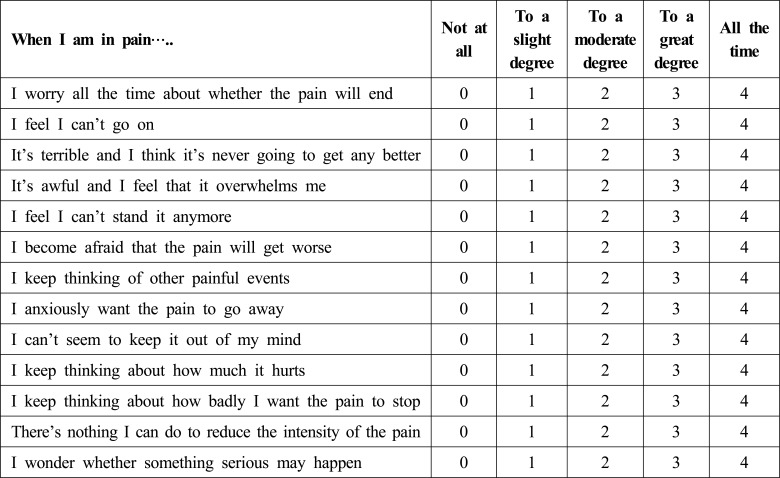
7. Sullivan MJ, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995; 7:524–532.

8. Sullivan MJ, Martel MO, Tripp D, Savard A, Crombez G. The relation between catastrophizing and the communication of pain experience. Pain. 2006; 122:282–288. PMID:
16545907.

9. Martin MY, Bradley LA, Alexander RW, Alarcón GS, Triana-Alexander M, Aaron LA, et al. Coping strategies predict disability in patients with primary fibromyalgia. Pain. 1996; 68:45–53. PMID:
9251997.

10. Jacobsen PB, Butler RW. Relation of cognitive coping and catastrophizing to acute pain and analgesic use following breast cancer surgery. J Behav Med. 1996; 19:17–29. PMID:
8932659.

11. Gil KM, Thompson RJ Jr, Keith BR, Tota-Faucette M, Noll S, Kinney TR. Sickle cell disease pain in children and adolescents: change in pain frequency and coping strategies over time. J Pediatr Psychol. 1993; 18:621–637. PMID:
8295083.

12. Koerner KR. The removal of impacted third molars. Principles and procedures. Dent Clin North Am. 1994; 38:255–278. PMID:
8206177.
13. Suren M, Kaya Z, Gokbakan M, Okan I, Arici S, Karaman S, et al. The role of pain catastrophizing score in the prediction of venipuncture pain severity. Pain Pract. 2014; 14:245–251. PMID:
23586760.

14. Gaudry E, Vagg P, Spielberger CD. Validation of the State-Trait distinction in anxiety research. Multivariate Behav Res. 1975; 10:331–341. PMID:
26829634.

15. Brasileiro BF, de Braganca RM, Van Sickels JE. An evaluation of patients' knowledge about perioperative information for third molar removal. J Oral Maxillofac Surg. 2012; 70:12–18. PMID:
21940090.

16. Muglali M, Komerik N. Factors related to patients' anxiety before and after oral surgery. J Oral Maxillofac Surg. 2008; 66:870–877. PMID:
18423273.

17. Kazancioglu HO, Dahhan AS, Acar AH. How could multimedia information about dental implant surgery effects patients' anxiety level? Med Oral Patol Oral Cir Bucal. 2017; 22:e102–e107. PMID:
27918733.

18. Ruscheweyh R, Nees F, Marziniak M, Evers S, Flor H, Knecht S. Pain catastrophizing and pain-related emotions: influence of age and type of pain. Clin J Pain. 2011; 27:578–586. PMID:
21368662.
19. Borsbo B, Peolsson M, Gerdle B. Catastrophizing, depression, and pain: correlation with and influence on quality of life and health - a study of chronic whiplash-associated disorders. J Rehabil Med. 2008; 40:562–569. PMID:
18758674.

20. Drahovzal DN, Stewart SH, Sullivan MJ. Tendency to catastrophize somatic sensations: pain catastrophizing and anxiety sensitivity in predicting headache. Cogn Behav Ther. 2006; 35:226–235. PMID:
17189240.

21. Edwards RR, Smith MT, Kudel I, Haythornthwaite J. Pain-related catastrophizing as a risk factor for suicidal ideation in chronic pain. Pain. 2006; 126:272–279. PMID:
16926068.

22. Chaves JF, Brown JM. Spontaneous cognitive strategies for the control of clinical pain and stress. J Behav Med. 1987; 10:263–276. PMID:
3612783.

23. Leventhal H, Brown D, Shacham S, Engquist G. Effects of preparatory information about sensations, threat of pain, and attention on cold pressor distress. J Pers Soc Psychol. 1979; 37:688–714. PMID:
448634.

24. Granot M, Ferber SG. The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain. 2005; 21:439–445. PMID:
16093750.
25. Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. 1986; 24:331–342. PMID:
3960574.

26. Diniz-Freitas M, Lago-Mendez L, Gude-Sampedro F, Somoza-Martin JM, Gandara-Rey JM, Garcia-Garcia A. Pederson scale fails to predict how difficult it will be to extract lower third molars. Br J Oral Maxillofac Surg. 2007; 45:23–26. PMID:
16434132.

27. Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003; 104:639–646. PMID:
12927636.

28. Reid GJ, Lang BA, McGrath PJ. Primary juvenile fibromyalgia. Psychological adjustment, family functioning, coping, and functional disability. Arthritis Rheum. 1997; 40:752–760. PMID:
9125260.

29. Kröner-Herwig B, Maas J. The German Pain Catastrophizing Scale for Children (PCS-C)–psychometric analysis and evaluation of the construct. Psychosoc Med. 2013; 10:doi.
30. Süren M, Okan I, Gökbakan AM, Kaya Z, Erkorkmaz U, Arici S, et al. Factors associated with the pain catastrophizing scale and validation in a sample of the Turkish population. Turk J Med Sci. 2014; 44:104–108. PMID:
25558568.

31. Ruscheweyh R, Nees F, Marziniak M, Evers S, Flor H, Knecht S. Pain catastrophizing and pain-related emotions: influence of age and type of pain. Clin J Pain. 2011; 27:578–586. PMID:
21368662.
32. Yuasa H, Kawai T, Sugiura M. Classification of surgical difficulty in extracting impacted third molars. Br J Oral Maxillofac Surg. 2002; 40:26–31. PMID:
11883966.

33. Renton T, Smeeton N, McGurk M. Factors predictive of difficulty of mandibular third molar surgery. Br Dent J. 2001; 190:607–610. PMID:
11441899.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download