INTRODUCTION
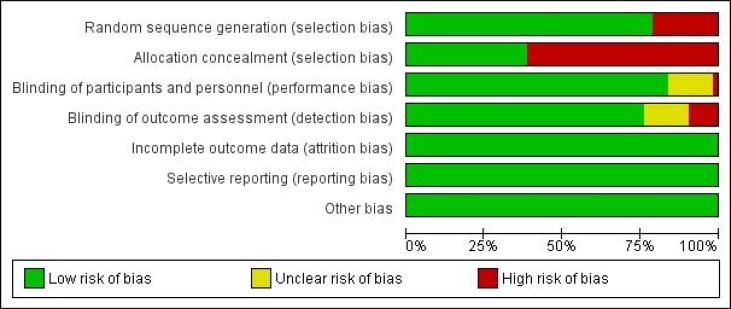
METHODS
1. Information sources and search strategy
2. Eligibility criteria
3. Study procedure and statistical considerations
RESULTS
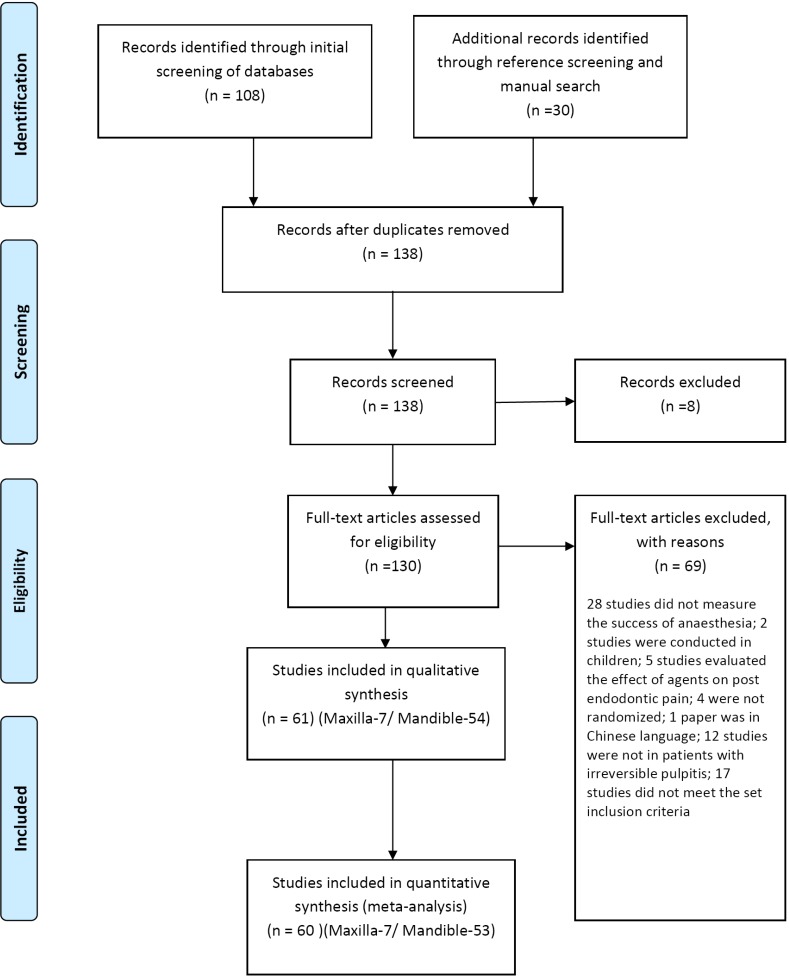
1. Search results
Table 1
Key characteristics of included studies
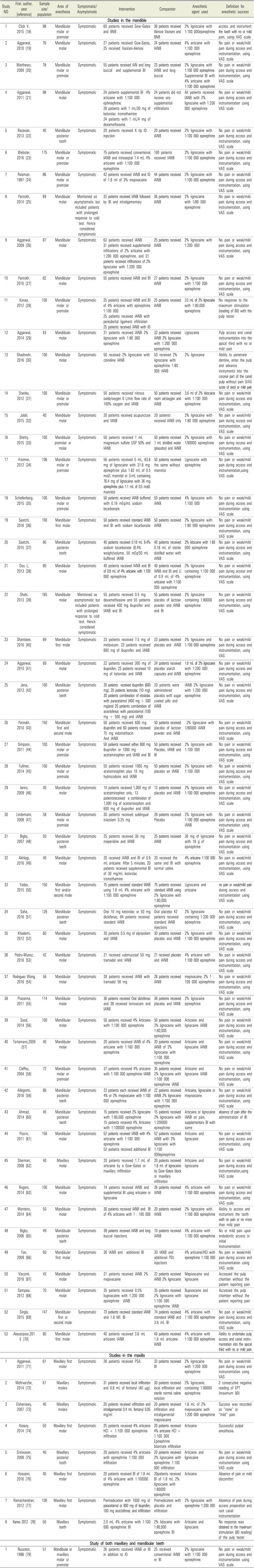
| Study NO | First author, year [reference] | Sample size/population | Area of anesthesia | Symptomatic/Asymptomatic | Intervention | Comparator | Anesthetic agent used | Definition for anesthetic success |
|---|---|---|---|---|---|---|---|---|
| Studies in the mandible | ||||||||
| 1 | Click V, 2015 [18] | 98 | Mandibular molar or premolar | Symptomatic | 60 patients received Gow–Gates and BNB | 38 patients received Akinosi Vazirani and BNB | 2% lignocaine with 1:100 000epinephrine | access and instrument the tooth with no or mild pain, using VAS scale |
| 2 | Aggarwal, 2010 [19] | 76 | Mandibular molar | Symptomatic | 27 patients received Gow-Gates, 25 received Vazirani-Akinosi | 24 patients received IANB | 4% articaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using |
| 3 | Matthews, 2009 [20] | 78 | Mandibular molar or premolar | Symptomatic | 55 patients received IAN and long buccal and supplemental BI | 23 patients received IANB and long buccal | 2% lignocaine with 1:100 000 epinephrine. | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| Supplemental BI with 4% articaine with 1:100 000 epinephrine | ||||||||
| 4 | Aggarwal, 2011 [21] | 98 | Mandibular molar | Symptomatic | 24 patients supplemental BI 4% articaine with 1:100 000 ephinephrine. | 24 patients did not receive any supplemental infiltrations | All patients received IANB with 2% lignocaine with 1:200 000 epinephrine | No pain or weak/mild pain during access and instrumentation using VAS scale |
| 26 patients with 1 mL/30 mg of ketorolac tromethamine | ||||||||
| 24 patients with 1 mL/4 mg of dexamethasone. | ||||||||
| 5 | Razavian, 2013 [22] | 40 | Mandibular posterior tooth | Symptomatic | 20 patients received X tip IO injection | 20 patients received IANB | 2% lignocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 6 | Webster, 2016 [23] | 175 | Mandibular molar or premolar | Symptomatic | 75 patients received conventional IANB and intraseptal 1.4 mL 4% articaine with 1:100 000 epinephrine | 100 patients received IANB | 2% lignocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 7 | Reisman, 1997 [24] | 86 | Mandibular molar or premolar | Symptomatic | 42 patients received IANB and IO of 1.8 ml of 3% mepivacaine | 44 patients received IANB | 2% lignocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 8 | Parirokh, 2014 [25] | 69 | Mandibular molar | Mentioned as asymptomatic but included patients with prolonged response to cold test. Hence considered symptomatic | 33 patients received IANB followed by BI and intraligamentary | 36 patients received IANB | 2% lignocaine with 1/80 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 9 | Aggarwal, 2009 [26] | 87 | Mandibular molar | Symptomatic | 62 patients received IANB. | 25 patients received | 2% lignocaine with | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 31 patients received supplemental infiltrations of 2% articaine with 1:200 000 epinephrine, and 31 patients received infiltrations of 2% lignocaine with 1:200 000 epinephrine | IANB | 1:200 000 | ||||||
| 10 | Parirokh, 2010 [27] | 82 | Mandibular molar | Symptomatic | 55 patients received IANB and BI | 27 patients received IANB | 2% lignocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 11 | Kanaa, 2012 [28] | 100 | Mandibular molar or premolar | Symptomatic | 25 patients received IANB and BI of 4% articaine with epinephrine 1:100 000 | 25 patients received IANB | 2.0 mL of 2% lignocaine with 1:80,000 epinephrine | No response to the maximum stimulation (reading of 80) with the pulp tester |
| 25 patients received IANB with periodontal ligament infiltration | ||||||||
| 25 patients received IANB with IO | ||||||||
| 12 | Aggarwal, 2014 [29] | 63 | Mandibular molar | Symptomatic | 31 patients received IANB 2% lignocaine with 1:80 000 epinephrine | 32 patients received IANB 2% lignocaine with 1:200 000 epinephrine | Lignocaine | Pulp access and canal instrumentation into the apical third with no or mild pain |
| 13 | Shadmehr, 2016 [30] | 100 | Mandibular molar | Symptomatic | 50 received 2% lignocaine with clonidine IANB | 50 received 2% lignocaine with epinephrine 1:80 000 IANB | 2% lignocaine | Ability to penetrate dentine, enter the pulp and advance instruments into the coronal part of the canal pulp without pain (VAS score of zero) or mild pain |
| 14 | Stanley, 2012 [31] | 100 | Mandibular molar or premolar | Symptomatic | 50 patients received nitrous oxide/oxygen 6 L/min flow rate of 100% oxygen and IANB | 50 patients received room air/oxygen and IANB | 3.6 ml of 2% lidocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 15 | Jalali, 2015 [32] | 40 | Mandibular molar | Symptomatic | 20 patients received acupuncture and IANB | 20 patients received IANB only | 2% lignocaine with 1:80 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 16 | Shetty, 2015 [33] | 100 | Mandibular premolar or molar | Symptomatic | 50 patients received 1 mL magnesium sulfate USP 50% and IANB | 50 patients received 1 mL distilled water (placebo) and IANB | 2% lignocaine with 1/80000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 17 | Kreimer, 2012 [34] | 106 | Mandibular molar or premolar | Symptomatic | 56 patients received 5 mL, 63.6 mg of lignocaine with 31.8 mg epinephrine plus 1.82 mL of 0.5 mol/L mannitol or 3-mL containing 76.4 mg of lignocaine with 36 mg epinephrine plus 1.1 mL of 0.5 mol/L mannitol | 50 patients received the same without mannitol | Lignocaine with epinephrine | No pain or weak/mild pain during access and instrumentation,using VAS scale |
| 18 | Schellenberg, 2015 [35] | 100 | Mandibular molar or premolar | Symptomatic | 50 patients received IANB buffered with 0.18 mEq/mL sodium bicarbonate | 50 patients received IANB | 4% lignocaine with 1:100 000 | No pain or weak/mild pain during access and instrumentation using VAS scale |
| 19 | Saatchi, 2016 [36] | 100 | Mandibular first molar | Symptomatic | 50 patients received standard IANB and BI with sodium bicarbonate | 50 patients received IANB | 2% lignocaine with 1:80 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 20 | Saatchi, 2015 [37] | 80 | Mandibular posterior tooth | Symptomatic | 40 patients received 0.18 mL 8.4% sodium bicarbonate (8.4% weight/volume, 50 mEq/50 mL buffered IANB | 40 patients received 0.18 mL of sterile distilled water with IANB | 2% lidocaine with 1:80 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 21 | Dou L, 2013 [38] | 80 | Mandibular molar | Symptomatic | 40 patients received IANB and BI of 0.9 mL of 4% articaine with 1:100 000 epinephrine | 40 patients received IANB and BI and LI of 0.9 mL of 4% articaine with 1:100 000 epinephrine | 2% lignocaine containing 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 22 | Shahi, 2013 [39] | 165 | Mandibular molar | Mentioned as asymptomatic but included patients with prolonged response to cold test. Hence considered symptomatic | 55 patients received 0.5 mg dexamethasone and 55 patients received 400 mg ibuprofen and IANB and BI | 55 patients received placebo of lactose powder and IANB and BI | 2% lignocaine containing 1:80000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 23 | Shantiaee, 2016 [40] | 69 | Mandibular first molar | Symptomatic | 23 patients received 7.5 mg of meloxicam; 23 patients received 600 mg of ibuprofen and IANB | 23 patients received placebo and IANB | 2% lignocaine and 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS |
| 24 | Aggarwal, 2010 [41] | 69 | Mandibular molar | Symptomatic | 22 patients received 300 mg of ibuprofen, 23 patients received 10 mg of ketorolac and IANB | 24 patients received placebo starch capsules and IANB | 1.8 mL of 2% lignocaine with 1:200 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 25 | Jena, 2013 [42] | 100 | Mandibular posterior teeth | Symptomatic | 20 patients received ibuprofen (600 mg), 20 patients ketorolac (10 mg), 20 patients combination of etodolac with paracetamol (400 mg + 500 mg)and 20 patients combination of aceclofenac with paracetamol (100 mg + 500 mg) and IANB | 20 patients were administered placebo with sugar coated pills and IANB | IANB 2% lignocaine with 1:200 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 26 | Parirokh, 2010 [43] | 150 | Mandibular first and second molar | Symptomatic | 50 patients received 600 mg ibuprofen and 60 patients received 75 mg indomethacin And IANB | 50 patients received placebo of lactose powder and IANB | 2% lignocaine with 1/80000 IANB | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 27 | Simpson, 2011 [44] | 100 | Mandibular molar or premolar | Symptomatic | 50 patients received either 800 mg ibuprofen or 1000 mg acetaminophen and IANB and BI | 50 patients received Placebo, IANB and BI | 2% lignocaine with 1:100 000 | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 28 | Fullmer, 2014 [45] | 100 | Mandibular molar or premolar | Symptomatic | 50 patients received 1000 mg acetaminophen plus 10 mg hydrocodone and IANB | 50 patients received placebo an IANB | 2% lignocaine with 1:100 000 | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 29 | Ianiro, 2009 [46] | 40 | Mandibular molar | Symptomatic | 14 patients received 1,000 mg of acetaminophen only, 13 patientsreceived a combination of 1,000 mg of acetaminophen and 600 mg of ibuprofen and IANB | 13 patients received placebo and IANB | 2% lignocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 30 | Lindemann, 2008 [47] | 58 | Mandibular molar or premolar | Symptomatic | 30 patients received sublingual triazolam 0.25 mg | 28 patients received Placebo | 2% lignocaine with 1:100 000 epinephrine IANB | No pain or weak/mild pain during access and instrumentation using VAS scale |
| 31 | Bigby, 2007 [48] | 50 | Mandibular posterior teeth | Symptomatic | 25 patients received 36 mg meperidine and IANB | 25 patients received IANB | 36 mg of lignocaine with 18 g of epinephrine | No pain or weak/mild pain during access and instrumentation using VAS scale |
| 32 | Akhlagi, 2016 [49] | 40 | Mandibular molar | Symptomatic | 20 received IANB and BI of 0.9 mL articaine. After 5 minutes, 20 patients received supplemental BI of 30 mg/mL ketorolac tromethamine | 20 received the same and BI with normal saline | 4% articaine 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 33 | Yadav, 2015 [50] | 150 | Mandibular first and/or second molar | Symptomatic | 75 patients received standard IANB using 1.8 mL 4% articaine with 1:100 000 epinephrine | 75 patients received standard IANB using 2% lignocaine with 1:80,000 epinephrine | Lignocaine and articaine | no pain or weak/mild pain during access and instrumentation using VAS scale |
| 34 | Saha, 2016 [51] | 126 | Mandibular posterior teeth | Symptomatic | Oral 10 mg ketorolac or 50 mg diclofenac, 84 patients received standard IANB | Oral placebo 42 patients received standard IANB injections | 2% lignocaine containing 1:200 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 35 | Khademi, 2012 [52] | 60 | Mandibular molar | Symptomatic | 30 patients 0.5 mg of alprazolam and IANB | 30 patients received placebo and IANB | 2% lignocaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 36 | Pedro-Munoz, 2016 [53] | 42 | Mandibular molar | Symptomatic | 21 received submucosal 50 mg tramadol and IANB | 21 received placebo and IANB | 4% articaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 37 | Rodrıguez Wong, 2016 [54] | 56 | Mandibular molar | Symptomatic | 28 patients received IANB with tramadol 50 mg | 28 patients received IANB | mepivacaine 2% 1 : 100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 38 | Prasanna, 2011 [55] | 114 | Mandibular molar | Symptomatic | 38 patients received Oral diclofenac and 38 received lornoxicam and IANB | 38 patients received placebo and IANB | 2% lignocaine epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 39 | Sood, 2014 [56] | 100 | Mandibular molar | Symptomatic | 50 patients received 4% Articaine with 1:100 000 epinephrine | 50 patients received 2% lignocaine with 1:80,000 epinephrine | Articaine and lignocaine IANB | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 40 | Tortamano,2009 [57] | 40 | Mandibular molar | Symptomatic | 20 patients received IANB of 4% articaine with 1:100 000 epinephrine | 20 patients received IANB of 2% lignocaine with 1:100 000 epinephrine | Articaine and lignocaine IANB | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 41 | Claffey, 2004 [58] | 72 | Mandibular molar or premolar | Symptomatic | 37 patients received 4% articaine with 1:100 000 epinephrine IANB | 35 patients received 2% lignocaine with 1:100 000 epinephrine IANB | Articaine and lignocaine IANB | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 42 | Allegretti, 2016 [59] | 66 | Mandibular posterior teeth | Symptomatic | 22 patients each received IANB of 4% or 2% mepivacaine with 1:100 000 epinephrine | 22 patients received IANB 2% lignocaine with 1:100 000 epinephrine | Articaine, lignocaine or mepivacaine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 43 | Ahmad, 2014 [60] | 45 | Mandibular posterior teeth | Symptomatic | 15 patients received 2% lignocaine with 1:80,000 epinephrine | 15 patients received 2% lignocaine with 1:200000 epinephrine | Articaine or lignocaine IANB on pain, supplementary BI with same | absence of pain after the administration of BI |
| 15 patients received 4% Articaine with 1:100000 epinephrine | ||||||||
| 44 | Poorni, 2011 [61] | 156 | Mandibular molar | Symptomatic | 52 patients received IANB with 4% articaine with 1:100 000 epinephrine | 52 patients received IANB with 2% lignocaine with 1:100 000epinephrine | Articaine and lignocaine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 52 patients received additional BI | ||||||||
| 45 | Sherman, 2008 [62] | 40 | Maxillary molar | Symptomatic | 20 patients received 1.7 mL of articaine by a Gow–Gates or maxillary infiltration | 20 patients received 1.8 mL of lignocaine by Gow–Gates block or maxillary infiltration | Articaine and lignocaine | No pain or weak/mild pain during access and instrumentation,using VAS scale |
| 46 | Rogers, 2014 [63] | 100 | Mandibular molar | Symptomatic | 74 patients received IANB and supplemental BI using articaine or lignocaine | 26 patients received IANB | 4% articaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 47 | Monteiro, 2014 [64] | 50 | Mandibular molar | Symptomatic | 30 patients received IANB and BI of 4% articaine with 1 : 100 000 | 20 patients received IANB. | 2% lignocaine with 1:100 000 epinephrine | Ability to access and instrument the tooth with no pain or no more than mild pain |
| 48 | Bigby, 2006 [65] | 49 | Mandibular posterior teeth | Symptomatic | 39 patients received IANB and long buccal injections | 10 patients received IANB | 4% articaine with 1:100 000 epinephrine | No or mild pain upon endodontic access or initial Instrumentation |
| 49 | Fan, 2009 [66] | 60 | Mandibular first molar | Symptomatic | 30 IANB and additional BI | 30 IANB and additional PDL injections | 4% articaine/HCl with epinephrine 1:100 000 | No pain or weak/mild pain during access and instrumentation using VAS scale |
| 50 | Visconti, 2016 [67] | 43 | Mandibular molar | Symptomatic | 21 patients received IANB 2% mepivacaine | 22 patients received IANB 2% lignocaine | Mepivacaine and lignocaine | Accessed the pulp chamber without the patient reporting pain |
| 51 | Sampaio, 2012 [68] | 70 | Mandibular molar | Symptomatic | 35 patients received 0.5% bupivacaine with 1:200 000 epinephrine IANB | 35 patients received 2% lignocaine with 1:100 000 epinephrine IANB | Bupivacaine and lignocaine | Accessed the pulp chamber without the patient reporting pain |
| 52 | Singla, 2015 [69] | 147 | Mandibular first or second molar | Symptomatic | 73 patients received standard IANB and 1.8 ML BI | 74 patients received standard IANB and 3.6 mL BI | 4% articaine with 1:100 000 epinephrine | No pain or weak/mild pain during access and instrumentation, using VAS scale |
| 53 | Abazarpoor,201 5 [70] | 80 | Mandibular first molar | Symptomatic | 40 patients received 3.6 mL articaine IANB | 40 patients received 1.8 mL articaine IANB | 4% articaine with 1:100 000 epinephrine | Ability to undertake pulp access and canal instrumentation into the apical third with no or mild pain |
| Studies in the maxilla | ||||||||
| 1 | Aggarwal, 2011 [71] | 61 | Maxillary first molar | Symptomatic | 28 patients received PSA | 33 patients received BI | 2% lignocaine with 1:200 000 epinephrine | No pain or weak/mild pain during access and instrumentation using VAS |
| 2 | Mehrvarzfar, 2014 [72] | 61 | Maxillary molars | Symptomatic | 31 patients received local infiltration and 0.8 mL of fentanyl (40 μg). | 30 patients received local infiltration and sterile normal saline solution | 2% lignocaine, containing 1:80000 epinephrine | 2 consecutive negative reading of EPT (maximum 80) |
| 3 | Elsharrawy, 2007 [73] | 40 | Maxillary molars | Symptomatic | 20 patients received infiltration and intraligamental 0.4 mL fentanyl 0.05 mg/ml | 20 patients received infiltration and intraligamental mepivacaine | 1.8 mL of 2% mepivacaine with 1:200 000 epinephrine | Success was recorded as “none” or “mild” pain. |
| 4 | Atasoy, 2014 [74] | 50 | Maxillary first molar | Symptomatic | 25 patients received 4% articaine HCl + 1:100 000 epinephrine infiltration | 20 patients received 4% articaine HCl + 1:100 000 Epinephrine bitartrate infiltration | Articaine | Successful pulpal anesthesia. |
| 5 | Srinivasan, 2009 [75] | 40 | Maxillary posterior tooth | Symptomatic | 20 patients received 4% articaine with epinephrine 1:100 000 infiltration | 20 patients received 2% lignocaine with epinephrine 1:100 000 infiltration | Articaine and lignocaine | No pain or weak/mild pain during access and instrumentation using VAS scale |
| 6 | Hosseini, 2016 [76] | 40 | Maxillary first molar | Symptomatic | 20 patients received BI of 1.8 mL of 4% articaine with 1:100000 epinephrine | 20patients received BI of 1.8 mL 2% lignocaine with 1:80000 epinephrine | Articaine | Absence of pain or mild discomfort |
| 7 | Ramachandran, 2012 [77] | 100 | Maxillary first molar | Symptomatic | Premedication with 1000 mg of paracetamol or 800 mg of ibuprofen, 100 mg aceclofenac and infiltration | Premedication with placebo and infiltration | 2% lignocaine with epinephrine 1:200 000 | Absence of pain during access preparation and root canal instrumentation |
| 8 | Kanna 2012 [78] | 50 | Maxillary teeth | Symptomatic | 2.0 mL 4% articaine with 1:100 000 epinephrine BI | 2% lidocaine with 1:80,000 epinephrine BI | Articaine and lignocaine | No response was obtained to the maximum stimulation (80 reading) of the pulp tester |
| Study of both maxillary and mandibular teeth | ||||||||
| 1 | Nusstein, 1998 [79] | 51 | Mandibular or maxillary molar or premolar | Symptomatic | 26 patients received IANB or BI in addition to IO | 25 received conventional IANB or BI | 2% lignocaine with 1:100 000 epinephrine. | No pain or weak/mild pain during access and instrumentation using VAS scale |
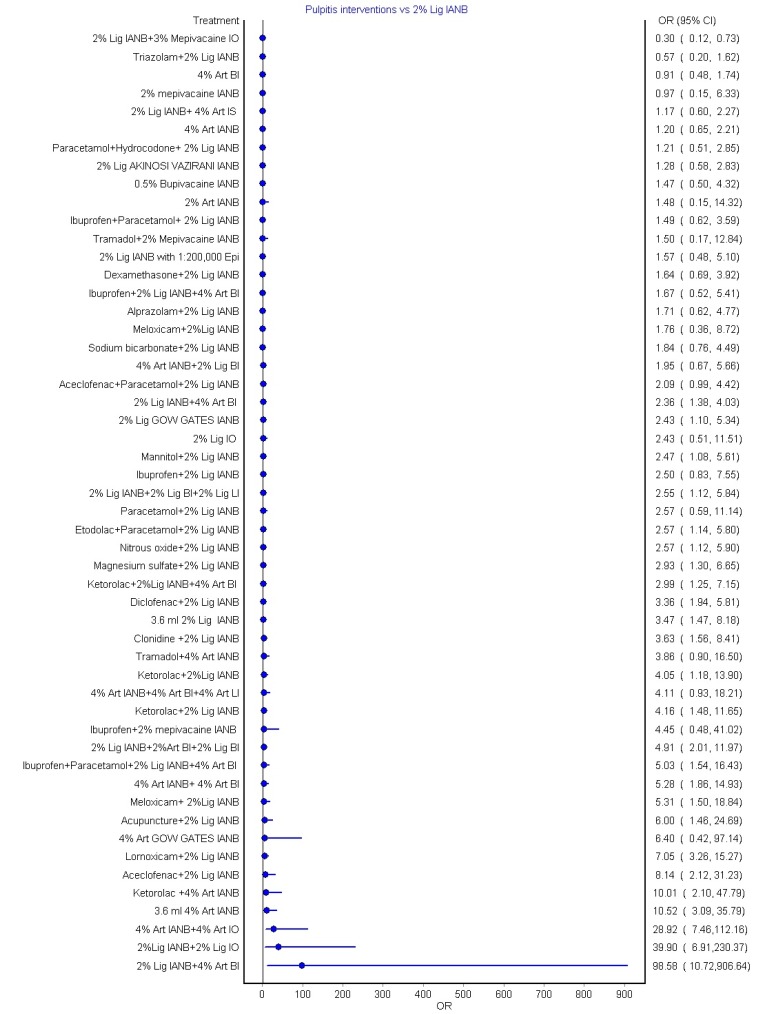
2. Direct comparison: Pooled results for mandibular anesthetic techniques
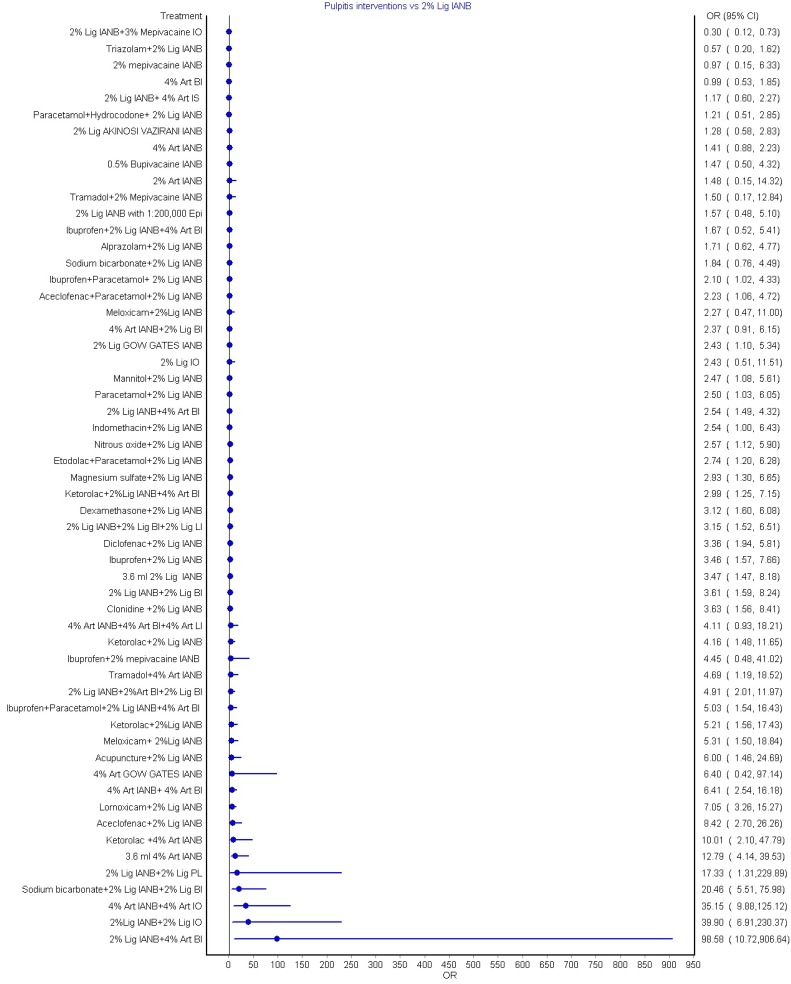
3. Indirect comparison: Pooled results for mandibular anesthetic techniques
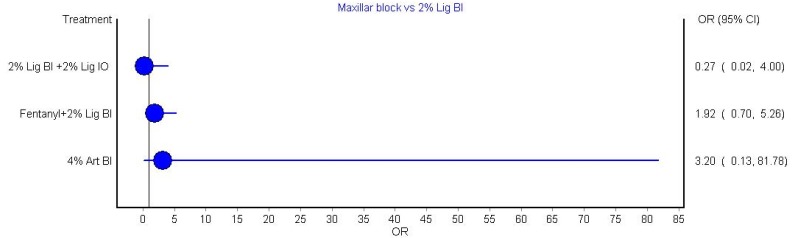
4. Indirect comparison: Pooled results for maxillary anesthetic techniques
5. Grading the evidence
Table 2
Grading the quality of evidence for key comparisons using 2% lignocaine IANB for the success of anesthesia
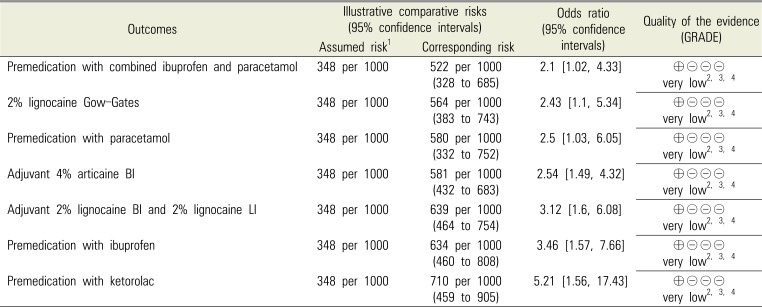
1—Assumed risk was the median control group risk across the studies
2—Downgraded one level as publication bias could not be assessed
3—Downgraded one level for imprecision of the estimates, as evident by the wider confidence intervals
4—Downgraded one level for low sample size
Very low quality: Marked uncertain about the estimate.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download