1. GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388:1659–1724. PMID:
27733284.
3. Achelrod D, Wenzel U, Frey S. Systematic review and metaanalysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015; 28:355–361. PMID:
25156625.

4. Tsioufis CP, Papademetriou V, Dimitriadis KS, Kasiakogias A, Tsiachris D, Worthley MI, et al. Catheter-based renal denervation for resistant hypertension: twenty-four month results of the EnligHTN I first-in-human study using a multi-electrode ablation system. Int J Cardiol. 2015; 201:345–350. PMID:
26301677.

5. Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009; 373:1275–1281. PMID:
19332353.

6. Gordan R, Gwathmey JK, Xie LH. Autonomic and endocrine control of cardiovascular function. World J Cardiol. 2015; 7:204–214. PMID:
25914789.

7. Chen PS, Chen LS, Fishbein MC, Lin SF, Nattel S. Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ Res. 2014; 114:1500–1515. PMID:
24763467.
8. Flack JM, Bhatt DL, Kandzari DE, Brown D, Brar S, Choi JW, et al. SYMPLICITY HTN-3 Investigators. An analysis of the blood pressure and safety outcomes to renal denervation in African Americans and Non-African Americans in the SYMPLICITY HTN-3 trial. J Am Soc Hypertens. 2015; 9:769–779. PMID:
26362830.

9. Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014; 370:1393–1401. PMID:
24678939.

10. Vink EE, Goldschmeding R, Vink A, Weggemans C, Bleijs RL, Blankestijn PJ. Limited destruction of renal nerves after catheter-based renal denervation: results of a human case study. Nephrol Dial Transplant. 2014; 29:1608–1610. PMID:
24875664.

11. Choe WS, Song WH, Jeong CW, Choi EK, Oh S. Anatomic conformation of renal sympathetic nerve fibers in living human tissues. Sci Rep. 2019; 9:4831. PMID:
30886195.

12. Atherton DS, Deep NL, Mendelsohn FO. Micro-anatomy of the renal sympathetic nervous system: a human postmortem histologic study. Clin Anat. 2012; 25:628–633. PMID:
21976355.

13. Tarzamni MK, Nezami N, Rashid RJ, Argani H, Hajealioghli P, Ghorashi S. Anatomical differences in the right and left renal arterial patterns. Folia Morphol (Warsz). 2008; 67:104–110. PMID:
18521808.
14. Olsen LK, Kamper AL, Svendsen JH, Feldt-Rasmussen B. Renal denervation. Eur J Intern Med. 2015; 26:95–105. PMID:
25676808.

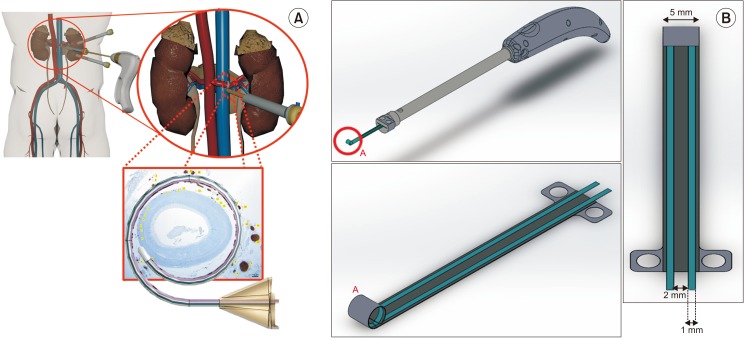
15. Ye E, Baik J, Lee S, Ryu SY, Yang S, Choi EK, et al. Design and simulation of novel laparoscopic renal denervation system: a feasibility study. Int J Hyperthermia. 2018; 35:9–18. PMID:
29772927.

16. Gill IS. Retroperitoneal laparoscopic nephrectomy. Urol Clin North Am. 1998; 25:343–360. PMID:
9633590.

17. Kuntz C, Wunsch A, Bödeker C, Bay F, Rosch R, Windeler J, et al. Effect of pressure and gas type on intraabdominal, subcutaneous, and blood pH in laparoscopy. Surg Endosc. 2000; 14:367–371. PMID:
10790557.

18. Gettman MT, Box G, Averch T, Cadeddu JA, Cherullo E, Clayman RV, et al. Consensus statement on natural orifice transluminal endoscopic surgery and single-incision laparoscopic surgery: heralding a new era in urology? Eur Urol. 2008; 53:1117–1120. PMID:
18304726.

19. Lee JK, Oh JJ, Lee S, Lee SB, Byun SS, Lee SE, et al. A new sliding-loop technique in renorrhaphy for partial nephrectomy: a feasibility study in a porcine model. Surg Innov. 2016; 23:130–133. PMID:
26169258.
20. Jung JW, Cha WH, Lee BK, Lee S, Lee SB, Lee SE, et al. Laparoendoscopic single-site surgery using innovative articulating instruments: preclinical evaluation of the prototype. J Endourol. 2014; 28:281–285. PMID:
24090367.

21. Choi EK, Shen MJ, Han S, Kim D, Hwang S, Sayfo S, et al. Intrinsic cardiac nerve activity and paroxysmal atrial tachyarrhythmia in ambulatory dogs. Circulation. 2010; 121:2615–2623. PMID:
20529998.

22. Táborský M, Richter D, Tonar Z, Kubíková T, Herman A, Peregrin J, et al. Early morphologic alterations in renal artery wall and renal nerves in response to catheter-based renal denervation procedure in sheep: difference between single-point and multiple-point ablation catheters. Physiol Res. 2017; 66:601–614. PMID:
28406699.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download