1. Kadri SS, Rhee C, Strich JR, Morales MK, Hohmann S, Menchaca J, et al. Estimating ten-year trends in septic shock incidence and mortality in United States academic medical centers using clinical data. Chest. 2017; 151(2):278–285. PMID:
27452768.
2. Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005; 365(9453):63–78. PMID:
15639681.

3. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017; 43(3):304–377. PMID:
28101605.
4. Hollenberg SM. Vasoactive drugs in circulatory shock. Am J Respir Crit Care Med. 2011; 183(7):847–855. PMID:
21097695.

5. Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, et al. Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA. 2016; 316(5):509–518. PMID:
27483065.
6. Vail EA, Gershengorn HB, Hua M, Walkey AJ, Wunsch H. Epidemiology of vasopressin use for adults with septic shock. Ann Am Thorac Soc. 2016; 13(10):1760–1767. PMID:
27404213.

7. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013; 369(9):840–851. PMID:
23984731.

8. Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008; 358(9):877–887. PMID:
18305265.

9. Russell JA. Vasopressin in vasodilatory and septic shock. Curr Opin Crit Care. 2007; 13(4):383–391. PMID:
17599007.

10. Landry DW, Levin HR, Gallant EM, Ashton RC Jr, Seo S, D'Alessandro D, et al. Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation. 1997; 95(5):1122–1125. PMID:
9054839.

11. Tsuneyoshi I, Yamada H, Kakihana Y, Nakamura M, Nakano Y, Boyle WA 3rd. Hemodynamic and metabolic effects of low-dose vasopressin infusions in vasodilatory septic shock. Crit Care Med. 2001; 29(3):487–493. PMID:
11373409.

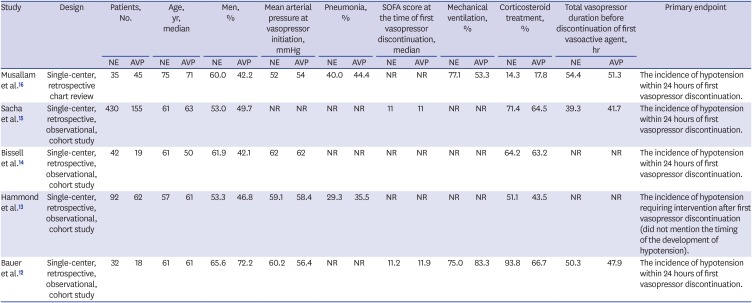
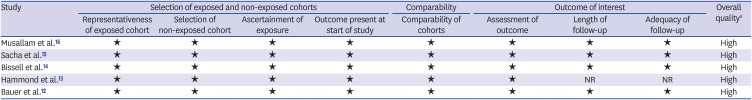
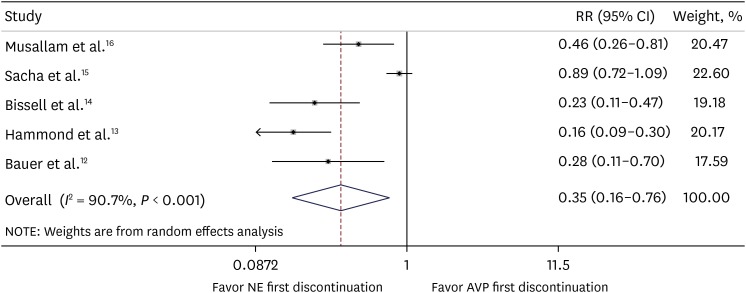
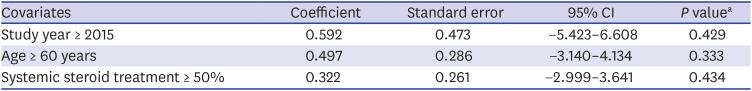
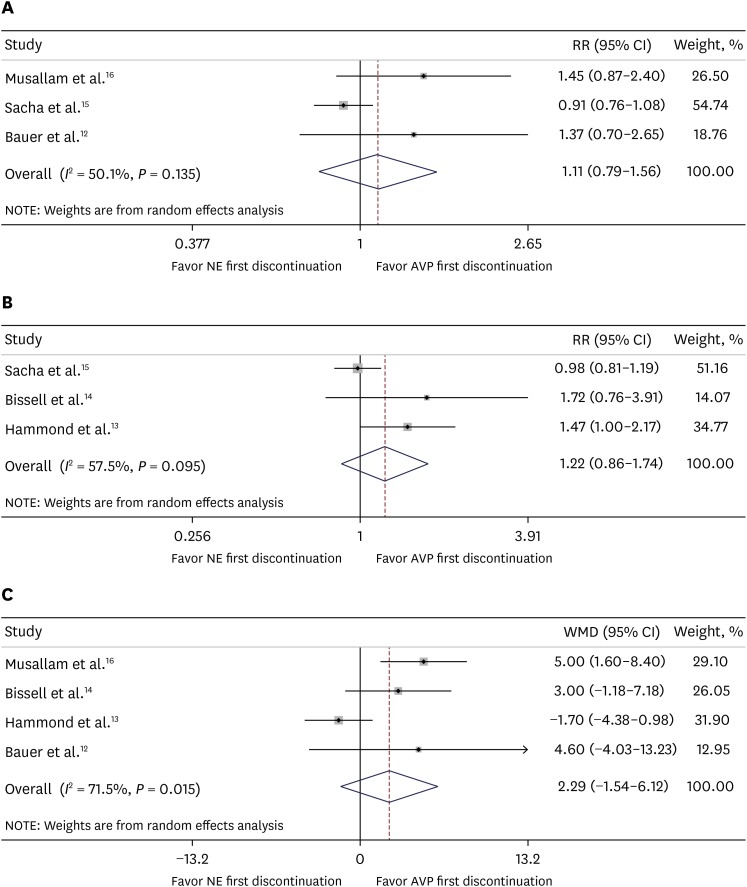
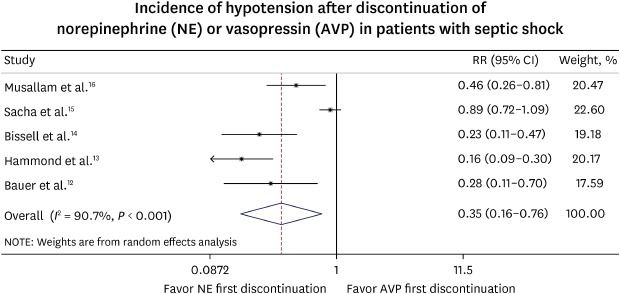
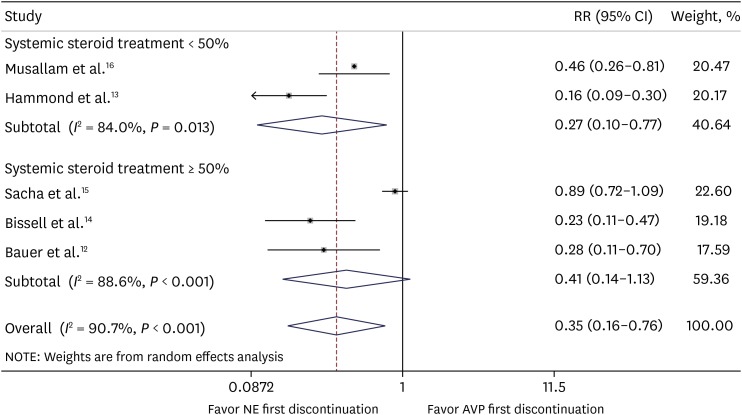
12. Bauer SR, Aloi JJ, Ahrens CL, Yeh JY, Culver DA, Reddy AJ. Discontinuation of vasopressin before norepinephrine increases the incidence of hypotension in patients recovering from septic shock: a retrospective cohort study. J Crit Care. 2010; 25(2):362.e7–362.11.

13. Hammond DA, McCain K, Painter JT, Clem OA, Cullen J, Brotherton AL, et al. Discontinuation of vasopressin before norepinephrine in the recovery phase of septic shock. J Intensive Care Med. 2019; 34(10):805–810. PMID:
28618919.

14. Bissell BD, Magee C, Moran P, Bastin ML, Flannery AH. Hemodynamic instability secondary to vasopressin withdrawal in septic shock. J Intensive Care Med. 2019; 34(9):761–765. PMID:
28750598.

15. Sacha GL, Lam SW, Duggal A, Torbic H, Reddy AJ, Bauer SR. Hypotension risk based on vasoactive agent discontinuation order in patients in the recovery phase of septic shock. Pharmacotherapy. 2018; 38(3):319–326. PMID:
29328496.

16. Musallam N, Altshuler D, Merchan C, Zakhary B, Aberle C, Papadopoulos J. Evaluating vasopressor discontinuation strategies in patients with septic shock on concomitant norepinephrine and vasopressin infusions. Ann Pharmacother. 2018; 52(8):733–739. PMID:
29560736.

17. Rachoin JS, Dellinger RP. Timing of norepinephrine in septic patients: not too little too late. Crit Care. 2014; 18(6):691. PMID:
25672524.

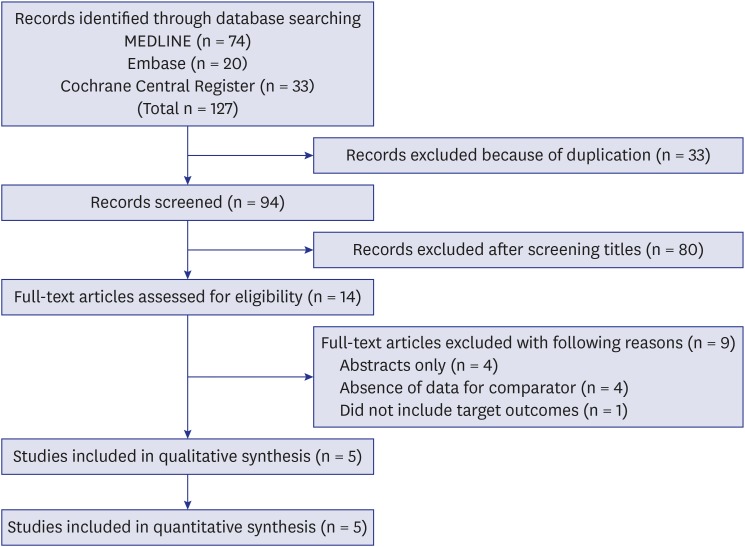
18. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151(4):264–269. PMID:
19622511.

20. Thompson SG. Why sources of heterogeneity in meta-analysis should be investigated. BMJ. 1994; 309(6965):1351–1355. PMID:
7866085.
21. Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, van der Meulen JH, et al. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999; 282(11):1061–1066. PMID:
10493205.

22. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315(7109):629–634. PMID:
9310563.

23. Russell JA, Walley KR, Gordon AC, Cooper DJ, Hébert PC, Singer J, et al. Interaction of vasopressin infusion, corticosteroid treatment, and mortality of septic shock. Crit Care Med. 2009; 37(3):811–818. PMID:
19237882.

24. Gordon AC, Mason AJ, Perkins GD, Stotz M, Terblanche M, Ashby D, et al. The interaction of vasopressin and corticosteroids in septic shock: a pilot randomized controlled trial. Crit Care Med. 2014; 42(6):1325–1333. PMID:
24557425.
25. Landry DW, Levin HR, Gallant EM, Seo S, D'Alessandro D, Oz MC, et al. Vasopressin pressor hypersensitivity in vasodilatory septic shock. Crit Care Med. 1997; 25(8):1279–1282. PMID:
9267938.

26. Mutlu GM, Factor P. Role of vasopressin in the management of septic shock. Intensive Care Med. 2004; 30(7):1276–1291. PMID:
15103461.

27. Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D. Circulating vasopressin levels in septic shock. Crit Care Med. 2003; 31(6):1752–1758. PMID:
12794416.

28. Jochberger S, Mayr VD, Luckner G, Wenzel V, Ulmer H, Schmid S, et al. Serum vasopressin concentrations in critically ill patients. Crit Care Med. 2006; 34(2):293–299. PMID:
16424705.

29. Pietranera L, Saravia F, Roig P, Lima A, De Nicola AF. Mineralocorticoid treatment upregulates the hypothalamic vasopressinergic system of spontaneously hypertensive rats. Neuroendocrinology. 2004; 80(2):100–110. PMID:
15475662.

30. Amado J, Gago P, Santos W, Mimoso J, de Jesus I. Cardiogenic shock: Inotropes and vasopressors. Rev Port Cardiol. 2016; 35(12):681–695. PMID:
27836218.

31. Jeon K, Song JU, Chung CR, Yang JH, Suh GY. Incidence of hypotension according to the discontinuation order of vasopressors in the management of septic shock: a prospective randomized trial (DOVSS). Crit Care. 2018; 22(1):131. PMID:
29784057.

32. Reilly JM, Cunnion RE, Burch-Whitman C, Parker MM, Shelhamer JH, Parrillo JE. A circulating myocardial depressant substance is associated with cardiac dysfunction and peripheral hypoperfusion (lactic acidemia) in patients with septic shock. Chest. 1989; 95(5):1072–1080. PMID:
2707065.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download