Abstract
Background
This is the first study on the blood donation trend in Iran at a national level. We report different characteristics of blood donation such as demographic status, donor type, donation trend, and geographical distribution of blood donation in Iran between 2003 and 2017.
Methods
This study used data registered in the donor vigilance part of the Iranian Blood Transfusion Organization. Statistical analysis was conducted using SPSS (SPSS Inc., Chicago, IL, USA) and ArcMap GIS version 10.2 software. A P-value <0.05 was considered statistically significant.
Results
Based on the study results, blood donation in Iran reached >2 million units in 2017; moreover, it is predicted that Iran will achieve >29 donations per 1,000 population in 2022. The proportion of regular and repeated donors increased from 77% in 2013 to 87% in 2017. The average blood donation rate in seven provinces was higher than the national average, and the average growth rate of their blood donation per population was positive.
Conclusion
The results of the current study showed that there is a recent increasing trend toward blood donation in Iran. Furthermore, the largest share of donations is related to regular donors. The increasing proportion of regular and repeated donors has led to the improvement in the quality and consequently health level of donated blood.
Blood transfusion is the process of receiving blood from another individual (donor). It is an extremely safe procedure that can save millions of lives worldwide. Some of the main indications for blood transfusion are anemia, thalassemia, cancer, and trauma [1].
The World Health Organization (WHO) has always emphasized that the blood transfusion organization should be part of the healthcare system and independently monitor the blood donation process [23]. According to a WHO report, annually, approximately 112.5 million blood donations are conducted worldwide [4], which indicates the importance of monitoring blood donation systems.
Iran is a Middle Eastern country, with an area of 1,648,195 km2 (636,372 sq mi). Iran's current population is >80 million, with ethnic diversity. Iran is subdivided into 31 provinces [3].
Regarding the need for blood in Iran, a statistics survey shows that blood donation is always required in this country. Iran is one of the countries located in “the thalassemia belt” with a significant annual number of newborns with thalassemia [5]. Moreover, nearly 3% of all referrals to medical centers are reportedly related to injuries [6]. Hence, blood transfusion in Iran is an essential component of the healthcare system, saving millions of lives annually.
The history of the early attempts of blood transfusion in Iran can be traced back to the 1940s; however, approximately three decades later, in 1974, the Iranian National Blood Transfusion Service was founded. Presently, Iran has not only reached a 100% nonremunerated voluntary blood donation but also secured a national self-sufficiency in blood and blood components. In all provinces of Iran, there is at least one blood donation center, which collects donated blood, conducts screening to prevent transfusion-transmitted infections, stores the blood, and provides medical centers with safe blood [1].
This is the first study on the blood donation trend in Iran at a national level. We report different characteristics of blood donation, such as demographic status, donor type, donation trend, and geographical distribution of blood donation in Iran between 2003 and 2017.
This study used the data registered in the donor vigilance part of the Iranian Blood Transfusion Organization. This section covers all activities related to surveillance of blood donors throughout Iran independently. Data on each donor, such as age, sex, donation type, and blood type, were collected at blood donation centers in all provinces in Iran and were then sent to the Donor Vigilance Unit once a month. This unit integrates all data received from different provinces and saves them in electronic files by year.
The data included the number of donors, demographic status, donor type, blood group type, and deferral rate between 2003 and 2017 for each province. The data that were used in this study and made available to us were in the integrated Excel form.
Statistical analysis was conducted using SPSS (SPSS Inc., Chicago, IL, USA) software. Chi-square test was performed for qualitative comparison among demographic variables, and linear regression was used to predict blood donation between 2003 and 2017 in Iran.
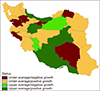
Furthermore, to analyze the status of donation in different provinces, initially, the rate of blood donation from 2011 to 2017 was calculated for each province; subsequently, these data were divided into two groups with negative and positive growth. Then, the average blood donation rate in each province was compared with the national average, and accordingly, the provinces were separated into two groups: higher and lower than the national average. Finally, they were divided into four categories and marked with different colors on the map: provinces with a negative growth rate and an average less than the national average (red), provinces with a positive growth rate and an average less than the national average (yellow), provinces with a negative growth rate and an average higher than the national average (bright green), and provinces with a positive growth rate and an average higher than the national average (dark green).
The incidence variations and spatial autocorrelation were assessed between provinces using Getis-Ord Gi and Moran's I tests, respectively. This chart was created using the ArcMap GIS version 10.2 software. A P-value <0.05 was considered statistically significant.
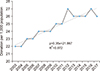
From 2003 to 2017, there were a total of 27,442,124 blood donations in Iran. The trend, which is calculated based on the whole population of the country per year, demonstrates an increase in blood donation in Iran over these years, in such a way that it has increased from 22 per 1,000 individuals in 2003 to 26 in 2017. Moreover, it is predicted that this number will increase to >29 by 2022 (Fig. 1).
In 2017, the national average blood donation rate was 26 per 1,000 individuals. Further analysis of the data showed that the trend and rate of donations can be categorized into four groups: The first group consisted of provinces that had a low rate of donation (less than the national average) and negative growth rate of donation, namely Kerman (southeast of Iran), Ilam, Kurdistan, Zanjan (west of Iran, near Iraq), Tehran (capital), and North Khorasan (east of Iran), which are depicted in the map as dark red. The second group consisted of provinces that had a low rate of donation (less than national average) but a positive growth rate of donation (depicted in yellow). Group three were composed of provinces that had a donation rate above the national average but a negative growth rate of donation (depicted in bright green). Group four consisted of provinces that had positive blood donation growth rate. Additionally, the average donation rate in these provinces was higher than the national average. These include Bandar Abbas, Blusher (bordering the Persian Gulf and Oman Sea, south of Iran), Fars (south of Iran), Mazandaran (bordering the Caspian Sea), Yazd (center of Iran), Qom, and Markazi (near Tehran, capital), which are depicted in the map as dark green (Fig. 2). The incidence variations and spatial autocorrelation were tested between provinces using Getis-Ord Gi and Moran's I tests, respectively, which revealed no significant results (P=0.1). These results showed no cluster containing a combination of the provinces; hence, there was no geographical correlation.
This 5-year survey (2013–2017) showed that women had a low proportion (4%) of blood donation overall; therefore, there was a significant difference in sex among blood donors (P<0.001). The data also indicated a significant difference among the age groups of donors (P<0.001), as the group of 30–40 years had the highest proportion (34%) of blood donation.
Another feature under consideration in this study was the type of donation. It was found that regular donors (donors with a gap of >12 mo between donations) were significantly more involved in donating blood than others. The results also showed the ratio of regular and repeated donors (donors with a gap <12 mo between donations) has increased from 77% in 2013 to 87% in 2017. The most frequent blood type among the donors was O+ and A+, with 34% and 27% of the total frequency, respectively. Therefore, this difference in blood types was also statistically significant (P<0.001).
The study of blood donation deferrals indicated that, generally, about 20% of Iranian blood donors are temporarily or permanently deferred from blood donation (refer to Table 1 for more details).
The results of this study generally show that the average blood donation rate in Iran was 26 donations per 1,000 individuals and will reach 29 donations by 2020. According to the WHO report, “based on samples of 1,000 people, the blood donation rate is 32.6 donations in high-income countries, 15.1 donations in upper-middle-income countries, 8.1 donations in lower-middle-income countries and 4.4 donations in low-income countries” [7]. Although blood donation in Iran is completely free and voluntary and financial incentives are not involved, it is one of the countries with the highest participation rate in blood donation.
The geographical distribution shows that, in provinces bordering the Caspian Sea, Persian Gulf, and Oman Sea and two provinces of Fars and Isfahan (center of Iran), the blood donation growth rate is positive, and the average blood donation rate is higher than the national average. Studies conducted on the distribution of certain diseases, such as beta thalassemia, in which blood transfusion is required, indicate that provinces bordering the Caspian Sea, Persian Gulf, and Oman Sea show the highest prevalence rate of these diseases in Iran. In a study published in 2007, these coastal provinces were among those with “very high” and “high” prevalence rates. Moreover, according to the latest report from the Iranian Legal Medicine Organization, Fars (south of Iran) is one of the provinces with the highest number of traffic accidents.
It seems that, considering the need for blood transfusion of individuals in these provinces compared to others, blood donation rate in these provinces is higher than those in other provinces.
The investigation of the characteristics of donors showed that women had a contribution of 4% to blood donation, which indicated their low participation rate. Various studies conducted worldwide showed the relatively low participation rate of women in blood donation. A study conducted in Nigeria demonstrated that women had 10% contribution to blood donation in this country [8]. Another study was performed in Romania, in which the results indicated 17.5% contribution of women to blood donation [9]. Moreover, the results of studies conducted in Ethiopia (12.1%), Netherlands (18.7%), China (18.6%), Iraq (0.3%), Qatar (2.6%), Turkey (11%), and Cameroon (19.5%) have presented that women have a small contribution to blood donation [10111213141516]. Various reasons can justify this low participation rate of women. A study conducted in Yazd (center of Iran), central Iran, which investigated the reasons of women's low participation in blood donation, showed that, despite the high awareness of women about the importance of blood transfusion, some reasons, including anemia, insufficient time, lack of husband's permission, fear, and difficulty in access to donation centers, form large barriers to their participation in blood donation [17].
The age distribution of donors demonstrated that the highest participation rate in blood donation was noted in those aged 20–40 years, which accounted for 64% of donors. The age distribution of donors in various countries showed that there were differences in the frequency of blood donation by age; however, in many cases, the age groups associated with the highest frequency in blood donation were overlapping.
The highest frequency in countries of Romania, Ethiopia, Netherlands, Iraq, Qatar, and Turkey was noted in the age groups of 18–35 (64%), 17–25 (52.8%), 50–60 (35.9%), 30–40 (37%), 25–45 (73.6%), and 30–50 (60.1%) years, respectively. It seems that, in addition to the age and physical conditions, which are the criteria for blood donation, the distribution of blood donors is affected by the age pyramid and age groups in each country. According to the latest census in Iran, the highest frequency of blood donation in the Iranian population has been observed in the age groups of 25–35 years.
The distribution of donors showed that the ratio of regular and repeated donors has increased recently and has reached 87% in the previous year. In terms of general health status, they are mostly in good condition; additionally, they tend to avoid high-risk behaviors more than others, leading to recent improvement in the quality of donated blood. The blood group distribution of donors showed that the highest frequency of blood donation was noted in those with O+. The results of other studies also showed that the blood group O is more abundant than others [1819202122]. It seems that this is the most common blood group worldwide.
Not all visitors for blood donation are qualified. To maintain the health of blood donors and recipients, some individuals are temporarily or permanently exempted. The results of this study showed that generally approximately 20% of visitors for blood donation are exempted. The studies already conducted in Isfahan (central Iran) and Shiraz (southwest Iran) reported this rate as 25.6% and 30.9%, respectively [2324]. However, in countries such as Brazil, India, Turkey, and the United States, it was 22.5%, 9%, 14%, and 12.8%, respectively. The pattern of exemption is different in various countries. The reported pattern for Iran shows that the majority of exemptions (88.6%) are temporary and more focused on first-time donors (43%). Most exemptions aim to maintain the donor's health (69%) [23].
Based on the results of the current study, there is an increasing trend toward blood donation in Iran. Furthermore, the largest proportion of donations is related to regular donors. The increasing proportion of regular and repeated donors has led to the improvement in the quality and consequently health level of donated blood. Finally, more detailed data can provide more information for health policymakers to make appropriate decisions, so it is recommended that more features from blood donors should be considered in future studies.
Figures and Tables
ACKNOWLEDGMENTS
F.Z, M.T.S, and A.S designed the study. M.T.S drafted the manuscript. M.T.S, F.Z, and M.R.B prepared and analyzed the data. AA.H and A.S clarified the content and revised the paper. The authors thank the Iranian Blood Transfusion Organization (IBTO) personnel.
Notes
References
1. Cheraghali A. Overview of blood transfusion system of Iran: 2002-2011. Iran J Public Health. 2012; 41:89–93.
2. Maghsudlu M, Nasizadeh S, Abolghasemi H, Ahmadyar S. Blood donation and donor recruitment in Iran from 1998 through 2007: ten years’ experience. Transfusion. 2009; 49:2346–2351.

3. Gharehbaghian A. Introduction of a program for voluntary blood donations in Iran (blood transfusion status in Iran). ISBT Sci Ser. 2012; 7:183–187.

4. Rigas AS, Pedersen OB, Erikstrup C, Hjalgrim H, Ullum H. Blood donation and iron deficiency. ISBT Sci Ser. 2017; 12:142–147.

5. Abolghasemi H, Amid A, Zeinali S, et al. Thalassemia in Iran: epidemiology, prevention, and management. J Pediatr Hematol Oncol. 2007; 29:233–238.
6. Soodejani M, Shirani Faradonbeh R, Hashemi S, Zahedi A, Dehghani A. Epidemiology of accidents and injuries in the city of Lordegan in 2012: a short report. J Rafsanjan Univ Med Sci. 2015; 13:917–922.
7. The WHO Global Database on Blood Safety (GDBS). Blood safety and availability. Geneva, Switzerland: World Health Organization. 2015. Accessed June 30, 2019. at https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability.
8. Ugwu AO, Madu AJ, Efobi CC, Ibegbulam OG. Pattern of blood donation and characteristics of blood donors in Enugu, Southeast Nigeria. Niger J Clin Pract. 2018; 21:1438–1443.
9. Hâţu G, Brumboiu MI, Czernichow P, Bocşan IS. The risk for hepatitis C infection in blood donors in Cluj County, Romania. Transfus Clin Biol. 2014; 21:94–97.

10. Tessema B, Yismaw G, Kassu A, et al. Seroprevalence of HIV, HBV, HCV and syphilis infections among blood donors at Gondar University Teaching Hospital, Northwest Ethiopia: declining trends over a period of five years. BMC Infect Dis. 2010; 10:111.

11. Mooij SH, Hogema BM, Tulen AD, et al. Risk factors for hepatitis E virus seropositivity in Dutch blood donors. BMC Infect Dis. 2018; 18:173.

12. Liu Y, Zeng P, Wang J, et al. Hepatitis B virus infection in a cohort of HIV infected blood donors and AIDS patients in Sichuan, China. J Transl Med. 2014; 12:164.

13. Al-Rubaye A, Tariq Z, Alrubaiy L. Prevalence of hepatitis B seromarkers and hepatitis C antibodies in blood donors in Basra, Iraq. BMJ Open Gastroenterol. 2016; 3:e000067.

14. Nasrallah GK, Al Absi ES, Ghandour R, et al. Seroprevalence of hepatitis E virus among blood donors in Qatar (2013-2016). Transfusion. 2017; 57:1801–1807.

15. Arslan O. Whole blood donor deferral rate and characteristics of the Turkish population. Transfus Med. 2007; 17:379–383.

16. Tagny CT, Nguefack-Tsague G, Fopa D, et al. Risk factors for human immunodeficiency virus among blood donors in Cameroon: evidence for the design of an Africa-specific donor history questionnaire. Transfusion. 2017; 57:1912–1921.

17. Javadzadeh Shahshahani H. Why don't women volunteer to give blood? A study of knowledge, attitude and practice of women about blood donation, Yazd, Iran, 2005. Transfus Med. 2007; 17:451–454.

18. Rao C, Shetty J. Frequency of ABO and rhesus (D) blood groups in dakshina kannada district of karnataka - a study from rural tertiary care teaching hospital in South India. Nitte Univ J Health Sci. 2014; 4:57–60.

19. Tesfaye K, Petros Y, Andargie M. Frequency distribution of ABO and Rh (D) blood group alleles in Silte Zone, Ethiopia. Egypt J Med Hum Genet. 2015; 16:71–76.

20. Hassan FM. Frequency of ABO, subgroup ABO and Rh(D) blood groups in major sudanese ethnic groups. Pak J Med Res. 2010; 49:21–24.
22. Mcarthur N, Penrose LS. World frequencies of the O, A and B blood group genes. Ann Eugen. 1951; 15:302–305.
23. Birjandi F, Gharehbaghian A, Delavari A, Rezaie N, Maghsudlu M. Blood donor deferral pattern in Iran. Arch Iran Med. 2013; 16:657–660.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download