Abstract
Congenital milia of the nipple are extremely rare, and standard treatment has not yet been established because nipple preserving excision is problematic due to the location. Although most reports show excisional biopsy resulting in good outcomes without recurrence, there is a lack of consensus about treatment modality, with several studies suggesting that incisional evacuation by needle, or a ‘wait and see’ approach represent sufficient treatment. This case report is about a recurrent case after incisional evacuation for congenital milium of the nipple. We recommend nipple preserving excision with exfoliation of the milial capsule as being the most appropriate treatment modality for congenital milium of the nipple.
Congenital milia of the nipple occur only rarely, and it has not yet been possible to establish standard treatment, given the difficulties associated with excision as a result of the location of the lesion [123]. While most reports show excisional biopsy resulting in a good outcome without recurrence, treatment modality is not universally agreed upon, and several studies argue that approaches such as ‘wait and see’ or incisional evacuation by needle or paper clip are sufficient treatments [456]. With this in mind, this study will report on a recurrent case following incisional evacuation for congenital milium of the nipple.
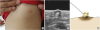
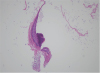
A 32 month-old girl was referred by a pediatrician to a pediatric surgeon in our hospital on account of an abscess-like lesion of the left nipple, which has existed since birth and was similar to ‘witch's milk’. She was born by normal vaginal delivery at gestational age 40 weeks, with a birth weight of 3800g. There had been no traumatic or surgical event on the left nipple in her medical history. The initial finding was a milk-colored tense nontender pustule, which covered the whole surface of the nipple. Ultrasonography showed a 6×5 mm round cyst with no specific connection to the underlying breast. Thus, on the impression of congenital milium of the nipple, incisional evacuation, which squeezes out of inner contents of the mass after incision with the tip of a 23-gauge needle was performed in the outpatient clinic, and the wound remained open (Fig. 1). Pathologic findings were compatible with an epidermal inclusion cyst showing squamous epithelium with lamellated keratinous materials (Fig. 2). After the first operation, the lesion appeared to be healed with slight elevation of left nipple, However, 16 months later, the patient revisited our hospital due to recurrence in the form of a 4×1.5 mm milk-colored, central elevation of the nipple. Excision of the lesion-containing capsule was performed with a No. 15 surgical blade in the outpatient clinic (Fig. 3). After this second operation, she improved without specific complications and had no recurrence within the follow up period of 9 months.
Congenital milia are common to the point of being developed in nearby 50% of neonates. Most are located on the face, upper trunk, or extremities, and disappear spontaneously after a few weeks [6]. However, cases developing on the nipple are extremely rare, and the location poses difficulties for excision. Standard treatment modality has therefore not yet been established. In the literature, despite the small number of studies reporting on congenital milium of the nipple, most show that excisional biopsy results in a good outcome without recurrence [5]. Other research however, argues that adequate treatments for these lesions include excisional evacuation by needle, or simply adopting a ‘wait and see’ approach [2]. This study reported a case in which secondary excision for recurrence was needed following incisional evacuation of the inner contents of the lesion. In all likelihood, recurrence after the first operation was as a result of the fact that, due to concern about preserving the nipple, the capsule of the epidermal inclusion cyst was allowed to remain. Thus, we recommend nipple preserving excision in conjunction with exfoliation of the milial capsule as being the most appropriate treatment modality for congenital milium of the nipple.
Notes
References
1. Dilek N, Dilek AR, Saral Y, Sehitoglu I. Epidermoid cyst on the nipple: a rare location. Breast J. 2014; 20:203–234.

3. Marchesi A, Parodi PC, Palitta G, Marchesi M, Vaienti L. A “polypoid” nipple: an unusual case of epidermoid cyst. J Plast Reconstr Aesthet Surg. 2014; 67:e27–e28.

4. George DE, Wasko CA, Hsu S. Surgical pearl: evacuation of milia with a paper clip. J Am Acad Dermatol. 2006; 54:326.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download