INTRODUCTION
Occupational skin diseases (OSDs) result from or become aggravated by working environments or skin contact with substances used at work.
1 Although OSDs can manifest in various forms, such as contact dermatitis, actinic keratosis, neoplasm, dermatophytosis, acne, and foreign body granulomas,
12 allergic or irritant contact dermatitis accounts for 70–95% of all OSDs. Therefore, OSDs are also referred to as occupational dermatitis.
Development of OSD is associated with contact with various agents present in the workplace. The most common substances include chemical agents (metals, acids and alkalis, aromatic hydrocarbons, lubricants, and cutting oils), physical agents (vibration, pressure, trauma, radiation, heat, and cold), and biological agents (viruses, bacteria, fungi, parasites, plants, and animals).
13 Industrial workers can be easily exposed to these agents, unlike the general population, which increases the likelihood of experiencing symptoms of OSDs. However, individual susceptibility can be affected by numerous factors, such as age, sex, race, exposed material, and occupational environment.
OSD is a common cause of occupational illnesses.
4 The proportion of individuals with OSD varies by country: 12.9–17.6% in the USA, 9.6% in France, 16% in Denmark and Finland, 22% in the UK, and 60% in industrialized countries.
5678 The economic burden caused by OSDs in Europe and the USA is high, considering direct and indirect costs for sick leave and lack of productivity.
910 In Korea, the reported number of OSD cases is low, and epidemiological data for OSD are limited, although skin disease is a common occupational disease. Because workers rarely seek medical consultations or pursue compensation schemes and believe that OSD is a transient, rather than serious and life-threatening, condition, interest in OSD among occupational physicians, allergists, and dermatologists is low due to the difficulty in diagnosing patients in a timely manner. Based on the official statistics of the Industrial Accident Compensation Insurance in Korea, 179 individuals (approximately 0.19 per 100000 workers) presented with OSDs between 2006 and 2012.
11 Epidemiological surveys have been conducted on specific occupational groups, such as automobile factory, metal handling, and health care workers, and some cases are reported in scientific publications.
121314151617 However, to our knowledge, no large-scale studies have assessed the occurrence of OSDs among all workers in Korea.
The Korean Working Conditions Survey (KWCS), a household survey conducted among workers based on probabilities proportional to systemic sampling of nationwide stratification, was developed on the basis of the European Working Condition Survey to improve working conditions and to establish new policies to enhance quality of life among workers by assessing work environments.
18 The large-scale cross-sectional nationwide KWCS has been conducted since 2006, which identifies current trends in working conditions, occupational hazards, and the health of Korean workers. Through analysis of the 4th KWCS data in 2014, this study aimed to investigate the prevalence rate and identify risk factors associated with the occurrence of OSDs among workers.
MATERIALS AND METHODS
Subjects
We used data from the 4th KWCS in 2014 conducted by the Korea Occupational Safety and Health Agency. Door-to-door interviews were conducted. The participants in the survey were selected via multi-area random sampling to ensure that the sample was representative of active Korean workers, which included wage workers, self-employed workers, and business owners aged >15 years. A total of 50007 working individuals from 17 cities were included.
OSD was defined as experiences of skin problems. If subjects answered “yes” to the question, “Over the last 12 months, did you experience any skin disease in any part of the body at your workplace or in your current job?”, they were classified into subjects with skin disease. Furthermore, subjects responding “yes” to the question, “Are your skin diseases due to your job?” among subjects with skin diseases were defined as having OSD.
Variables
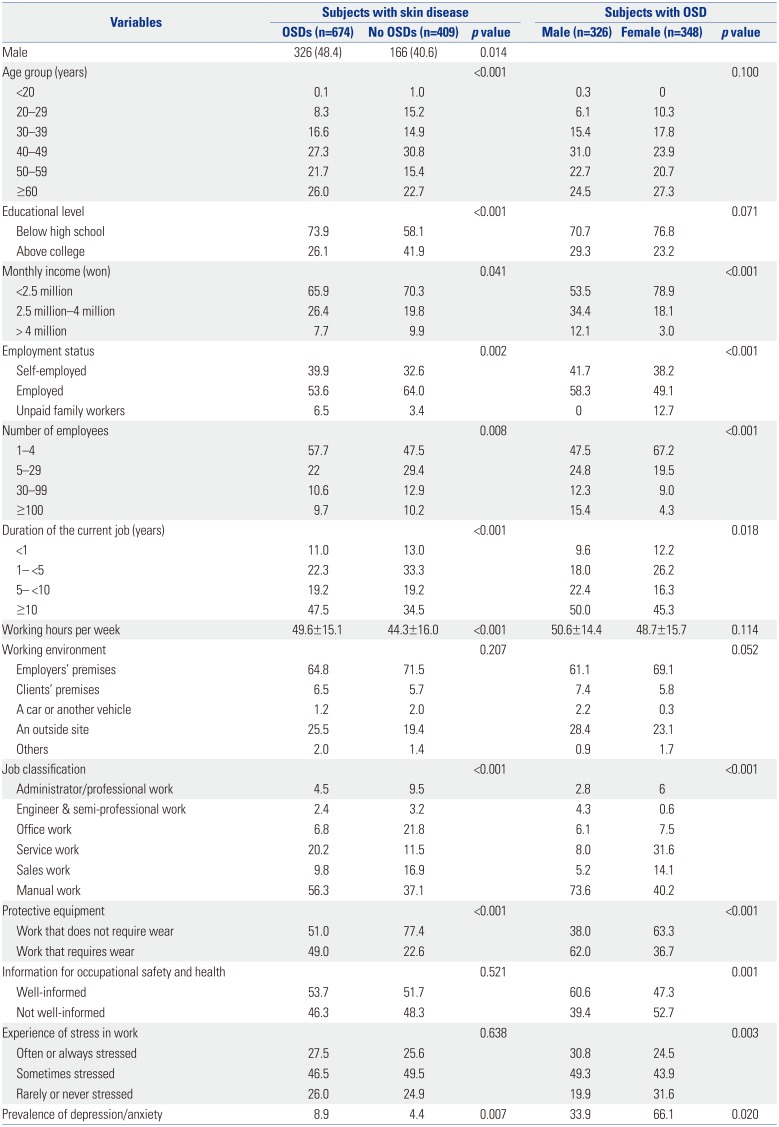
Sociodemographic variables, such as age, sex, education level, and monthly income, were included. Employment status, number of employees, working duration in the current job, working hours per week, working place, use of protective equipment, availability of information about occupational safety and health, experience of stress in work, and job and industrial classification were considered to be work-related factors. Jobs were classified as follows: administrator/professional (senior managers and professionals), engineer and semi-professional, office, service, sales, and manual work (skilled agriculture/forestry/fishery worker, technical skilled and related skill workers, equipment-machinery operators and assembly workers, and simple labor workers). Industries were classified based on the Korean Standard Industrial Classification: agriculture, forestry, fishery; manufacturing; water supply, sewage and waste management; materials recovery; construction; transportation and storage; wholesale and retail trade; accommodation and food service activities; human health and social work activities; business facility management and business support services; membership organizations, repair, and other personal services; information and communication; financial and insurance activities; real estate activities; and others (mining; electricity, gas, steam, air conditioning supply; professional, scientific, technical activities; public administration, defense, compulsory social security; education; arts, sports, recreation related services; and activities of households as employers). In addition, hazardous factors that could affect a worker's skin disease, such as vibration, high and low temperature exposure, skin contact with chemical products, and inhalation of smoke/fumes/powder/dusts or vapor, were analyzed.
Statistical analysis
All analyses were performed using the IBM Statistical Package for the Social Sciences, software version 22.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were applied for all measures. Values are presented as mean±standard deviation or frequencies (%). Student's t-test and chi-square test were used to compare differences between participants with and without OSD. To identify factors affecting OSDs, logistic regression analyses were performed. A p value <0.05 was considered significant.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of Kosin University Gospel Hospital (Approval No. 018-09-013). The need for written informed consent was waived because the study used secondary data that did not include confidential health information.
DISCUSSION
This study used data obtained from the 4th KWCS survey, which is a large-scale cross-sectional nationwide survey, to investigate the prevalence and risk factors affecting the development of work-related skin diseases among Korean workers. The present study is the first nationwide epidemiological study on OSDs in Korea. The prevalence rate of self-reported OSDs over the last 12 months was 1.35% in all workers. Although there are differences according to the survey methods, our results were similar to those of developing countries.
819 However, such rates were relatively lower than those of developed countries (9.6–17.6%).
56 The differences may be due to variations in industry structures, but may also be related to the level of disease awareness. Work-related skin disease can vary widely in severity from serious cases of dermatitis to minor skin diseases, which may not be recognized as an adverse health outcome by individuals in developing countries. Considering that we are in the process of becoming a developed country, the prevalence of OSDs in Korea may increase. It has been reported that diseases caused by chemicals are continuously decreasing in Korea.
20 Additionally, the overall incidence of OSDs in other developed countries has recently been reported as decreasing slightly,
21 with the reduction possibly having an association with increased industrial automation and better education of management, supervisors, and workers on the prevention of occupational diseases in general. Therefore, the trends for the prevalence of OSDs in Korea will require further research.
In the present study, 62.2% of workers with skin diseases presented with OSDs, although the prevalence of self-reported OSDs was not high. Of course, the prevalence of OSDs may be lower when diagnosed by a specialist.
522 Nonetheless, questionnaire-based population studies are dependent on the participants' memories, which might result in recall bias. In particular, minor skin diseases may be ignored. Additionally, some individuals are not aware of the effect of their work on the development of disease; therefore, the prevalence of OSDs among participants with skin diseases may be higher, and such results indicate that the possibility of developing OSDs must be considered in Korean workers with skin diseases.
OSD-related industries vary from country to country. According to the 2013 Centers for Disease Control and Prevention in the USA, OSDs occur frequently in individuals working in industries related to food, cosmetics, health, agriculture, cleaning, painting, machinery, printing/lithography, and construction.
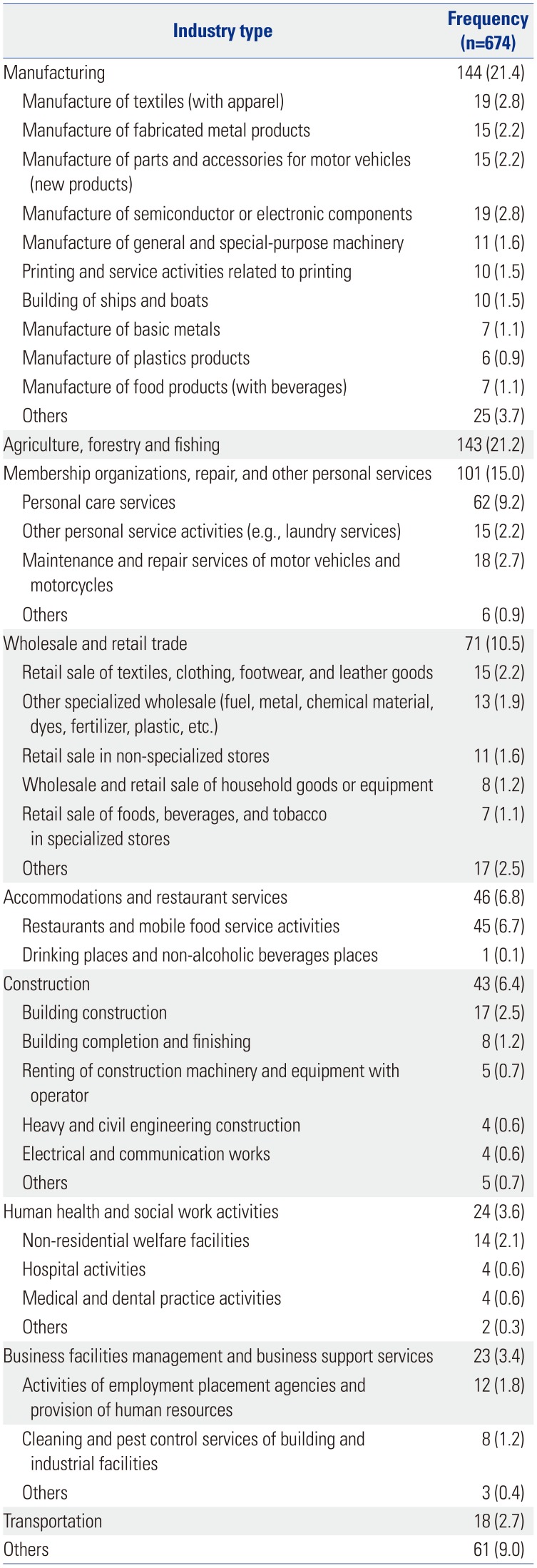
1 Our study indicates that the prevalence of OSDs is the greatest in manufacturing; agriculture and fishing; repair and personal care services; waste collection, treatment, and disposal activities; and construction industries. Moreover, textile and metal-related industries were associated with occurrences of OSD among manufacturing, repair, and other personal services, as well as wholesale and retail trade industries. Individuals working in these sectors in Korea are at risk, although we could not identify the causative agents in this study.
The probability and severity of OSD depend on the type of exposure and its duration. However, various factors, including age, gender, ethnicity, allergic status, non-occupational environmental factors (foods, drugs, cosmetics, etc.), and occupational environmental factors, influence the development of OSDs because they are caused by the combined actions of endogenous susceptibility factors and exposures to exogenous risk factors when the skin contacts an irritant or allergen.
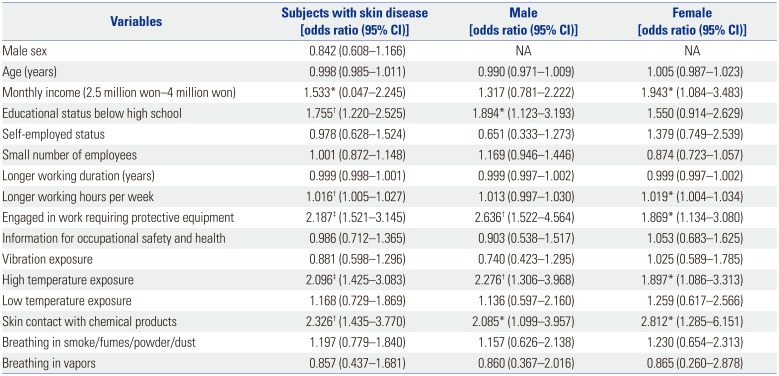
2324 In this study, we did not assess the association with atopy status or history of allergic disease because this information was not included in the KWCS data. However, our results did show that older age, lower educational level, monthly income, self-employment, working in small-sized businesses, and longer working periods and working hours per week were risk factors for developing OSD in Korea. In particular, multivariate logistic analysis showed that an educational status below high school (OR: 1.755), monthly income between 2.5 million won and 4 million won (OR: 1.533), longer working hours per work day (OR: 1.016), and engaging in work requiring protective equipment (OR: 2.187) were significant factors. This study revealed that the incidence rates of OSDs were similar in both male and female individuals. According to statistics by the Korea Occupational Safety and Health Agency from 1999 to 2007 regarding cause investigations for industrial accidents, OSDs were more commonly observed in male participants (74.2%).
25 In addition, OSD predominantly affected male or female workers in studies conducted in other countries.
57192627 Thus, we considered the analysis of gender-related differences in the occurrences of OSD. Our results showed that OSD was more common in female workers in the less educated and low-income groups. Females were more likely to be employed in service work, whereas males were more likely to be employed in manual work. Females with OSD were more involved in work that did not require the use of protective equipment, and they were not well-informed about occupational safety and health. When multivariate logistic analysis was performed for each gender, monthly income and longer working hours per week in females and an educational status below high school in males were significant risk factors for OSD development. Additionally, engaging in work requiring protective equipment was a risk factor in both females and males. Whether gender has an impact on the development of OSD is unclear, our study indicates that the risk factors associated with the progression of OSD differed according to gender. Thus, we should pay attention to gender differences when creating preventive strategies for OSD.
OSD is observed in workers exposed to a variety of different workplace hazards, from metal working fluids to other chemicals, that can cause irritation or allergic dermatitis.
23 In this study, we confirmed that handling or skin contact with chemical products was a significant risk factor (OR: 2.326). Exposure to high temperatures was also an important risk factor in this study (OR: 2.096). How exposure affects the development of OSD was not fully elucidated; however, exposure to a higher temperature is associated with poorly controlled dermatitis. Higher temperature-induced sweating causes irritation with eczema and exacerbates skin dryness via the evaporation of water on the skin surface.
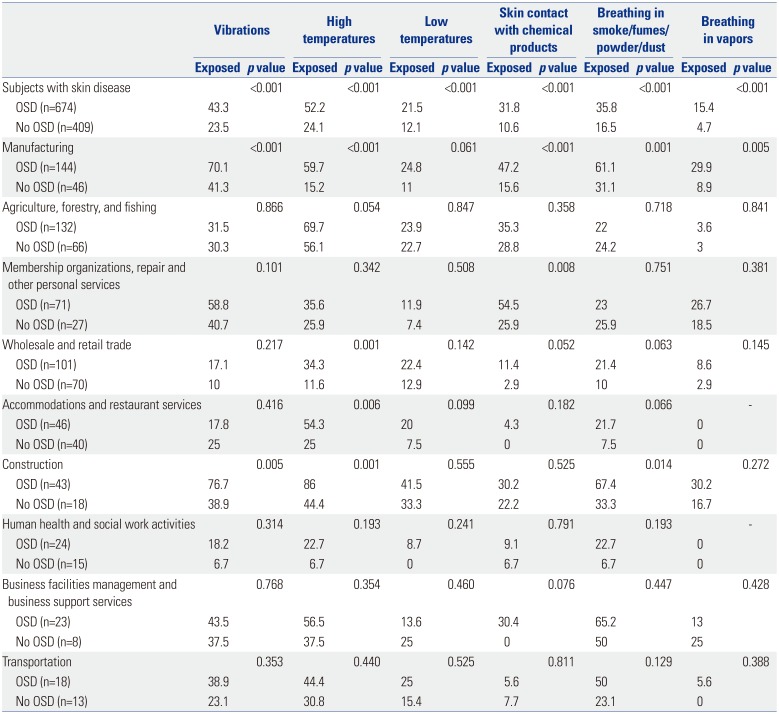
28 In this study, workers with OSD reported greater exposure to vibration, lower temperatures, and smoke/fumes/powder/dust or vapors than workers without OSD. However, these factors were not significant in the multivariate logistic analysis. However, in each industry, our results showed that the relationship between these hazardous factors and OSD differed according to industry type. Exposure to vibration was a significant hazardous risk factor in the manufacturing and construction industries; exposure to high temperatures was in manufacturing, wholesale and retail trade, accommodations and restaurant services, and construction industries; and skin contact with chemical products and exposure to breathing in smoke/fumes/powder/dust or vapors were only in the manufacturing industry. These results suggest that preventive strategies and research targets for OSD should be established considering hazardous risk factors applicable to each industry sector.
OSD is usually not a serious condition; however, it can result in conditions that are severe and difficult to treat, and it can cause discomfort and functional changes that interfere with social life and work.
823 Numerous studies have evaluated the consequences of OSD on work productivity and have reported on working days lost,
72329 although we could not find a significant difference in the loss of working days between subjects with and without OSD (data not shown). Disability is often reported, which may require adaptations or changes for a different position.
71923 Generally, the prognosis of patients with ODSs is not good.
30 Delayed recognition of OSD can result in continued exposure to causative agents, which may adversely result in a poor prognosis.
31 Therefore, preventive measures must be planned considering the risk factors associated with the development of OSD.
Approximately 30% of dermatological patients present with psychiatric problems, such as anxiety and depression.
32 These psychological problems affect work productivity, as well as quality of life and management of disease. The present study showed that depression/anxiety problems were significantly more prevalent in participants with OSD than in those without (8.9% vs. 4.4%). Although we did not investigate the association between depression/anxiety problems and quality of life and work productivity, our results indicated that such psychological problems should be considered in subjects with OSD.
The present study had some limitations with the use of the KWCS data even though the database provided socio-demographic and work-related information in Korea. First, the definition of OSD may lack objectivity. Diagnosis of OSD is based on the concordance between medical findings and those of the work environment, which can be done through allergology and skin test. However, OSD was not only defined by a specialist's diagnosis, but also by self-reporting, because OSD has been identified as a priority area for research and prevention and because information from population-based studies is also useful. Actually, many of the existing epidemiological studies for OSD have used self-reported questionnaires. Nevertheless, the possibility of underestimation due to recall bias or overestimation compared with the diagnosis of doctors should be considered. Second, because the study had a cross-sectional design, any causal relationships might be difficult to explain. Third, data were limited to those obtained from the KWCS, and we could not consider any additional risk factors, such as history of allergic disease. Despite these limitations, this study is significant, as it provided information that can improve comprehension of the current prevalence and risk factors of OSD among Korean workers.
To the best of our knowledge, this study is the first to describe the epidemiology of OSDs in Korea using nationwide KWCS data. These results provide directions for the management of risk factors to reduce the incidence of OSDs in actual workplaces. In light of the limitations in using self-reported data, further studies must be conducted to investigate causal inferences that may influence the associations highlighted in this article.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download