Firefighters are considered to have one of the most dangerous jobs. In the Republic of Korea (ROK), the number of fire service casualties has been reported to reach 2058 over the past 5 years.
1 During fire suppression and first aid rescue, firefighters are exposed to hazardous environments, making them vulnerable to various physical and mental disorders.
23 Extremely high temperatures and smoke, which contains gaseous pollutants and particulate toxins, at fire sites increase the risk of cardiovascular disease in firefighters.
456 There is also a risk to the mental health of firefighters, as they often encounter injuries or deaths.
78
Several cohort studies have investigated the risk or protective factors for physical and mental disorders among firefighters. Firefighter Obesity Research: Work-place Assessment to Reduce Disease (FORWARD) was a representative large-scale study that aimed to prevent long-term diseases caused by obesity in the United States.
7 Another cohort study investigated cancer risk among approximately 30000 firefighters working in three U.S. cities.
8 Representative large-scale studies have also been conducted in Europe. Using data from the Nordic occupational cancer project conducted in five Nordic countries (Denmark, Finland, Island, Sweden, and Norway), 16422 male firefighters were tracked for 45 years to identify their cancer patterns.
9 Moreover, in Finland, a 13-year follow-up study was conducted on the association between musculoskeletal pain and other symptoms in firefighters.
101112 Most studies have shown that firefighters are at high risk of developing occupational diseases.
1314151617
In Korea, a cohort of 33416 male firefighters, based on data from the Korea National Central Cancer Registry, was built to investigate cancer incidence from 1996 to 2007.
18 A study conducted by the Korean National Fire Agency (NFA) investigated work-related incidents over a 5-year period.
19 Although a number of similar studies have been conducted in the ROK, most of those studies used registry data or National Health Insurance claims data. Cohort studies focusing on the physical and mental health of firefighters, while considering the work and environment of firefighters, have not yet been conducted.
20 The current study's protocols were approved by the institutional review boards of Severance Hospital, Yonsei University Health System in Seoul, Korea (4-2016-0187), Wonju Severance Christian Hospital in Wonju, Korea (CR316014-002), and Gyeongsang National University Hospital in Jinju, Korea (GNUH 2016-04-015-006). In this prospective cohort study, we aimed to identify the risk and protective factors for cardiovascular disease and mental health in firefighters.
45
We recruited firefighters, fire service academy trainees, and retirees from the NFA in Korea. Baseline health examinations were conducted at three university hospitals: Severance Hospital recruited firefighters from Seoul, Gyeonggi, Chungcheongnam-do, Daejeon, and Jeollabuk-do regions; Wonju Severance Christian Hospital recruited firefighters from Gangwon and Chungcheongbuk-do regions; and Gyeongsang National University Hospital recruited firefighters from Gyeongsangbuk-do, Gyeongsangnam-do, and Jeollanam-do regions. A total of 1022 firefighters were recruited from 2016 to 2017. The participants consisted of 100 fire service academy students, 448 fire-control workers, 213 paramedics and rescue workers, 185 office administrators, and 76 retirees. According to recruiting institutions, 401 participants were recruited from Severance Hospital, 307 from Wonju Severance Christian Hospital, and 314 from Gyeongsang National University Hospital. Among these participants, 978 (95.70%) were male and 44 (4.30%) were female. Firefighters who participated in the baseline examination were followed-up every 2 years. Before starting the research, a standardized protocol was prepared and distributed to all nurses who conducted the examination. They received standardized training on screening schedules, process verification, and examination simulations.
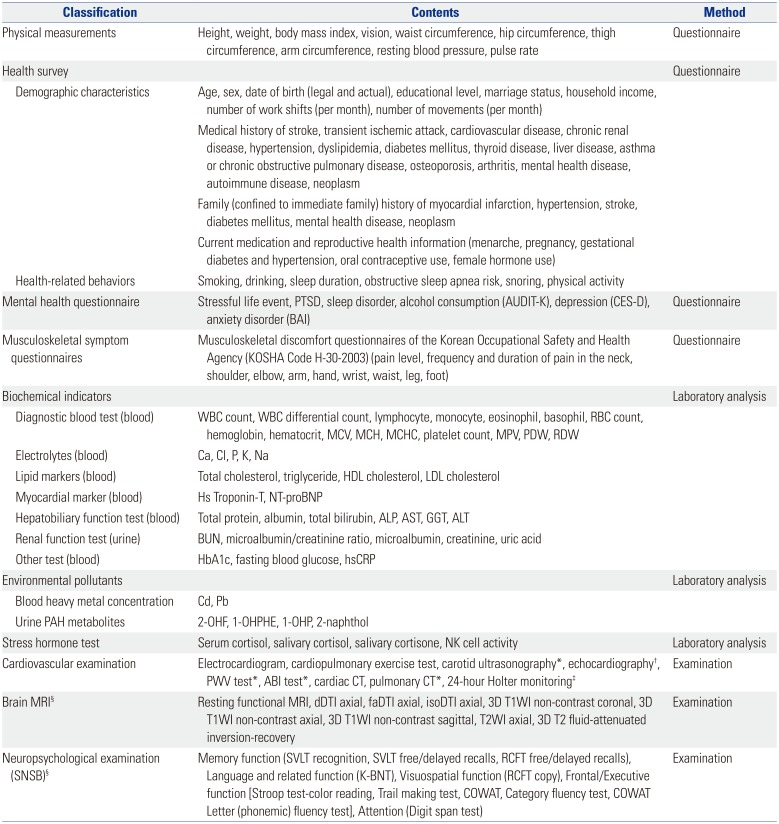
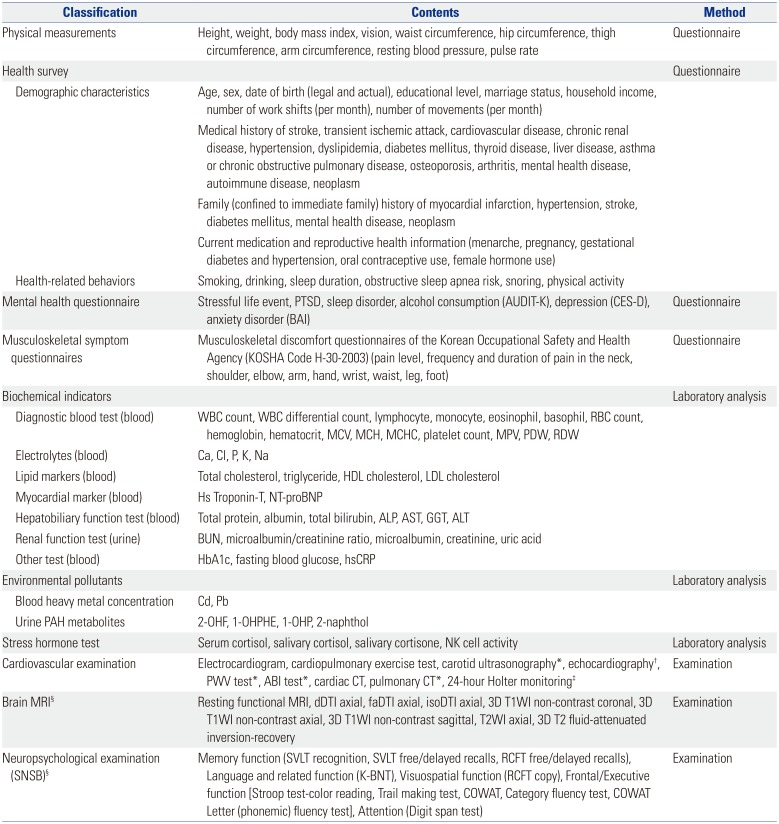
The topics and items in the questionnaires used in FRESH cohort are listed in
Table 1. All participants were interviewed by trained nurses. Questionnaires at baseline covered information on anthropometric measures and medical history, and evaluated factors related to the participants' occupational environment, such as work shifts and experience of psychological trauma.
Table 1
Elements Evaluated at Baseline in FRESH Specialized Cohort
|
Classification |
Contents |
Method |
|
Physical measurements |
Height, weight, body mass index, vision, waist circumference, hip circumference, thigh circumference, arm circumference, resting blood pressure, pulse rate |
Questionnaire |
|
Health survey |
|
Questionnaire |
|
Demographic characteristics |
Age, sex, date of birth (legal and actual), educational level, marriage status, household income, number of work shifts (per month), number of movements (per month) |
|
|
Medical history of stroke, transient ischemic attack, cardiovascular disease, chronic renal disease, hypertension, dyslipidemia, diabetes mellitus, thyroid disease, liver disease, asthma or chronic obstructive pulmonary disease, osteoporosis, arthritis, mental health disease, autoimmune disease, neoplasm |
|
Family (confined to immediate family) history of myocardial infarction, hypertension, stroke, diabetes mellitus, mental health disease, neoplasm |
|
Current medication and reproductive health information (menarche, pregnancy, gestational diabetes and hypertension, oral contraceptive use, female hormone use) |
|
Health-related behaviors |
Smoking, drinking, sleep duration, obstructive sleep apnea risk, snoring, physical activity |
|
Mental health questionnaire |
Stressful life event, PTSD, sleep disorder, alcohol consumption (AUDIT-K), depression (CES-D), anxiety disorder (BAI) |
Questionnaire |
|
Musculoskeletal symptom questionnaires |
Musculoskeletal discomfort questionnaires of the Korean Occupational Safety and Health Agency (KOSHA Code H-30-2003) (pain level, frequency and duration of pain in the neck, shoulder, elbow, arm, hand, wrist, waist, leg, foot) |
Questionnaire |
|
Biochemical indicators |
|
|
|
Diagnostic blood test (blood) |
WBC count, WBC differential count, lymphocyte, monocyte, eosinophil, basophil, RBC count, hemoglobin, hematocrit, MCV, MCH, MCHC, platelet count, MPV, PDW, RDW |
|
|
Electrolytes (blood) |
Ca, Cl, P, K, Na |
|
Lipid markers (blood) |
Total cholesterol, triglyceride, HDL cholesterol, LDL cholesterol |
|
Myocardial marker (blood) |
Hs Troponin-T, NT-proBNP |
|
Hepatobiliary function test (blood) |
Total protein, albumin, total bilirubin, ALP, AST, GGT, ALT |
|
Renal function test (urine) |
BUN, microalbumin/creatinine ratio, microalbumin, creatinine, uric acid |
|
Other test (blood) |
HbA1c, fasting blood glucose, hsCRP |
|
Environmental pollutants |
|
Laboratory analysis |
|
Blood heavy metal concentration |
Cd, Pb |
|
|
Urine PAH metabolites |
2-OHF, 1-OHPHE, 1-OHP, 2-naphthol |
|
Stress hormone test |
Serum cortisol, salivary cortisol, salivary cortisone, NK cell activity |
Laboratory analysis |
|
Cardiovascular examination |
Electrocardiogram, cardiopulmonary exercise test, carotid ultrasonography*, echocardiography†, PWV test*, ABI test*, cardiac CT, pulmonary CT*, 24-hour Holter monitoring‡
|
Examination |
|
Brain MRI§
|
Resting functional MRI, dDTI axial, faDTI axial, isoDTI axial, 3D T1WI non-contrast coronal, 3D T1WI non-contrast axial, 3D T1WI non-contrast sagittal, T2WI axial, 3D T2 fluid-attenuated inversion-recovery |
Examination |
|
Neuropsychological examination (SNSB)§
|
Memory function (SVLT recognition, SVLT free/delayed recalls, RCFT free/delayed recalls), Language and related function (K-BNT), Visuospatial function (RCFT copy), Frontal/Executive function [Stroop test-color reading, Trail making test, COWAT, Category fluency test, COWAT Letter (phonemic) fluency test], Attention (Digit span test) |
Examination |

Musculoskeletal symptoms were surveyed using the Musculoskeletal Discomfort questionnaire of the Korean Occupational Safety and Health Agency (KOSHA), which is based on the musculoskeletal symptom criteria established by the National Institute for Occupational Safety and Health in the United States.
21 Ocular surface disease index (OSDI) survey was used to assess dry eye symptoms.
22 Currently, the regular health examination program performed by the NFA includes slit-lamp examination, fundus photography, ocular tonometry, and eyesight test; therefore, considering the redundancy of the examination, we only included xerophthalmia survey.
23
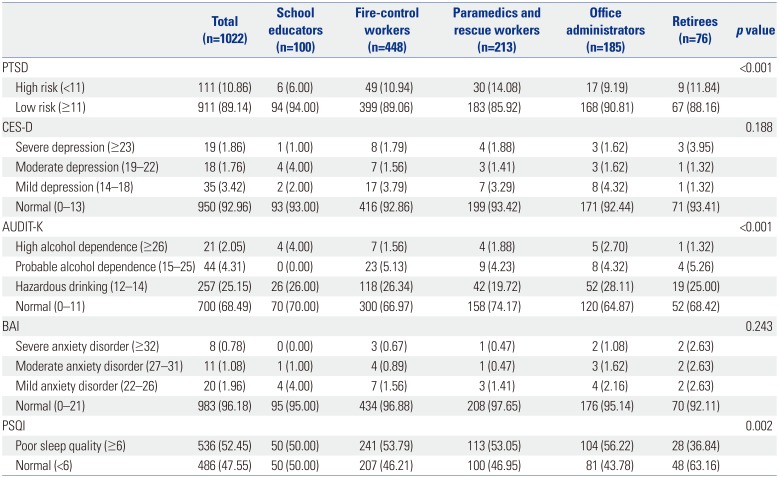
To measure mental health status, we included questionnaires on post-traumatic stress disorder (PTSD), sleep disorder, depression, and anxiety disorder. PTSD was measured using the PTSD Checklist-Specific (PCL-S).
2425 Sleep disorders were measured using the Pittsburgh Sleep Quality Index (PSQI), and depression was characterized by a shortened Center for Epidemiologic Studies Depression scale (CES-D).
2627 The Alcohol Use Disorders Identification Test in Korea (AUDIT-K) was used to evaluate alcohol consumption; finally, the Beck Anxiety Inventory (BAI) was used to measure anxiety disorders as follows: severe anxiety (BAI score ≥32), moderate anxiety (27–31), mild anxiety (22–26), and normal (0–21).
2829 The following blood indices were measured: biochemical indicators, diagnostic blood test, electrolytes lipid markers, myocardial marker, hepatobiliary function test, renal function test, blood glucose-related test, and high-sensitivity C-reactive protein (hsCRP).
Firefighters are often exposed to various health hazards, especially heavy metals and persistent organic pollutants. The concentrations of two heavy metals (lead, cadmium) and four polycyclic aromatic hydrocarbons (PAHs; 2-naphthol, 2-hydroxyfluorene, 1-hydroxyphenanthrene, 1-hydroxypyrene) were measured in the blood and urine, respectively.
For stress-related hormone measurements, the level of serum cortisol, salivary cortisol, and cortisone were measured, and hair was collected to perform long-term stress hormone analysis. Natural killer (NK) cell activity was measured to examine the relationship between immune function and stress.
Among the 1022 participants, 352 further underwent 3 Tesla (3T) brain magnetic resonance imaging (MRI), as firefighters are exposed to particulate matter and carbon monoxides and are at risk of mild traumatizing brain injury; these could result in structural and functional abnormalities in the brain. The brain MRI protocols included the following: dTI axial, faDTI axial, isoDTI axial, 3D T1WI non-contrast coronal, 3D T1WI non-contrast axial, 3D T1WI non-contrast sagittal, T2WI axial, resting functional MRI, and 3D T2 fluid-attenuated inversion-recovery. All three hospitals used the same brain MRI protocols. Brain volume and cortical thickness were estimated using Inbrain® software (
https://www.inbrain.co.kr/).
30313233 While brain MRI can identify structural changes, neuropsychological examinations are required to identify functional abnormalities. Neuropsychological examinations not only indicate abnormalities in the functional areas of the brain, but also compare them to the average level. Participants undergoing brain MRI underwent neuropsychological testing using the Seoul Neuropsychological Screening Battery (SNSB).
34
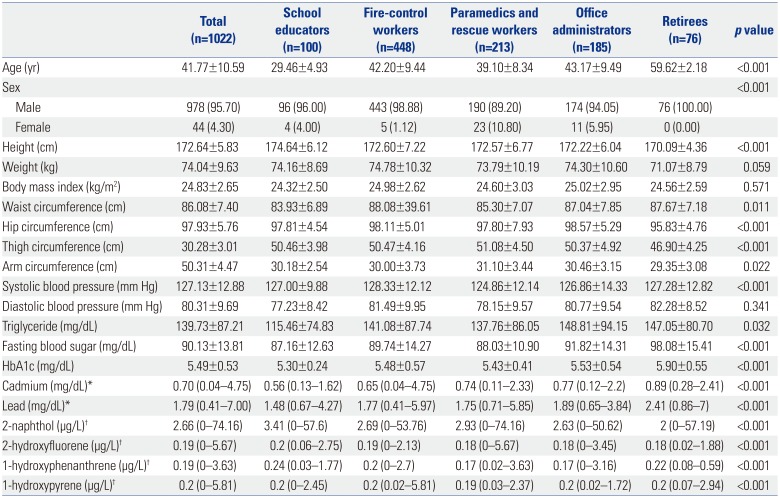
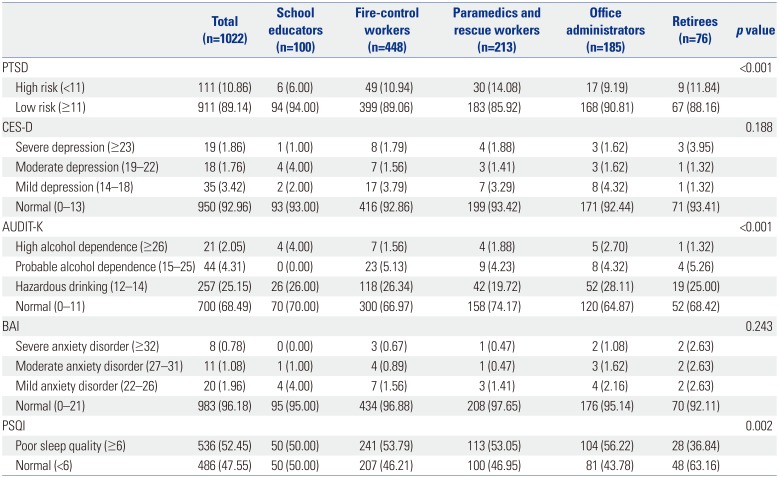
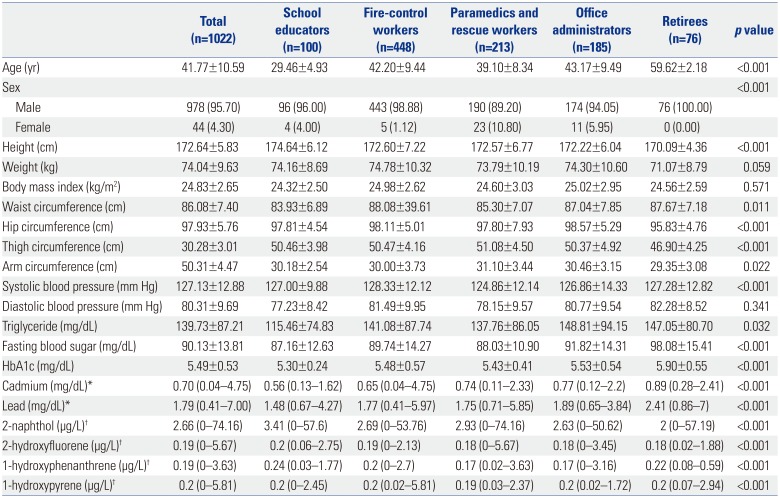
Baseline characteristics are shown in
Tables 2 and
3. Distribution and statistical significance of the variables by duty were verified, while assuming that work environment could vary greatly depending on the duty, and that the duty would have a significant effect on cardiovascular and mental health. Systolic blood pressure was the lowest in paramedics and rescue workers, and the highest in fire-control workers (
p<0.001). The proportion of participants with high-risk PTSD was 111 (10.86%). Among firefighters, the proportion of participants with high-risk PTSD (14.08%) was the highest among paramedics and rescue workers. The risk of severe depression, according to CES-D test, was the highest in retiree group. Severe anxiety was identified in eight participants (0.78%). PSQI tests showed that 486 out of 1022 participants had normal sleep quality (47.55%), whereas 536 had poor sleep quality (52.45%). SNSB test was performed in 350 participants, which included 16 fire service academy students, 177 fire-control workers, 62 paramedics and rescue workers, 59 office administrators, and 36 retirees.
Table 2
General Characteristics of Firefighters in FRESH Cohort at Baseline
|
Total (n=1022) |
School educators (n=100) |
Fire-control workers (n=448) |
Paramedics and rescue workers (n=213) |
Office administrators (n=185) |
Retirees (n=76) |
p value |
|
Age (yr) |
41.77±10.59 |
29.46±4.93 |
42.20±9.44 |
39.10±8.34 |
43.17±9.49 |
59.62±2.18 |
<0.001 |
|
Sex |
|
|
|
|
|
|
<0.001 |
|
Male |
978 (95.70) |
96 (96.00) |
443 (98.88) |
190 (89.20) |
174 (94.05) |
76 (100.00) |
|
|
Female |
44 (4.30) |
4 (4.00) |
5 (1.12) |
23 (10.80) |
11 (5.95) |
0 (0.00) |
|
|
Height (cm) |
172.64±5.83 |
174.64±6.12 |
172.60±7.22 |
172.57±6.77 |
172.22±6.04 |
170.09±4.36 |
<0.001 |
|
Weight (kg) |
74.04±9.63 |
74.16±8.69 |
74.78±10.32 |
73.79±10.19 |
74.30±10.60 |
71.07±8.79 |
0.059 |
|
Body mass index (kg/m2) |
24.83±2.65 |
24.32±2.50 |
24.98±2.62 |
24.60±3.03 |
25.02±2.95 |
24.56±2.59 |
0.571 |
|
Waist circumference (cm) |
86.08±7.40 |
83.93±6.89 |
88.08±39.61 |
85.30±7.07 |
87.04±7.85 |
87.67±7.18 |
0.011 |
|
Hip circumference (cm) |
97.93±5.76 |
97.81±4.54 |
98.11±5.01 |
97.80±7.93 |
98.57±5.29 |
95.83±4.76 |
<0.001 |
|
Thigh circumference (cm) |
30.28±3.01 |
50.46±3.98 |
50.47±4.16 |
51.08±4.50 |
50.37±4.92 |
46.90±4.25 |
<0.001 |
|
Arm circumference (cm) |
50.31±4.47 |
30.18±2.54 |
30.00±3.73 |
31.10±3.44 |
30.46±3.15 |
29.35±3.08 |
0.022 |
|
Systolic blood pressure (mm Hg) |
127.13±12.88 |
127.00±9.88 |
128.33±12.12 |
124.86±12.14 |
126.86±14.33 |
127.28±12.82 |
<0.001 |
|
Diastolic blood pressure (mm Hg) |
80.31±9.69 |
77.23±8.42 |
81.49±9.95 |
78.15±9.57 |
80.77±9.54 |
82.28±8.52 |
0.341 |
|
Triglyceride (mg/dL) |
139.73±87.21 |
115.46±74.83 |
141.08±87.74 |
137.76±86.05 |
148.81±94.15 |
147.05±80.70 |
0.032 |
|
Fasting blood sugar (mg/dL) |
90.13±13.81 |
87.16±12.63 |
89.74±14.27 |
88.03±10.90 |
91.82±14.31 |
98.08±15.41 |
<0.001 |
|
HbA1c (mg/dL) |
5.49±0.53 |
5.30±0.24 |
5.48±0.57 |
5.43±0.41 |
5.53±0.54 |
5.90±0.55 |
<0.001 |
|
Cadmium (mg/dL)*
|
0.70 (0.04–4.75) |
0.56 (0.13–1.62) |
0.65 (0.04–4.75) |
0.74 (0.11–2.33) |
0.77 (0.12–2.2) |
0.89 (0.28–2.41) |
<0.001 |
|
Lead (mg/dL)*
|
1.79 (0.41–7.00) |
1.48 (0.67–4.27) |
1.77 (0.41–5.97) |
1.75 (0.71–5.85) |
1.89 (0.65–3.84) |
2.41 (0.86–7) |
<0.001 |
|
2-naphthol (μg/L)†
|
2.66 (0–74.16) |
3.41 (0–57.6) |
2.69 (0–53.76) |
2.93 (0–74.16) |
2.63 (0–50.62) |
2 (0–57.19) |
<0.001 |
|
2-hydroxyfluorene (μg/L)†
|
0.19 (0–5.67) |
0.2 (0.06–2.75) |
0.19 (0–2.13) |
0.18 (0–5.67) |
0.18 (0–3.45) |
0.18 (0.02–1.88) |
<0.001 |
|
1-hydroxyphenanthrene (μg/L)†
|
0.19 (0–3.63) |
0.24 (0.03–1.77) |
0.2 (0–2.7) |
0.17 (0.02–3.63) |
0.17 (0–3.16) |
0.22 (0.08–0.59) |
<0.001 |
|
1-hydroxypyrene (μg/L)†
|
0.2 (0–5.81) |
0.2 (0–2.45) |
0.2 (0.02–5.81) |
0.19 (0.03–2.37) |
0.2 (0.02–1.72) |
0.2 (0.07–2.94) |
<0.001 |

Table 3
Mental Health Status of Firefighters in FRESH Cohort at Baseline
|
Total (n=1022) |
School educators (n=100) |
Fire-control workers (n=448) |
Paramedics and rescue workers (n=213) |
Office administrators (n=185) |
Retirees (n=76) |
p value |
|
PTSD |
|
|
|
|
|
|
<0.001 |
|
High risk (<11) |
111 (10.86) |
6 (6.00) |
49 (10.94) |
30 (14.08) |
17 (9.19) |
9 (11.84) |
|
|
Low risk (≥11) |
911 (89.14) |
94 (94.00) |
399 (89.06) |
183 (85.92) |
168 (90.81) |
67 (88.16) |
|
|
CES-D |
|
|
|
|
|
|
0.188 |
|
Severe depression (≥23) |
19 (1.86) |
1 (1.00) |
8 (1.79) |
4 (1.88) |
3 (1.62) |
3 (3.95) |
|
|
Moderate depression (19–22) |
18 (1.76) |
4 (4.00) |
7 (1.56) |
3 (1.41) |
3 (1.62) |
1 (1.32) |
|
|
Mild depression (14–18) |
35 (3.42) |
2 (2.00) |
17 (3.79) |
7 (3.29) |
8 (4.32) |
1 (1.32) |
|
|
Normal (0–13) |
950 (92.96) |
93 (93.00) |
416 (92.86) |
199 (93.42) |
171 (92.44) |
71 (93.41) |
|
|
AUDIT-K |
|
|
|
|
|
|
<0.001 |
|
High alcohol dependence (≥26) |
21 (2.05) |
4 (4.00) |
7 (1.56) |
4 (1.88) |
5 (2.70) |
1 (1.32) |
|
|
Probable alcohol dependence (15–25) |
44 (4.31) |
0 (0.00) |
23 (5.13) |
9 (4.23) |
8 (4.32) |
4 (5.26) |
|
|
Hazardous drinking (12–14) |
257 (25.15) |
26 (26.00) |
118 (26.34) |
42 (19.72) |
52 (28.11) |
19 (25.00) |
|
|
Normal (0–11) |
700 (68.49) |
70 (70.00) |
300 (66.97) |
158 (74.17) |
120 (64.87) |
52 (68.42) |
|
|
BAI |
|
|
|
|
|
|
0.243 |
|
Severe anxiety disorder (≥32) |
8 (0.78) |
0 (0.00) |
3 (0.67) |
1 (0.47) |
2 (1.08) |
2 (2.63) |
|
|
Moderate anxiety disorder (27–31) |
11 (1.08) |
1 (1.00) |
4 (0.89) |
1 (0.47) |
3 (1.62) |
2 (2.63) |
|
|
Mild anxiety disorder (22–26) |
20 (1.96) |
4 (4.00) |
7 (1.56) |
3 (1.41) |
4 (2.16) |
2 (2.63) |
|
|
Normal (0–21) |
983 (96.18) |
95 (95.00) |
434 (96.88) |
208 (97.65) |
176 (95.14) |
70 (92.11) |
|
|
PSQI |
|
|
|
|
|
|
0.002 |
|
Poor sleep quality (≥6) |
536 (52.45) |
50 (50.00) |
241 (53.79) |
113 (53.05) |
104 (56.22) |
28 (36.84) |
|
|
Normal (<6) |
486 (47.55) |
50 (50.00) |
207 (46.21) |
100 (46.95) |
81 (43.78) |
48 (63.16) |
|

Of the 352 brain MRI tests, 255 showed negative findings in brain. Thirteen and 11 subjects showed old infarct lesions and small vessel disease, respectively, while no participant showed acute cerebral infarction or hemorrhagic lesions. Twelve participants with neoplastic lesions had benign tumors, and no malignant tumor was observed. In addition, 60, two, and four subjects showed nonspecific blight object, atrophic changes, and normal variants (mastoid effusion, cavum septum pellucidum, cavum vergae), respectively.
FRESH cohort study was able to identify the risk and protective factors for cardiovascular disease and mental disorders in more than 1000 Korean firefighters. In order to consider the exposure variations in occupational environments, we recruited firefighters from three different regions in Korea. In addition to different variables, exposure to heavy metals and PAHs can also be used to confirm the association of occupational exposure with cardiovascular and mental disorders. Although firefighters are part of an occupational group that is vulnerable to a wide variety of mental health hazards and toxic substances, previous studies have only examined the association between mental disorders, such as anxiety disorders and PTSD, and the results of questionnaire surveys.
2324 Since 3T brain MRI and neuropsychological tests were performed in this study, it was possible to identify both functional and structural changes in the brain.
FRESH cohort offered several advantages. This was the first study to investigate cardiovascular disease and cognitive function of firefighters in Korea. While previous cohort studies on firefighters were mainly retrospective studies using secondary data, this study examined factors that affect cardiovascular disease, mental disease, and cognitive dysfunction using various clinical tests as a prospective study. In addition, inspections were conducted for firefighters nationwide using standardized screening protocols. In the study design process, standardization protocols were prepared and distributed to all researchers, and standardization training was provided to the personnel who conducted the examinations to minimize measurement errors at different institutions.
Nevertheless, our research also had some limitations. First of all, selection bias may have resulted from only including subjects who applied for the study, rather than randomly selecting the participants. For example, people who are usually interested in health-related issues may have been more likely to participate in this study, which could lead to the healthy worker effect. In addition, some of the items that should be investigated specifically for firefighters were not included in our questionnaire. For example, years of service and recent exposure to trauma can be important variables in analyzing the relationship between disease and work characteristics. To compensate for this, starting in 2018, when baseline participants began their first follow-up, we added questions about the date of entry, date of retirement (if leaving), and trauma experienced within the last 6 months.
FRESH study is available to those who are interested in collaboration. FRESH research committee requests a short research proposal, including background information, research questions, methods, and authorship. FRESH research committee is responsible for the distribution and control of data. Researchers who are interested in collaborative research can contact the FRESH investigator at
freshcohort@gmail.com.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download