1. Mandl F. Klinisches und experimentelles zur frage der lokalisierten und generalisierten ostitis fibrosa: unter besonderer berücksichtigung der therapie der letzteren. Teil 2. Arch Klin Chir. 1926; 143:245–248.
2. Niederle BE, Schmidt G, Organ CH, Niederle B. Albert J and his surgeon: a historical reevaluation of the first parathyroidectomy. J Am Coll Surg. 2006; 202:181–190. PMID:
16377512.

3. van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg. 1991; 15:688–692. PMID:
1767534.

4. Allendorf J, DiGorgi M, Spanknebel K, Inabnet W, Chabot J, Logerfo P. 1112 Consecutive bilateral neck explorations for primary hyperparathyroidism. World J Surg. 2007; 31:2075–2080. PMID:
17768656.

5. Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002; 235:665–670. PMID:
11981212.

6. Westerdahl J, Lindblom P, Bergenfelz A. Measurement of intraoperative parathyroid hormone predicts long-term operative success. Arch Surg. 2002; 137:186–190. PMID:
11822958.

7. Irvin GL 3rd, Carneiro DM, Solorzano CC. Progress in the operative management of sporadic primary hyperparathyroidism over 34 years. Ann Surg. 2004; 239:704–708. PMID:
15082975.

8. Chen H, Pruhs Z, Starling JR, Mack E. Intraoperative parathyroid hormone testing improves cure rates in patients undergoing minimally invasive parathyroidectomy. Surgery. 2005; 138:583–587. PMID:
16269285.

9. Grant CS, Thompson G, Farley D, van Heerden J. Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy: Mayo Clinic experience. Arch Surg. 2005; 140:472–478. PMID:
15897443.
10. Molinari AS, Irvin GL 3rd, Deriso GT, Bott L. Incidence of multiglandular disease in primary hyperparathyroidism determined by parathyroid hormone secretion. Surgery. 1996; 120:934–936. PMID:
8957476.

11. Lew JI, Irvin GL 3rd. Focused parathyroidectomy guided by intra-operative parathormone monitoring does not miss multiglandular disease in patients with sporadic primary hyperparathyroidism: a 10-year outcome. Surgery. 2009; 146:1021–1027. PMID:
19879612.

12. Sackett WR, Barraclough B, Reeve TS, Delbridge LW. Worldwide trends in the surgical treatment of primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Arch Surg. 2002; 137:1055–1059. PMID:
12215160.

13. Greene AB, Butler RS, McIntyre S, Barbosa GF, Mitchell J, Berber E, et al. National trends in parathyroid surgery from 1998 to 2008: a decade of change. J Am Coll Surg. 2009; 209:332–343. PMID:
19717037.

14. Nussbaum SR, Zahradnik RJ, Lavigne JR, Brennan GL, Nozawa-Ung K, Kim LY, et al. Highly sensitive two-site immunoradiometric assay of parathyrin, and its clinical utility in evaluating patients with hypercalcemia. Clin Chem. 1987; 33:1364–1367. PMID:
3608153.

15. Irvin GL 3rd, Dembrow VD, Prudhomme DL. Operative monitoring of parathyroid gland hyperfunction. Am J Surg. 1991; 162:299–302. PMID:
1683177.

16. Irvin GL 3rd, Deriso GT 3rd. A new, practical intraoperative parathyroid hormone assay. Am J Surg. 1994; 168:466–468. PMID:
7977975.

17. Irvin GL 3rd, Prudhomme DL, Deriso GT, Sfakianakis G, Chandarlapaty SK. A new approach to parathyroidectomy. Ann Surg. 1994; 219:574–579. PMID:
8185406.

18. Irvin GL 3rd, Sfakianakis G, Yeung L, Deriso GT, Fishman LM, Molinari AS, et al. Ambulatory parathyroidectomy for primary hyperparathyroidism. Arch Surg. 1996; 131:1074–1078. PMID:
8857905.

19. Kaplan EL, Yashiro T, Salti G. Primary hyperparathyroidism in the 1990s. Choice of surgical procedures for this disease. Ann Surg. 1992; 215:300–317. PMID:
1558410.
20. Mun HC, Conigrave A, Wilkinson M, Delbridge L. Surgery for hyperparathyroidism: does morphology or function matter most? Surgery. 2005; 138:1111–1120. PMID:
16360398.

21. Elliott DD, Monroe DP, Perrier ND. Parathyroid histopathology: is it of any value today? J Am Coll Surg. 2006; 203:758–765. PMID:
17084340.

22. Carneiro DM, Solorzano CC, Nader MC, Ramirez M, Irvin GL 3rd. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate. Surgery. 2003; 134:973–979. PMID:
14668730.

23. Akerstrom G, Malmaeus J, Bergstrom R. Surgical anatomy of human parathyroid glands. Surgery. 1984; 95:14–21. PMID:
6691181.
24. Uden P, Chan A, Duh QY, Siperstein A, Clark OH. Primary hyperparathyroidism in younger and older patients: symptoms and outcome of surgery. World J Surg. 1992; 16:791–797. PMID:
1413850.
25. St Goar WT. Gastrointestinal symptoms as a clue to the diagnosis of primary hyperparathyroidism: a review of 45 cases. Ann Intern Med. 1957; 46:102–118. PMID:
13395220.

26. Chan AK, Duh QY, Katz MH, Siperstein AE, Clark OH. Clinical manifestations of primary hyperparathyroidism before and after parathyroidectomy. A case-control study. Ann Surg. 1995; 222:402–412. PMID:
7677469.

27. Bilezikian JP, Potts JT Jr. Asymptomatic primary hyperparathyroidism: new issues and new questions: bridging the past with the future. J Bone Miner Res. 2002; 17:N57–N67. PMID:
12412779.
28. Eigelberger MS, Cheah WK, Ituarte PH, Streja L, Duh QY, Clark OH. The NIH criteria for parathyroidectomy in asymptomatic primary hyperparathyroidism: are they too limited. Ann Surg. 2004; 239:528–535. PMID:
15024314.
29. Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014; 99:3561–3569. PMID:
25162665.

30. Tonelli F, Spini S, Tommasi M, Gabbrielli G, Amorosi A, Brocchi A, et al. Intraoperative parathormone measurement in patients with multiple endocrine neoplasia type I syndrome and hyperparathyroidism. World J Surg. 2000; 24:556–562. PMID:
10787076.

31. Chou FF, Lee CH, Chen JB, Hsu KT, Sheen-Chen SM. Intraoperative parathyroid hormone measurement in patients with secondary hyperparathyroidism. Arch Surg. 2002; 137:341–344. PMID:
11888464.

32. Haustein SV, Mack E, Starling JR, Chen H. The role of intraoperative parathyroid hormone testing in patients with tertiary hyperparathyroidism after renal transplantation. Surgery. 2005; 138:1066–1071. PMID:
16360392.

33. Solorzano CC, Carneiro-Pla DM, Lew JI, Rodgers SE, Montano R, Irvin GL 3rd. Intra-operative parathyroid hormone monitoring in patients with parathyroid cancer. Ann Surg Oncol. 2007; 14:3216–3222. PMID:
17805932.

34. Lim JY, Herman MC, Bubis L, Epelboym I, Allendorf JD, Chabot JA, et al. Differences in single gland and multigland disease are seen in low biochemical profile primary hyperparathyroidism. Surgery. 2017; 161:70–77. PMID:
27847113.

35. Carneiro DM, Irvin GL 3rd, Inabnet WB. Limited versus radical parathyroidectomy in familial isolated primary hyperparathyroidism. Surgery. 2002; 132:1050–1054. PMID:
12490854.

36. Chiu B, Sturgeon C, Angelos P. Which intraoperative parathyroid hormone assay criterion best predicts operative success? A study of 352 consecutive patients. Arch Surg. 2006; 141:483–487. PMID:
16702520.
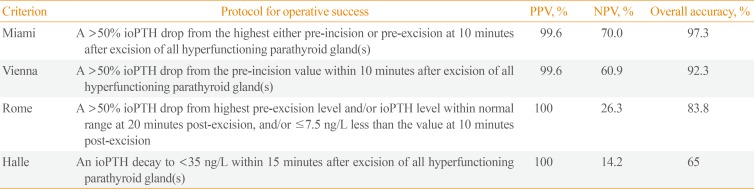
37. Barczynski M, Konturek A, Hubalewska-Dydejczyk A, Cichon S, Nowak W. Evaluation of Halle, Miami, Rome, and Vienna intraoperative iPTH assay criteria in guiding minimally invasive parathyroidectomy. Langenbecks Arch Surg. 2009; 394:843–849. PMID:
19529957.

38. Irvin GL 3rd, Solorzano CC, Carneiro DM. Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg. 2004; 28:1287–1292. PMID:
15517474.

39. Khan ZF, Picado O, Marcadis AR, Farra JC, Lew JI. Additional 20-minute intraoperative parathormone measurement can minimize unnecessary bilateral neck exploration. J Surg Res. 2019; 235:264–269. PMID:
30691805.

40. Moalem J, Ruan DT, Farkas RL, Shen WT, Miller S, Duh QY, et al. Prospective evaluation of the rate and impact of hemolysis on intraoperative parathyroid hormone (IOPTH) assay results. Ann Surg Oncol. 2010; 17:2963–2969. PMID:
20552403.

41. Sippel RS, Becker YT, Odorico JS, Springman SR, Chen H. Does propofol anesthesia affect intraoperative parathyroid hormone levels? A randomized, prospective trial. Surgery. 2004; 136:1138–1142. PMID:
15657568.

42. Woodrum DT, Saunders BD, England BG, Burney RE, Doherty GM, Gauger PG. The influence of sample site on intraoperative PTH monitoring during parathyroidectomy. Surgery. 2004; 136:1169–1175. PMID:
15657572.

43. Beyer TD, Chen E, Ata A, DeCresce R, Prinz RA, Solorzano CC. A prospective evaluation of the effect of sample collection site on intraoperative parathormone monitoring during parathyroidectomy. Surgery. 2008; 144:504–509. PMID:
18847632.

44. Yang GP, Levine S, Weigel RJ. A spike in parathyroid hormone during neck exploration may cause a false-negative intraoperative assay result. Arch Surg. 2001; 136:945–949. PMID:
11485536.

45. Teo R, Farra JC, Khan ZF, Marcadis AR, Lew JI. Intraoperative parathormone spikes during parathyroidectomy may be associated with multiglandular disease. Surgery. 2018; 163:393–396. PMID:
29174058.

46. Westerdahl J, Bergenfelz A. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: five-year follow-up of a randomized controlled trial. Ann Surg. 2007; 246:976–980. PMID:
18043099.
47. Bergenfelz AO, Jansson SK, Wallin GK, Martensson HG, Rasmussen L, Eriksson HL, et al. Impact of modern techniques on short-term outcome after surgery for primary hyperparathyroidism: a multicenter study comprising 2,708 patients. Langenbecks Arch Surg. 2009; 394:851–860. PMID:
19618204.

48. Chen H, Sokoll LJ, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery. 1999; 126:1016–1021. PMID:
10598182.

49. Fahy BN, Bold RJ, Beckett L, Schneider PD. Modern parathyroid surgery: a cost-benefit analysis of localizing strategies. Arch Surg. 2002; 137:917–922. PMID:
12146990.
50. Lew JI, Solorzano CC, Montano RE, Carneiro-Pla DM, Irvin GL 3rd. Role of intraoperative parathormone monitoring during parathyroidectomy in patients with discordant localization studies. Surgery. 2008; 144:299–306. PMID:
18656639.

51. Lew JI, Rivera M, Irvin GL 3rd, Solorzano CC. Operative failure in the era of focused parathyroidectomy: a contemporary series of 845 patients. Arch Surg. 2010; 145:628–633. PMID:
20644124.
52. Bergenfelz AO, Hellman P, Harrison B, Sitges-Serra A, Dralle H. European Society of Endocrine Surgeons. Positional statement of the European Society of Endocrine Surgeons (ESES) on modern techniques in pHPT surgery. Langenbecks Arch Surg. 2009; 394:761–764. PMID:
19575214.

53. Bergenfelz AO, Wallin G, Jansson S, Eriksson H, Martensson H, Christiansen P, et al. Results of surgery for sporadic primary hyperparathyroidism in patients with preoperatively negative sestamibi scintigraphy and ultrasound. Langenbecks Arch Surg. 2011; 396:83–90. PMID:
21061130.

54. Lee NC, Norton JA. Multiple-gland disease in primary hyperparathyroidism: a function of operative approach? Arch Surg. 2002; 137:896–899. PMID:
12146987.

55. Haciyanli M, Lal G, Morita E, Duh QY, Kebebew E, Clark OH. Accuracy of preoperative localization studies and intraoperative parathyroid hormone assay in patients with primary hyperparathyroidism and double adenoma. J Am Coll Surg. 2003; 197:739–746. PMID:
14585407.

56. Clerici T, Brandle M, Lange J, Doherty GM, Gauger PG. Impact of intraoperative parathyroid hormone monitoring on the prediction of multiglandular parathyroid disease. World J Surg. 2004; 28:187–192. PMID:
14708048.

57. Siperstein A, Berber E, Barbosa GF, Tsinberg M, Greene AB, Mitchell J, et al. Predicting the success of limited exploration for primary hyperparathyroidism using ultrasound, sestamibi, and intraoperative parathyroid hormone: analysis of 1158 cases. Ann Surg. 2008; 248:420–428. PMID:
18791362.
58. Westerdahl J, Bergenfelz A. Sestamibi scan-directed parathyroid surgery: potentially high failure rate without measurement of intraoperative parathyroid hormone. World J Surg. 2004; 28:1132–1138. PMID:
15490068.

59. McGill J, Sturgeon C, Kaplan SP, Chiu B, Kaplan EL, Angelos P. How does the operative strategy for primary hyperparathyroidism impact the findings and cure rate? A comparison of 800 parathyroidectomies. J Am Coll Surg. 2008; 207:246–249. PMID:
18656054.

60. Carneiro-Pla DM, Solorzano CC, Lew JI, Irvin GL 3rd. Long-term outcome of patients with intraoperative parathyroid level remaining above the normal range during parathyroidectomy. Surgery. 2008; 144:989–993. PMID:
19041008.

61. Schneider DF, Mazeh H, Chen H, Sippel RS. Predictors of recurrence in primary hyperparathyroidism: an analysis of 1386 cases. Ann Surg. 2014; 259:563–568. PMID:
24263316.
62. Wharry LI, Yip L, Armstrong MJ, Virji MA, Stang MT, Carty SE, et al. The final intraoperative parathyroid hormone level: how low should it go? World J Surg. 2014; 38:558–563. PMID:
24253106.

63. Taylor J, Fraser W, Banaszkiewicz P, Drury P, Atkins P. Lateralization of parathyroid adenomas by intra-operative parathormone estimation. J R Coll Surg Edinb. 1996; 41:174–177. PMID:
8763181.
64. Udelsman R, Osterman F, Sokoll LJ, Drew H, Levine MA, Chan DW. Rapid parathyroid hormone measurement during venous localization. Clin Chim Acta. 2000; 295:193–198. PMID:
10767405.

65. Ito F, Sippel R, Lederman J, Chen H. The utility of intraoperative bilateral internal jugular venous sampling with rapid parathyroid hormone testing. Ann Surg. 2007; 245:959–963. PMID:
17522522.

66. Perrier ND, Ituarte P, Kikuchi S, Siperstein AE, Duh QY, Clark OH, et al. Intraoperative parathyroid aspiration and parathyroid hormone assay as an alternative to frozen section for tissue identification. World J Surg. 2000; 24:1319–1322. PMID:
11038200.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download