This article has been
cited by other articles in ScienceCentral.
Transoral endoscopic thyroid surgery is known to be an innovative, effective and safe procedure, which is offered as a scarless technique to strongly motivated patients who want to obtain a good aesthetic result. However, evaluating the complications of this procedure, what we know is that only a few of these are related to thyroid surgery (bleeding, permanent or transient hypocalcemia, recurrent laryngeal nerve injury, seroma, surgical site infection) since more than 70% are specific of the transoral endoscopic technique such as: zygomatic bruising, chin flap perforation, oral commissure tearing, dimpling on the chin and mental nerve (MN) injury (
1). The main cause of their occurrence is the placement of the trocars. Due to the fact that transoral endoscopic thyroidectomy with vestibular approach (TOETVA) is carried out through a 3-port technique placed at the oral vestibule, the incisions that are currently performed are one central of 10 millimeters (optical port for 30° endoscope) and 2 lateral of 5 millimeters (working ports for dissecting and coagulating instruments) (
2). The central one is performed 1 cm above the inferior labial frenulum, meanwhile the laterals are performed in correspondence of the mental foramina (MFs), parallel to the first incision. After cutting mucosa and submucosa, we move on to the dissection of a flap, with a curved Kelly clamp, up to the lower edge of the mandible. The flap is set up along a plane that runs at the same level as the mental nerve, and its branches, and it will allow the insertion and passage of the trocars. It is clear that during this maneuver there are 2 main risks: 1) perforation of the chin flap; 2) MN injury. Therefore the precise location of the nerve is important in this type of surgery and its injury should be avoided.
The MN is one of the branches of the inferior alveolar nerve, branch of the mandibular nerve. The mandibular nerve is the third branch of the trigeminal nerve (fifth cranial nerve), a mixed nerve consisting of somatic efferent (motor) and somatic afferent (sensory) fibers (
Fig. 1). The afferent fibers of the mandibular nerve innervate several skin areas of the face, the oral mucosa, the lower teeth and gums. Instead, the motor branches supply muscles of the first branchial arch, including the masticatory muscles. The mandibular nerve emerges from the lateral part of the trigeminal ganglion and exits the middle cranial fossa via the foramen ovale, which is anterior to the foramen spinosum (
3). After coming out of the foramen ovale, it splits into 2 large trunks, anterior and posterior: 1) the anterior trunk is a predominantly motor nerve and gives rise to the masseteric branch, pterygoid medial nerve, deep temporal nerve, and buccal nerve; 2) the posterior or posteromedial trunk is mainly sensitive nerve, it breaks down into the auriculo-temporal nerve and lingual nerve, and the inferior alveolar nerve. The inferior alveolar nerve has only-sensitive fibers that traverse the mandibular canal to exit via the MF (
Fig. 2). Through this foramen, the MN exits, it supplies sensation to the skin and buccal mucosa of the lip and the skin of the chin (
Fig. 3). In particular sensory innervation of the MN may have some overlap with the contralateral once. The sensory innervation of the MN divides among 3 smaller branches. One of the branches from the MN will innervate the skin on the chin. The other 2 nerves provide sensory innervation to the gingivae, the mucosa, and the lower lip (
Fig. 3). The MN is also linked to the branches of the facial nerve (
4). The MF is commonly located halfway between the upper alveolar crest and the lower edge of the mandibular bone, in direct line with the second premolar. As already mentioned, on a vertical plane, the foramen has been found above, at, or below the apex of the premolars. Most commonly, it lies below the midpoint of the distance between the lower border of the mandible and the alveolar margin. In the horizontal plane, it is one quarter of the distance from the mental symphysis to the posterior border of the ramus of the mandible (
5) (
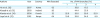
Fig. 4). However exact MF location can be variable. According to the literature research in a very small percentage of people, the MN origin can be the first molar or the first premolar (
Table 1) (
6789). Moreover, in older or edentulous individuals, there is alveolar bone resorption which makes the location of the MF closer to the alveolar crest in most of the patients. The variations are obviously influenced by gender, age, race. In a study carried out on 525 dry mandibles, Gershenson et al. (
10) reported that 4.3% of the mandibles had double MFs, 0.7% had triple MFs and that one mandible had 4 MFs on one side. Besides, the branching of the MN may vary slightly. In some individuals, there may be more branches that come from the MN. So the various foramina lead to variations in the branches of the exiting MN. Even with the differences in the branching of the MN, the sensory territory is consistent (
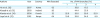
11). Most common pattern is bifurcation (about 40%) followed by trifurcation (30%), single (20%), and quadrification (<10%) (
Table 2) (
12131415).
The above description of the anatomy of the MN is of remarkable importance for the surgeon performing a TOETVA. To improve the quality of TOETVA and prevent MN damage, accurate intraoperative anatomical orientation of MN is essential (
16). Vestibular incisions must be made in safe areas to minimize the risk of MN involvement, which would lead to dysesthesias in the areas innervated by the MN. The current incisions are performed according to the projections of the branches of the MN and of the MF on the vestibular mucosa. But the dissection of the MN on cadaver model allowed to highlight the course of the MN and its ramifications (
17). Zhang et al. (
17) pointed out that the MN has a medial curvilinear course and MN soon branches out. So a triangular safety zone has been identified and the surgeon should consider that 1) a high median incision can damage the medial branches of the MN; 2) extending the median incision laterally, the MN injury can occur bilaterally; 3) a 1 cm high median incision, or a more inferiorly positioned median one, or a perpendicular opening may better preserve the MN. Instead, the 2 lateral 5 mm incisions are made at the most lateral-anterior aspect of the oral commissure in the mucosal border to avoid MN injury and instrument collision (
Fig. 5) (
18).
Transoral thyroid surgery represents the latest technological advancement in the approach to minimally invasive endocrine surgery. However, it is clear that conventional open thyroid surgery will still be performed. TOETVA advantages have been speculated and demonstrated in prospective studies, but so far, these procedures are still limited to a minority of patients. Several critical issues, including the MN injury and overall safety of the transoral approach and whether it will provide significant patient benefit in postoperative outcomes compared with open surgery and other endoscopic procedures, must be resolved before the new technique is successfully and responsibly introduced in clinical care. Additionally, it is recognised that the early use of this approach by surgeons, who might be relatively inexperienced in the particular skill sets required, might lead to new or serious complications, which should definitely be avoided during the start of this concept. Finally, TOETVA should provide all the advantages of other endoscopic surgeries and natural orifice transluminal endoscopic surgery (NOTES) concept. Certainly, there are significant differences between TOETVA and the other NOTES approaches (transgastric appendectomy, transvaginal cholecystectomy, cancer staging, percutaneous endoscopic gastrostomy salvage). Wound infection, incisional hernias and postoperative adhesions in abdominal surgery are common surgical complications and are eliminated with NOTES. However, these sequelae rarely belong to thyroid surgery. The advantages of NOTES for thyroid gland incision might still be less impressive than those in abdominal surgery.
Figures and Tables
Fig. 1
MN is a branch of the posterior trunk of the inferior alveolar nerve, which is itself a branch of the mandibular division of the trigeminal nerve. The MN emerges at the mental foramen in the mandible, and divides beneath the depressor anguli oris muscle into 3 branches: one descends to the skin of the chin, 2 ascend to the skin and mucous membrane of the lower lip. These branches communicate freely with the facial nerve.
MN = mental nerve.
Fig. 2
The mental foramen may be oval or round and is usually located apical to the second mandibular premolar or between apices of the premolars. However, its location can vary from the mandibular canine to the first molar. Very few variants of this nerve have been described in literature.

Fig. 3
mental nerve is a sensory nerve which provides sensation to the front of the chin and lower lip as well as the labial gingivae of the mandibular anterior teeth and the premolars.

Fig. 4
Landmarks for MN identification. (A) MN origin and foramen is 2 cm below the ipsilateral labial commissure, a finger nail above the jaw; (B) the nerve is 2.5 cm lateral to an imaginary median line of the face; (C) in the intra-oral perspective, the MN originates between the 3rd and 4th tooth.
MN = mental nerve.

Fig. 5
The dissection of the MN on cadaver allowed to highlight the course of the MN and its ramifications. The MN has a medial curvilinear course. MN soon branches out. The areas highlighted in green are zones with absence or less concentration of peripheral branches of the MN. A vestibular incision in these areas appears to be safe and prevents MN injury. Conventionally, the central incision is 1–2 cm in length and is placed beyond the cranial aspect of the buccal-mandibular frenulum, while 2 lateral 5 mm incisions are made at the most lateral-anterior aspect of the oral commissure in the mucosal border to avoid MN injury and instrument collision. It should be noted that a too inferior median incision, too close to the gingiva (red area) can interfere with the endoscopic instruments and furthermore create adhesions/sinechie with the gingival sulcus or lesion of the inferior labial frenulum.
MN = mental nerve.
*MN branches.

Table 1
MN origin/foramen location according to literature research

|
Authors |
Year |
Country |
Side |
MN origin/foramen location (%) |
|
I |
II |
III |
IV |
V |
VI |
|
Agarwal and Gupta (6) |
2012 |
India |
Rt. |
0 |
0 |
7.8 |
81.5 |
2.7 |
7.9 |
|
Lt. |
0 |
0 |
7.6 |
81.5 |
3.1 |
7.8 |
|
Amorim et al. (7) |
2008 |
Brazil |
Rt. |
0 |
0 |
19.8 |
71.4 |
8.8 |
0 |
|
Lt. |
0 |
0 |
23.1 |
68.1 |
8.8 |
0 |
|
Yeşilyurt et al. (8) |
2008 |
Turkey |
Rt. |
0 |
5.7 |
34.3 |
55.7 |
4.3 |
0 |
|
Lt. |
0 |
7.1 |
25.7 |
61.4 |
5.7 |
0 |
|
Budhiraja et al. (9) |
2013 |
India |
Rt. |
0 |
3.8 |
20.0 |
61.0 |
14.3 |
0.9 |
|
Lt. |
0 |
2.9 |
20.9 |
59.1 |
15.2 |
1.9 |
Table 2
Prevalence of the different branching patterns of the MN in different populations
|
Authors |
Year |
Country |
MN dissected |
No. of MN branches (%) |
|
1 |
2 |
3 |
4 |
|
Hu et al. (12) |
2007 |
Korea |
62 |
- |
38.8 |
61.3 |
- |
|
Alsaad et al. (13) |
2003 |
Ireland |
26 |
- |
44.4 |
55.6 |
- |
|
Alantar et al. (14) |
2000 |
French |
32 |
22.0 |
28.0 |
28.0 |
22.0 |
|
Loyal et al. (15) |
2012 |
Kenya |
64 |
19.0 |
39.0 |
34.0 |
8.0 |









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download