INTRODUCTION
During the last decade, a dramatic increase in the incidence of thyroid malignancy resulted in an increased demand for thyroid surgery. Several energy devices were invented and widely adopted in surgical fields with a hemostatic purpose. Many surgeons use them to supplement electric cautery (e.g., Bovie) and ligature. The excellent coagulation decreased the operative time and incidence of postoperative hematoma. Harmonic and Ligasure are well-known devices not only for thyroid surgery but also for abdominal surgery. However, they are based on a different energy delivery system in that Harmonic and Ligasure use ultrasonic and bipolar energy for coagulation and cutting function, respectively.
Because thyroid is a richly vascularized organ, appropriate vessel ligation and sealing are important during thyroidectomy. In addition, adequate visualization of recurrent laryngeal nerves (RLNs) by reducing the frequency of subtle but annoying bleeding and simultaneously avoiding thermal injury by energy devices along the nerve trajectory, is critical to prevent postoperative voice morbidity. Preservation of parathyroid glands is one of the longstanding imperatives. Because parathyroid glands are supplied by a tiny end-artery, preservation of parathyroid gland without thermal injury can be a challenge.
A recently developed energy device, Thunderbeat, uses the combined functions of both ultrasonic scalpel and bipolar sealer. Studies reported a shorter operation time with Thunderbeat in abdomino-pelvic surgery (
12). Several studies compared hemostatic energy-based devices, such as Harmonic and Ligasure, and conventional clamp and tie techniques for thyroidectomy. To the best of our knowledge, no prospective head-to-head comparison of the 3 energy devices has been conducted until now, which facilitated the selection of devices.
We designed this single-blind, prospective, randomized controlled study to analyze the safety and feasibility of each energy device in thyroid surgery.
MATERIALS AND METHODS
1. Patient selection
This single-blind, prospective, randomized clinical trial was performed from July 2016 to November 2016 at the Department of Endocrine Surgery, Samsung Medical Center by a single experienced surgeon. We obtained the approval of the Institutional Review Board (SMC 2016-02-049) before the patients were recruited and their informed consent was obtained by certified doctors.
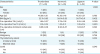
Inclusion criteria were conventional open thyroidectomy in patients aged between 20 and 70 years. The thyroid tumor was either benign or malignant but limited to 4 cm with no evidence of lymph node metastasis, i.e., clinical T1–2 no stage, in pre-operative radiological images (thyroid ultrasonography or thyroid computed tomography).
Patients with the following features were excluded from the study: 1) age <20 years or >70 years, 2) thyroid tumor size >4 cm, 3) suspicious extrathyroidal invasion either in pre-operative radiological or intra-operative findings, 4) clinically evident lymph node (central or lateral) metastasis or distant metastasis in pre-operative radiological images, 5) associated severe comorbidities (e.g., severe cardiovascular, pulmonary, kidney, liver disease, or psychological problem), 6) previous history of thyroid surgery or neck irradiation, 7) thyroid parenchymal disease such as Graves' disease or Hashimoto's thyroiditis, and 8) patients who did not agree to this clinical trial. Patients meeting the eligibility criteria were randomly allocated to one of the 3 groups according to energy device: Harmonic (H group), Ligasure (L group), and Thunderbeat (T group).
2. Study design
This study was designed to evaluate the safety and efficacy of using Thunderbeat Open Fine Jaw (Olympus, Tokyo, Japan; Thunderbeat) compared with Harmonic Focus Plus (Ethicon, Somerset, NJ, USA; ultrasonic scalpel; Harmonic) and Ligasure Small Jaw (Covidien, Dublin, Ireland; bipolar sealer; Ligasure) in conventional open thyroidectomy.
We formulated 2 hypotheses in this clinical trial. First, Thunderbeat entails shorter operation time compared with Harmonic and Ligasure. Because Thunderbeat has 3 functions—sealing, cutting, dissection—at the same time, and shorter and faster cutting time and dissection speed than Harmonic or Ligasure, the operative time is shortened (
3). Second, Thunderbeat is not inferior to Harmonic and Ligasure in terms of surgical morbidities. Heat production by the devices and its lateral spread might affect nerve or parathyroid injury similarly (
23).
3. Surgical strategy
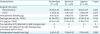
The extent of thyroid surgery is based on 2015 American Thyroid Association Guidelines. We performed unilateral total thyroidectomy in cases of benign disease or malignant tumor <4 cm without extrathyroidal extension. We performed bilateral total thyroidectomy for bilateral tumors. In our institution, we conducted prophylactic central lymph node (CLN) dissection (CLND) in cases of malignancy. When CLN metastasis was confirmed by frozen biopsy (lymph node metastasis with ≥6 lymph nodes or >2 mm in diameter), surgical option was extended to bilateral total thyroidectomy. We divided ‘operative time’ into 2 components: ‘thyroidectomy time’ between midline incision of linear alba and removal of unilateral thyroid gland; and ‘CLND time’ covering the duration between start of CLND and complete excision of CLN. Thyroidectomies were performed by a single surgeon who is expert in endocrine surgery and had much experience in using energy devices.
4. Evaluation of surgical outcomes
Surgical specimens were microscopically examined by 2 or more experienced pathologists. The following histopathological parameters were assessed: cell type of the main lesion, primary tumor size (longest diameter of the largest lesion), location, multifocality, bilaterality, extrathyroidal extension, lymphovascular invasion, margin involvement, regional LN metastasis, and underlying thyroid conditions, such as chronic lymphocytic thyroiditis. Multifocality was defined by 2 or more lesions of conventional papillary thyroid carcinoma in one lobe, regardless of bilaterality. Notably, histopathology results of LN status were reported on a “per level” basis and were indicated by surgeons during operation. Thyroid cancer staging was determined in accordance with the American Joint Committee on Cancer recommendations (
4).
5. Statistical analysis
We assumed type I error, statistical power and dropout rates as 0.05%, 90%, and 10%, respectively, and assigned the experimental and the control groups on a one-to-one correspondence. The target number of subjects in this study included a total of 75 patients, with 25 patients in each group. We considered patients' sex as a confounding factor, and used a stratified randomly permuted block design according to a male-to-female ratio of 1:4.
We generated the random allocation sequence based on online calculations (
http://www.randomization.com). To maintain confidentiality of randomization and blindness of allocation, we only exposed information about grouping to the medical personnel including the surgeon on the day of the operation.
The results of continuous variables were presented as mean±standard deviation, and categorical variables were presented as percentages. Statistical significance among the 3 groups was analyzed by using one-way analysis of variance and Kruskal-Wallis test for continuous variables and χ2 test for categorical variables. All statistical tests were 2-sided, and P<0.05 was considered statistically significant.
DISCUSSION
Use of energy-based devices for thyroid surgery is recognized as safe and effective and is associated with intraoperative advantages, post-operative outcomes and cost-effectiveness (
56789). The challenge is to decide the device that is appropriate under the specific circumstances, and the choice is based on the surgeon's preference or experience. The study findings should provide additional guidance.
Several reports have compared the hemostatic methods including Harmonic, Ligasure, Thunderbeat, and conventional clamp-and-tie devices. Most often, the clinical studies comparing the energy devices in thyroid surgery focused on 3 issues: first, intraoperative hemostasis and postoperative hematoma or bleeding; second, postoperative complication, in terms of RLN injury and hypocalcemia due to parathyroid dysfunction or sacrifice; and third, the speed and cost-effectiveness based on operation time and duration of facility usage.
A meta-analysis (
6) revealed that Harmonic yielded superior intraoperative (operation time, and blood loss) and postoperative outcomes (hypoparathyroidism, drain output, neck collection, and length and cost of hospital stay) compared with Ligasure or the classic clamp-and-tie technique. However, it may be associated with the risk of RLN paralysis. The use of Ligasure was associated with the lowest complication.
However, according to a prospective, randomized, controlled trial by Kwak et al. (
10), Harmonic and Ligasure did not differ in operative time, postoperative transient hypoparathyroidism, or permanent RLN injury, and were equally effective in open thyroidectomy.
Another prospective randomized study (
11) comparing different energy-based devices such as Harmonic and Ligasure also revealed no significant difference in intraoperative and postoperative outcomes.
A retrospective, non-inferiority study (
12) showed that Thunderbeat was comparable to Harmonic in terms of intraoperative outcomes (duration of surgery, and blood loss) and postoperative complications (hypocalcemia, and RLN paralysis). Despite evidence derived from published studies on the effectiveness of energy-based devices, no clear guidance is available for the selection of hemostatic devices. Although each device is based on a different energy mechanism, several studies reported few differences in operative outcomes with no obvious or consistent benefit shown by one energy source compared with the others. Because safety of devices was already established by clinical and laboratory studies, the selection of an energy-based device for therapeutic application is a challenge.
We performed a literature review to analyze the properties and clinical benefits of each energy-based device. Several animal models were used to study the properties of devices. Seehofer et al. (
3) designed a pig model to compare Thunderbeat with Harmonic and Ligasure via surgical procedures using abdominal and limb vessels. The maximal burst pressure of Thunderbeat was higher than that of Harmonic and was the highest among the 3 devices. Arterial cutting time was rapid with Thunderbeat and statistically significant compared with the other 2 devices. The maximum temperature of Thunderbeat and Harmonic was comparable and significantly higher than that of Ligasure. However, Ligasure revealed the largest tissue sealing width among the 3 devices.
Smith et al. (
13) performed procedures to divide thyroid parenchyma using a porcine model with ultrasonic device (UD) and electronic vessel sealing (EVS). The UD reached higher maximum temperature than EVS, but the lateral thermal spread of the 2 devices was comparable and not significantly different. The maximum temperature and lateral thermal spread of the devices were important factors contributing to the surgical outcomes without damage to the adjacent tissue.
In the porcine study (
14), the thyroid and perithyroidal tissues were transected with energy devices. A distance of more than 2 mm between the jaw of each device and the RLN suggested the absence of RLN injury. The findings showed that a specific distance was needed to prevent the lateral thermal spread and associated nerve damage in 3 energy devices (Ligasure, Harmonic, and Thunderbeat).
The amplitudes and latencies of RLN were analyzed during thyroidectomy of piglets with continuous intraoperative neuromonitoring (
15). When the distance of Thunderbeat was greater than 3 mm from the nerve, there was no obvious change in safety parameter. However, at a device distance of less than 1 mm from the nerve, immediate loss of signal was observed. Time was a critical parameter for distances shorter than 2 mm. When the activation duration exceeded 8 seconds, about 50% of signal variation was detected.
Based on these results and other reported studies, the merits and demerits of the 3 energy-based devices can be summarized as follows.
Harmonic uses energy based on mechanical vibrations, which generate frictional heat via high-frequency ultrasonic energy. This device seals the vessels and the perithyroidal tissue but facilitates surgical resection with relatively low peak temperatures and less lateral thermal spread.
Under prolonged activation (>8 seconds), the peak temperature was increased by more than 100°C, and when the distance from the crucial structure was less than 2 mm, the lateral heat spread affected the surrounding tissues (
Supplementary Table 1) (
13). It may trigger tissue damage to the unintended areas such as the vasculature of the parathyroid glands or RLN (
11). Furthermore, Harmonic failed to seal large vessels (
3).
Ligasure uses electrically generated bipolar energy by directly contacting the tissue and raising the peak temperature, resulting in vessel sealing up to 7 mm in diameter with a relatively low maximal temperature compared with other devices (
313). However, because Ligasure shows the widest sealing length and the longest average cutting time, it is not intended for sharp and sophisticated performance (
2).
Thunderbeat utilizes both ultrasonically generated frictional energy and electrically generated bipolar energy. This device performs sealing, cutting, and dissecting functions simultaneously and shows the highest versatility. It also saves the operation time according to many studies.
However, the device has both advantages and limitations. The potential lateral spread of thermal energy by friction and the high peak temperature is inevitably associated with high speeds of cutting and dissection. Thunderbeat also has a relatively large and blunt cutting blade compared with Harmonic focus, and therefore, it is not indicated for fine dissection unlike Harmonic blade tip during thyroid surgery. A thin blade is essential for dissection. In addition, the thermal control system should be updated to minimize the thermal damage.
The 2 cases of VCP in the Thunderbeat group of this study may be associated with the nature of the device, i.e., high maximal temperature, and the relative inexperience in usage of the new device compared with other devices. Transient RLN palsy caused by ‘Thunderbeat’ were detected in first 2 consecutive patients. VCP that was not significantly different between the 3 groups was reported during the initial phase of this study.
A study investigating the objective and subjective voice outcomes after thyroidectomy using energy-based devices (
16) showed voice alterations with or without VCP. In our study, we evaluated only objective findings with perioperative laryngoscopy. We did not investigate subjective dysfunction, and therefore, it is possible that voice dysfunction might occur even in the absence of VCP.
The duration of thyroidectomy (from midline incision to removal of thyroid) was significantly shorter in the Thunderbeat group. In contrast, CLND was faster with Harmonic compared with Thunderbeat, suggesting that Thunderbeat shortened surgical time via simultaneous action of dissection, sealing, and cutting during thyroidectomy. Harmonic facilitates sealing and cutting at the same time, which is less when the dissection field is smaller than in thyroidectomy, such as CLND. Our findings, were consistent with other recent studies comparing Harmonic and Thunderbeat (
12): thyroidectomy time was shorter with Thunderbeat compared with Harmonic, but the lymph node dissection time was not significantly different between the 2 groups.
This study has several limitations, potential bias, and confounding factors. Even if a surgeon was fully aware of the new energy device, its limited usage compared with the other devices may result in discrepancy in proficiency. It can be considered as source of potential bias.
We allocated the patients evenly and stratified by considering sex as a confounding factor; however, a few clinical characteristics were not matched among the 3 groups.
In the T group, a patient manifested subclinical hyperthyroidism with a pre-operative TSH level of 0.01 mIU/L and a free T4 level of 2.16 mIU/L. Although the mean free T4 level was not significantly different among the 3 groups, the mean TSH level was evidently lower in the T group. Subclinical hyperthyroidism might affect the hemostatic procedure due to the bleeding risk and the long operation time, damage to the parathyroid function, and injury to the RLN. However, in this study, thyroidectomy time was faster in the T group, and postoperative complications were comparable among the 3 groups.
Although other basic clinical characteristics including causes of operation, extent of thyroidectomy, and CLND were not significantly different among the 3 groups, the results might be influenced by uncontrolled confounding factors.
In spite of limitations, this study has several strengths. As far as we know, this study is the first randomized controlled trial comparing 3 energy devices for thyroid surgery. Second, even though each device was used in different patients, the surgical procedures were performed by a single experienced surgeon. We may disregard the interpersonal differences in surgical technique and the learning curve of the surgeon.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download