1. Kim MK, Kim T, Moon HG, Jin US, Kim K, Kim J, et al. Effect of cosmetic outcome on quality of life after breast cancer surgery. Eur J Surg Oncol. 2015; 41(3):426–432.
2. Kolyadina IV, Poddubnaya IV, Frank GA, Komov DV, Karseladze AI, Ermilova VD, et al. Stage I breast cancer heterogeneity: biological and predictive value. Malig Tumour. 2015; (1):35.
3. De Angelis C, Di Maio M, Crispo A, Giuliano M, Schettini F, Bonotto M, et al. Luminal-like HER2-negative stage IA breast cancer: a multicenter retrospective study on long-term outcome with propensity score analysis. Oncotarget. 2017; 8(68):112816–112824.
4. Esbah O, Oksuzoglu B. Prognostic & predictive factors for planning adjuvant chemotherapy of early-stage breast cancer. Indian J Med Res. 2017; 146(5):563–571.
5. Vieira AF, Schmitt F. An update on breast cancer multigene prognostic tests-emergent clinical biomarkers. Front Med (Lausanne). 2018; 5:248.
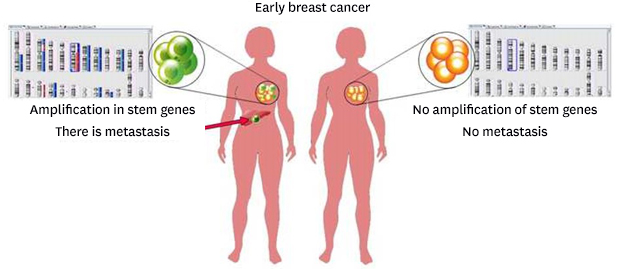
6. Litviakov N, Ibragimova M, Slonimskaya E, Skurikhin E, Tsyganov M, Pershina O, et al. Somatic-stem transition of tumor cells is a key link in the metastasis. Ann Oncol. 2018; 8:Suppl 8. 682–682.
7. Ibragimova MK, Tsyganov MM, Litviakov NV. Natural and chemotherapy-induced clonal evolution of tumors. Biochemistry (Mosc). 2017; 82(4):413–425.
8. Hyman E, Kauraniemi P, Hautaniemi S, Wolf M, Mousses S, Rozenblum E, et al. Impact of DNA amplification on gene expression patterns in breast cancer. Cancer Res. 2002; 62(21):6240–6245.
9. Houvenaeghel G, Goncalves A, Classe JM, Garbay JR, Giard S, Charytensky H, et al. Characteristics and clinical outcome of T1 breast cancer: a multicenter retrospective cohort study. Ann Oncol. 2014; 25(3):623–628.
10. Theriault RL, Litton JK, Mittendorf EA, Chen H, Meric-Bernstam F, Chavez-Macgregor M, et al. Age and survival estimates in patients who have node-negative T1ab breast cancer by breast cancer subtype. Clin Breast Cancer. 2011; 11(5):325–331.
11. Cancello G, Maisonneuve P, Rotmensz N, Viale G, Mastropasqua MG, Pruneri G, et al. Prognosis in women with small (T1mic,T1a,T1b) node-negative operable breast cancer by immunohistochemically selected subtypes. Breast Cancer Res Treat. 2011; 127(3):713–720.
12. Fisher B, Dignam J, Bryant J, Wolmark N. Five versus more than five years of tamoxifen for lymph node-negative breast cancer: updated findings from the National Surgical Adjuvant Breast and Bowel Project B-14 randomized trial. J Natl Cancer Inst. 2001; 93(9):684–690.
13. Foekens JA, Atkins D, Zhang Y, Sweep FC, Harbeck N, Paradiso A, et al. Multicenter validation of a gene expression-based prognostic signature in lymph node-negative primary breast cancer. J Clin Oncol. 2006; 24(11):1665–1671.
14. DePinho RA. The age of cancer. Nature. 2000; 408(6809):248–254.
15. Azim HA Jr, Nguyen B, Brohée S, Zoppoli G, Sotiriou C. Genomic aberrations in young and elderly breast cancer patients. BMC Med. 2015; 13(1):266.
16. Brown SB, Hankinson SE. Endogenous estrogens and the risk of breast, endometrial, and ovarian cancers. Steroids. 2015; 99(Pt A):8–10.
17. Kwon YW, Ahn HS, Park JY, Yang HM, Cho HJ, Kim HS. Imprinted gene Zinc finger protein 127 is a novel regulator of master pluripotency transcription factor, Oct4. BMB Rep. 2018; 51(5):242–248.
18. Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006; 126(4):663–676.
19. Cai S, Geng S, Jin F, Liu J, Qu C, Chen B. POU5F1/Oct-4 expression in breast cancer tissue is significantly associated with non-sentinel lymph node metastasis. BMC Cancer. 2016; 16(1):175.
20. Ma Y, Fei L, Zhang M, Zhang W, Liu X, Wang C, et al. Lamin B2 binding to minichromosome maintenance complex component 7 promotes non-small cell lung carcinogenesis. Oncotarget. 2017; 8(62):104813–104830.
21. Wang LN, Gao MH, Wang B, Cong BB, Zhang SC. A role for GPI-CD59 in promoting T-cell signal transduction via LAT. Oncol Lett. 2018; 15(4):4873–4881.
22. Youn HJ, Jung SH. Overexpression of the Bmi-1 oncoprotein correlates with axillary lymph node metastases in invasive ductal breast cancer. J Breast Cancer. 2005; 8(2):17–22.
23. Kim EA, Kim YH, Kang HW, Yoon HY, Kim WT, Kim YJ, et al. Lower levels of human MOB3B are associated with prostate cancer susceptibility and aggressive Clinicopathological characteristics. J Korean Med Sci. 2015; 30(7):937–942.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download