1. Lewis MA, Pascoal A, Keevil SF, Lewis CA. Selecting a CT scanner for cardiac imaging: the heart of the matter. Br J Radiol. 2016; 89:20160376. PMID:
27302494.

2. Lawler LP, Pannu HK, Fishman EK. MDCT evaluation of the coronary arteries, 2004: how we do it--data acquisition, postprocessing, display, and interpretation. AJR Am J Roentgenol. 2005; 184:1402–1412. PMID:
15855087.

3. Mori S, Endo M, Obata T, Murase K, Fujiwara H, Susumu K, et al. Clinical potentials of the prototype 256-detector row CT-scanner. Acad Radiol. 2005; 12:148–154. PMID:
15721591.
4. Mori S, Kondo C, Suzuki N, Yamashita H, Hattori A, Kusakabe M, et al. Volumetric cine imaging for cardiovascular circulation using prototype 256-detector row computed tomography scanner (4-dimensional computed tomography): a preliminary study with a porcine model. J Comput Assist Tomogr. 2005; 29:26–30. PMID:
15665678.
5. Mori S, Endo M, Obata T, Tsunoo T, Susumu K, Tanada S. Properties of the prototype 256-row (cone beam) CT scanner. Eur Radiol. 2006; 16:2100–2108. PMID:
16568264.

6. Raju R, Cury RC, Precious B, Blanke P, Naoum C, Arepalli C, et al. Comparison of image quality, and diagnostic interpretability of a new volumetric high temporal resolution scanner versus 64-slice MDCT. Clin Imaging. 2016; 40:205–211. PMID:
26995571.

7. Latif MA, Sanchez FW, Sayegh K, Veledar E, Aziz M, Malik R, et al. Volumetric single-beat coronary computed tomography angiography: relationship of image quality, heart rate, and body mass index. Initial patient experience with a new computed tomography scanner. J Comput Assist Tomogr. 2016; 40:763–772. PMID:
27331931.
8. Morcos SK, Thomsen HS, Webb JAW. Contrast Media Safety Committee of the European Society of Urogenital Radiology (ESUR). Contrast-media-induced nephrotoxicity: a consensus report. Eur Radiol. 1999; 9:1602–1613. PMID:
10525875.

9. McDonald RJ, McDonald JS, Bida JP, Carter RE, Fleming CJ, Misra S, et al. Intravenous contrast material-induced nephropathy: causal or coincident phenomenon? Radiology. 2013; 267:106–118. PMID:
23360742.

10. McDonald JS, McDonald RJ, Carter RE, Katzberg RW, Kallmes DF, Williamson EE. Risk of intravenous contrast material-mediated acute kidney injury: a propensity score-matched study stratified by baseline-estimated glomerular filtration rate. Radiology. 2014; 271:65–73. PMID:
24475854.

11. Johnson PT, Pannu HK, Fishman EK. IV contrast infusion for coronary artery CT angiography: literature review and results of a nationwide survey. AJR Am J Roentgenol. 2009; 192:W214–W221. PMID:
19380526.

12. Wintersperger BJ, Nikolaou K. Basics of cardiac MDCT: techniques and contrast application. Eur Radiol. 2005; 15 Suppl 2:B2–B9. PMID:
15801051.
13. Kumamaru KK, Steigner ML, Soga S, Signorelli J, Bedayat A, Adams K, et al. Coronary enhancement for prospective ECG-gated single R-R axial 320-MDCT angiography: comparison of 60- and 80-mL iopamidol 370 injection. AJR Am J Roentgenol. 2011; 197:844–850. PMID:
21940571.

14. Hein PA, May J, Rogalla P, Butler C, Hamm B, Lembcke A. Feasibility of contrast material volume reduction in coronary artery imaging using 320-slice volume CT. Eur Radiol. 2010; 20:1337–1343. PMID:
20016900.

15. Kim R, Park EA, Lee W, Chung JW. Feasibility of 320-row area detector CT coronary angiography using 40 mL of contrast material: assessment of image quality and diagnostic accuracy. Eur Radiol. 2016; 26:3802–3810. PMID:
26905865.
16. Cademartiri F, Maffei E, Palumbo AA, Malagò R, La Grutta L, Meiijboom WB, et al. Influence of intra-coronary enhancement on diagnostic accuracy with 64-slice CT coronary angiography. Eur Radiol. 2008; 18:576–583. PMID:
17934740.

17. Cademartiri F, Mollet NR, Lemos PA, Saia F, Midiri M, de Feyter PJ, et al. Higher intracoronary attenuation improves diagnostic accuracy in MDCT coronary angiography. AJR Am J Roentgenol. 2006; 187:W430–W433. PMID:
16985117.

18. Fei X, Du X, Yang Q, Shen Y, Li P, Liao J, et al. 64-MDCT coronary angiography: phantom study of effects of vascular attenuation on detection of coronary stenosis. AJR Am J Roentgenol. 2008; 191:43–49. PMID:
18562723.

19. Benz DC, Gräni C, Hirt Moch B, Mikulicic F, Vontobel J, Fuchs TA, et al. A low-dose and an ultra-low-dose contrast agent protocol for coronary CT angiography in a clinical setting: quantitative and qualitative comparison to a standard dose protocol. Br J Radiol. 2017; 90:20160933. PMID:
28406318.

20. Tan SK, Yeong CH, Raja Aman RRA, Ng KH, Abdul Aziz YF, Chee KH, et al. Low tube voltage prospectively ECG-triggered coronary CT angiography: a systematic review of image quality and radiation dose. Br J Radiol. 2018; 91:20170874. PMID:
29493261.

21. Hsiao EM, Rybicki FJ, Steigner M. CT coronary angiography: 256-slice and 320-detector row scanners. Curr Cardiol Rep. 2010; 12:68–75. PMID:
20425186.

22. Rybicki FJ, Otero HJ, Steigner ML, Vorobiof G, Nallamshetty L, Mitsouras D, et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging. 2008; 24:535–546. PMID:
18368512.

23. Chen MY, Shanbhag SM, Arai AE. Submillisievert median radiation dose for coronary angiography with a secondgeneration 320-detector row CT scanner in 107 consecutive patients. Radiology. 2013; 267:76–85. PMID:
23340461.

24. Benz DC, Gräni C, Mikulicic F, Vontobel J, Fuchs TA, Possner M, et al. Adaptive statistical iterative reconstruction-V: impact on image quality in ultralow-dose coronary computed tomography angiography. J Comput Assist Tomogr. 2016; 40:958–963. PMID:
27560012.
25. Richards CE, Dorman S, John P, Davies A, Evans S, Ninan T, et al. Low-radiation and high image quality coronary computed tomography angiography in “real-world” unselected patients. World J Radiol. 2018; 10:135–142. PMID:
30386498.

26. Kalisz K, Buethe J, Saboo SS, Abbara S, Halliburton S, Rajiah P. Artifacts at cardiac CT: physics and solutions. Radiographics. 2016; 36:2064–2083. PMID:
27768543.

27. Leipsic J, Labounty TM, Hague CJ, Mancini GBJ, O'Brien JM, Wood DA, et al. Effect of a novel vendor-specific motion-correction algorithm on image quality and diagnostic accuracy in persons undergoing coronary CT angiography without rate-control medications. J Cardiovasc Comput Tomogr. 2012; 6:164–171. PMID:
22551593.

28. Fan L, Zhang J, Xu D, Dong Z, Li X, Zhang L. CTCA image quality improvement by using snapshot freeze technique under prospective and retrospective electrocardiographic gating. J Comput Assist Tomogr. 2015; 39:202–206. PMID:
25564298.

29. Lee H, Kim JA, Lee JS, Suh J, Paik SH, Park JS. Impact of a vendor-specific motion-correction algorithm on image quality, interpretability, and diagnostic performance of daily routine coronary CT angiography: influence of heart rate on the effect of motion-correction. Int J Cardiovasc Imaging. 2014; 30:1603–1612. PMID:
25038955.

30. Carrascosa P, Deviggiano A, Capunay C, De Zan MC, Goldsmit A, Rodriguez-Granillo GA. Effect of intracycle motion correction algorithm on image quality and diagnostic performance of computed tomography coronary angiography in patients with suspected coronary artery disease. Acad Radiol. 2015; 22:81–86. PMID:
25281361.

31. Pontone G, Andreini D, Bertella E, Baggiano A, Mushtaq S, Loguercio M, et al. Impact of an intra-cycle motion correction algorithm on overall evaluability and diagnostic accuracy of computed tomography coronary angiography. Eur Radiol. 2016; 26:147–156. PMID:
25953001.

32. Liang J, Wang H, Xu L, Dong L, Fan Z, Wang R, et al. Impact of SSF on diagnostic performance of coronary computed tomography angiography within 1 heart beat in patients with high heart rate using a 256-row detector computed tomography. J Comput Assist Tomogr. 2018; 42:54–61. PMID:
28708724.

33. Chen Y, Wei D, Li D, Liu Z, Hu Z, Li M, et al. The value of 16-cm wide-detector computed tomography in coronary computed tomography angiography for patients with high heart rate variability. J Comput Assist Tomogr. 2018; 42:906–911. PMID:
30119063.

34. Park JB, Jeong YJ, Lee G, Lee NK, Kim JY, Lee JW. Influence of heart rate and innovative motion-correction algorithm on coronary artery image quality and measurement accuracy using 256-detector row computed tomography scanner: phantom study. Korean J Radiol. 2019; 20:94–101. PMID:
30627025.

35. Raman SV, Shah M, McCarthy B, Garcia A, Ferketich AK. Multi-detector row cardiac computed tomography accurately quantifies right and left ventricular size and function compared with cardiac magnetic resonance. Am Heart J. 2006; 151:736–744. PMID:
16504643.

36. Asferg C, Usinger L, Kristensen TS, Abdulla J. Accuracy of multi-slice computed tomography for measurement of left ventricular ejection fraction compared with cardiac magnetic resonance imaging and two-dimensional transthoracic echocardiography: a systematic review and meta-analysis. Eur J Radiol. 2012; 81:e757–e762. PMID:
22381439.
37. de Graaf FR, Schuijf JD, van Velzen JE, Nucifora G, Kroft LJ, de Roos A, et al. Assessment of global left ventricular function and volumes with 320-row multidetector computed tomography: a comparison with 2D-echocardiography. J Nucl Cardiol. 2010; 17:225–231. PMID:
19953354.

38. Kang EJ, Lee KN, Choi WJ, Kim YD, Shin KM, Lim JK, et al. Left ventricular functional parameters and geometric patterns in Korean adults on coronary CT angiography with a 320-detector-row CT scanner. Korean J Radiol. 2017; 18:664–673. PMID:
28670161.

39. Voros S. What are the potential advantages and disadvantages of volumetric CT scanning? J Cardiovasc Comput Tomogr. 2009; 3:67–70. PMID:
19201673.

40. de Roos A. Myocardial perfusion imaging with multidetector CT: beyond lumenography. Radiology. 2010; 254:321–323. PMID:
20093505.

41. Iwasaki K. Myocardial ischemia is a key factor in the management of stable coronary artery disease. World J Cardiol. 2014; 6:130–139. PMID:
24772253.

42. Groothuis JG, Beek AM, Brinckman SL, Meijerink MR, Koestner SC, Nijveldt R, et al. Low to intermediate probability of coronary artery disease: comparison of coronary CT angiography with first-pass MR myocardial perfusion imaging. Radiology. 2010; 254:384–392. PMID:
20089723.

43. Yang DH, Kim YH. CT myocardial perfusion imaging: current status and future perspectives. Int J Cardiovasc Imaging. 2017; 33:1009–1020. PMID:
28281025.

44. Seitun S, De Lorenzi C, Cademartiri F, Buscaglia A, Travaglio N, Balbi M, et al. CT myocardial perfusion imaging: a new frontier in cardiac imaging. Biomed Res Int. 2018; 2018:7295460. PMID:
30406139.

45. Kurata A, Mochizuki T, Koyama Y, Haraikawa T, Suzuki J, Shigematsu Y, et al. Myocardial perfusion imaging using adenosine triphosphate stress multi-slice spiral computed tomography: alternative to stress myocardial perfusion scintigraphy. Circ J. 2005; 69:550–557. PMID:
15849441.
46. Takx RA, Blomberg BA, El Aidi H, Habets J, de Jong PA, Nagel E, et al. Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging. 2015; 8:e002666. PMID:
25596143.

47. Cademartiri F, Seitun S, Clemente A, La Grutta L, Toia P, Runza G, et al. Myocardial blood flow quantification for evaluation of coronary artery disease by computed tomography. Cardiovasc Diagn Ther. 2017; 7:129–150. PMID:
28540209.

48. George RT, Mehra VC, Chen MY, Kitagawa K, Arbab-Zadeh A, Miller JM, et al. Myocardial CT perfusion imaging and SPECT for the diagnosis of coronary artery disease: a head-to-head comparison from the CORE320 multicenter diagnostic performance study. Radiology. 2014; 272:407–416. PMID:
24865312.

49. Pelgrim GJ, Nieuwenhuis ER, Duguay TM, van der Geest RJ, Varga-Szemes A, Slump CH, et al. Optimal timing of image acquisition for arterial first pass CT myocardial perfusion imaging. Eur J Radiol. 2017; 86:227–233. PMID:
28027752.

50. van Rosendael AR, de Graaf MA, Dimitriu-Leen AC, van Zwet EW, van den Hoogen IJ, Kharbanda RK, et al. The influence of clinical and acquisition parameters on the interpretability of adenosine stress myocardial computed tomography perfusion. Eur Heart J Cardiovasc Imaging. 2017; 18:203–211. PMID:
27013247.

51. Kitagawa K, Goto Y, Nakamura S, Takafuji M, Hamdy A, Ishida M, et al. Dynamic CT perfusion imaging: state of the art. Cardiovasc Imaging Asia. 2018; 2:38–48.

52. George RT, Arbab-Zadeh A, Miller JM, Vavere AL, Bengel FM, Lardo AC, et al. Computed tomography myocardial perfusion imaging with 320-row detector computed tomography accurately detects myocardial ischemia in patients with obstructive coronary artery disease. Circ Cardiovasc Imaging. 2012; 5:333–340. PMID:
22447807.

53. Rochitte CE, George RT, Chen MY, Arbab-Zadeh A, Dewey M, Miller JM, et al. Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J. 2014; 35:1120–1130. PMID:
24255127.
54. Cury RC, Kitt TM, Feaheny K, Blankstein R, Ghoshhajra BB, Budoff MJ, et al. A randomized, multicenter, multivendor study of myocardial perfusion imaging with regadenoson CT perfusion vs single photon emission CT. J Cardiovasc Comput Tomogr. 2015; 9:103–112.e1-e2. PMID:
25726411.

55. Chen MY, Rochitte CE, Arbab-Zadeh A, Dewey M, George RT, Miller JM, et al. Prognostic value of combined CT angiography and myocardial perfusion imaging versus invasive coronary angiography and nuclear stress perfusion imaging in the prediction of major adverse cardiovascular events: the CORE320 multicenter study. Radiology. 2017; 284:55–65. PMID:
28290782.
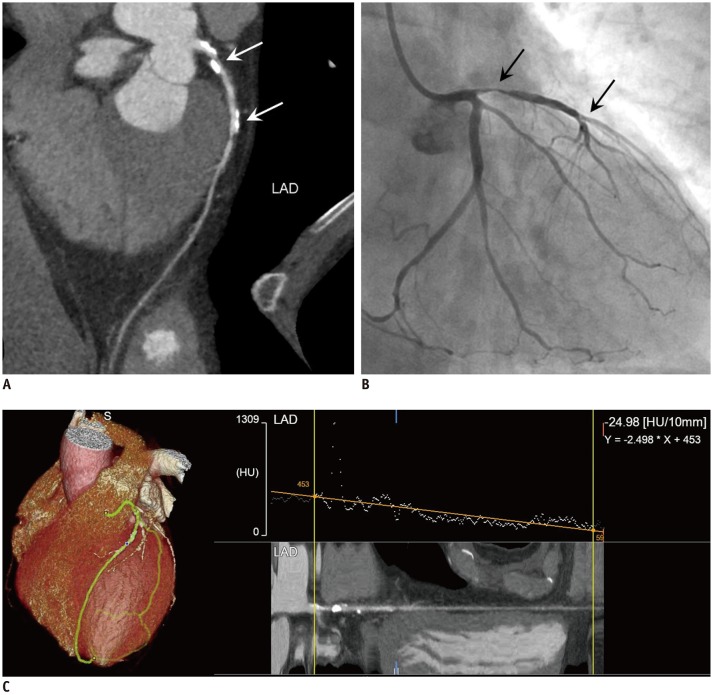
56. Steigner ML, Mitsouras D, Whitmore AG, Otero HJ, Wang C, Buckley O, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010; 3:179–186. PMID:
20044512.

57. Choi JH, Min JK, Labounty TM, Lin FY, Mendoza DD, Shin DH, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging. 2011; 4:1149–1157. PMID:
22093264.

58. Yoon YE, Choi JH, Kim JH, Park KW, Doh JH, Kim YJ, et al. Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography: diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. JACC Cardiovasc Imaging. 2012; 5:1088–1096. PMID:
23153908.
59. Wong DT, Ko BS, Cameron JD, Nerlekar N, Leung MC, Malaiapan Y, et al. Transluminal attenuation gradient in coronary computed tomography angiography is a novel noninvasive approach to the identification of functionally significant coronary artery stenosis: a comparison with fractional flow reserve. J Am Coll Cardiol. 2013; 61:1271–1279. PMID:
23414792.
60. Stuijfzand WJ, Danad I, Raijmakers PG, Marcu CB, Heymans MW, van Kuijk CC, et al. Additional value of transluminal attenuation gradient in CT angiography to predict hemodynamic significance of coronary artery stenosis. JACC Cardiovasc Imaging. 2014; 7:374–386. PMID:
24631509.

61. Ko BS, Wong DT, Nørgaard BL, Leong DP, Cameron JD, Gaur S, et al. Diagnostic performance of transluminal attenuation gradient and noninvasive fractional flow reserve derived from 320-detector row CT angiography to diagnose hemodynamically significant coronary stenosis: an NXT substudy. Radiology. 2016; 279:75–83. PMID:
26444662.

62. Chow BJ, Kass M, Gagné O, Chen L, Yam Y, Dick A, et al. Can differences in corrected coronary opacification measured with computed tomography predict resting coronary artery flow? J Am Coll Cardiol. 2011; 57:1280–1288. PMID:
21392642.

63. Park EA, Lee W, Park SJ, Kim YK, Hwang HY. Influence of coronary artery diameter on intracoronary transluminal attenuation gradient during CT angiography. JACC Cardiovasc Imaging. 2016; 9:1074–1083. PMID:
27372017.

64. Bom MJ, Driessen RS, Stuijfzand WJ, Raijmakers PG, Van Kuijk CC, Lammertsma AA, et al. Diagnostic value of transluminal attenuation gradient for the presence of ischemia as defined by fractional flow reserve and quantitative positron emission tomography. JACC Cardiovasc Imaging. 2019; 12:323–333. PMID:
29248645.

65. Goldstein JA, Gallagher MJ, O'Neill WW, Ross MA, O'Neil BJ, Raff GL. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007; 49:863–871. PMID:
17320744.

66. Hoffmann U, Bamberg F, Chae CU, Nichols JH, Rogers IS, Seneviratne SK, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (rule out myocardial infarction using computer assisted tomography) trial. J Am Coll Cardiol. 2009; 53:1642–1650. PMID:
19406338.
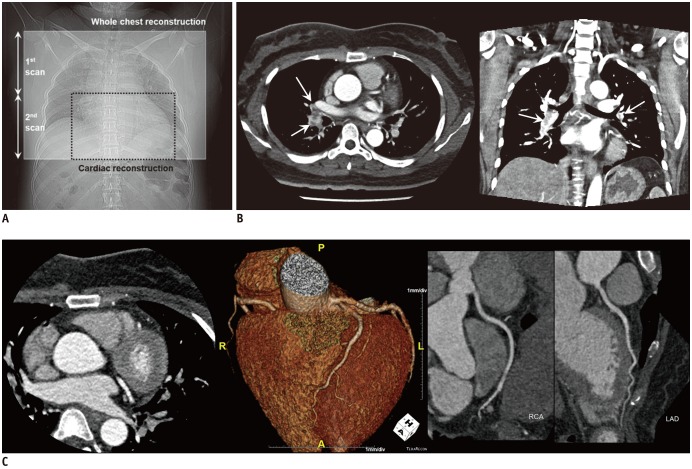
67. Sommer WH, Schenzle JC, Becker CR, Nikolaou K, Graser A, Michalski G, et al. Saving dose in triple-rule-out computed tomography examination using a high-pitch dual spiral technique. Invest Radiol. 2010; 45:64–71. PMID:
20027121.

68. Krissak R, Henzler T, Prechel A, Reichert M, Gruettner J, Sueselbeck T, et al. Triple-rule-out dual-source CT angiography of patients with acute chest pain: dose reduction potential of 100 kV scanning. Eur J Radiol. 2012; 81:3691–3696. PMID:
21163600.
69. Takx RAP, Krissak R, Fink C, Bachmann V, Henzler T, Meyer M, et al. Low-tube-voltage selection for triple-rule-out CTA: relation to patient size. Eur Radiol. 2017; 27:2292–2297. PMID:
27686566.

70. Hein PA, Romano VC, Lembcke A, May J, Rogalla P. Initial experience with a chest pain protocol using 320-slice volume MDCT. Eur Radiol. 2009; 19:1148–1155. PMID:
19137311.

71. Durmus T, Rogalla P, Lembcke A, Mühler MR, Hamm B, Hein PA. Low-dose triple-rule-out using 320-row-detector volume MDCT--less contrast medium and lower radiation exposure. Eur Radiol. 2011; 21:1416–1423. PMID:
21347640.
72. Kang EJ, Lee KN, Kim DW, Kim BS, Choi S, Park BH, et al. Triple rule-out acute chest pain evaluation using a 320-row-detector volume CT: a comparison of the wide-volume and helical modes. Int J Cardiovasc Imaging. 2012; 28 Suppl 1:7–13. PMID:
22618435.

73. Chen Y, Wang Q, Li J, Jia Y, Yang Q, He T. Triple-rule-out CT angiography using two axial scans with 16 cm wide-detector for radiation dose reduction. Eur Radiol. 2018; 28:4654–4661. PMID:
29789908.
74. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011; 364:2187–2198. PMID:
21639811.

75. Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tuzcu EM, et al. PARTNER 1 trial investigators. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015; 385:2477–2484. PMID:
25788234.
76. Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. PARTNER 2 Investigators. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016; 374:1609–1620. PMID:
27040324.
77. Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Søndergaard L, Mumtaz M, et al. SURTAVI Investigators. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017; 376:1321–1331. PMID:
28304219.

78. Blanke P, Weir-McCall JR, Achenbach S, Delgado V, Hausleiter J, Jilaihawi H, et al. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI) / transcatheter aortic valve replacement (TAVR): an expert consensus document of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2019; 13:1–20.

79. Achenbach S, Delgado V, Hausleiter J, Schoenhagen P, Min JK, Leipsic JA. SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr. 2012; 6:366–380. PMID:
23217460.

80. Gilard M, Eltchaninoff H, Iung B, Donzeau-Gouge P, Chevreul K, Fajadet J, et al. FRANCE 2 Investigators. Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med. 2012; 366:1705–1715. PMID:
22551129.
81. Zahn R, Gerckens U, Grube E, Linke A, Sievert H, Eggebrecht H, et al. German Transcatheter Aortic Valve Interventions-Registry Investigators. Transcatheter aortic valve implantation: first results from a multi-centre real-world registry. Eur Heart J. 2011; 32:198–204. PMID:
20864486.

82. Mata-Mbemba D, Labani A, El Ghannudi S, Jeung MY, Ohlmann P, Roy C, et al. 320-row CT transcatheter aortic valve replacement planning with a single reduced contrast media bolus injection. PLoS One. 2018; 13:e0204145. PMID:
30212567.

83. Pulerwitz TC, Khalique OK, Nazif TN, Rozenshtein A, Pearson GD, Hahn RT, et al. Very low intravenous contrast volume protocol for computed tomography angiography providing comprehensive cardiac and vascular assessment prior to transcatheter aortic valve replacement in patients with chronic kidney disease. J Cardiovasc Comput Tomogr. 2016; 10:316–321. PMID:
27061253.

84. Shuman WP, Green DE, Busey JM, Ramos MM, Branch KR, Koprowicz KM, et al. Wide-detector axial CT versus 4 cm detector helical CT for transcatheter aortic valve replacement: iodine dose, radiation, and image quality. Clin Imaging. 2016; 40:1213–1218. PMID:
27616154.

85. Kroft LJ, Roelofs JJ, Geleijns J. Scan time and patient dose for thoracic imaging in neonates and small children using axial volumetric 320-detector row CT compared to helical 64-, 32-, and 16- detector row CT acquisitions. Pediatr Radiol. 2010; 40:294–300. PMID:
19997730.

86. Podberesky DJ, Angel E, Yoshizumi TT, Toncheva G, Salisbury SR, Brody AS, et al. Comparison of radiation dose estimates and scan performance in pediatric high-resolution thoracic CT for volumetric 320-detector row, helical 64-detector row, and noncontiguous axial scan acquisitions. Acad Radiol. 2013; 20:1152–1161. PMID:
23931430.

87. Ryu YJ, Kim WS, Choi YH, Cheon JE, Lee SM, Cho HH, et al. Pediatric chest CT: wide-volume and helical scan modes in 320-MDCT. AJR Am J Roentgenol. 2015; 205:1315–1321. PMID:
26587939.

88. Zhu Y, Li Z, Ma J, Hong Y, Pi Z, Qu X, et al. Imaging the infant chest without sedation: feasibility of using single axial rotation with 16-cm wide-detector CT. Radiology. 2018; 286:279–285. PMID:
28956735.

89. Gottumukkala RV, Kalra MK, Tabari A, Otrakji A, Gee MS. Advanced CT techniques for decreasing radiation dose, reducing sedation requirements, and optimizing image quality in children. Radiographics. 2019; 39:709–726. PMID:
30924753.

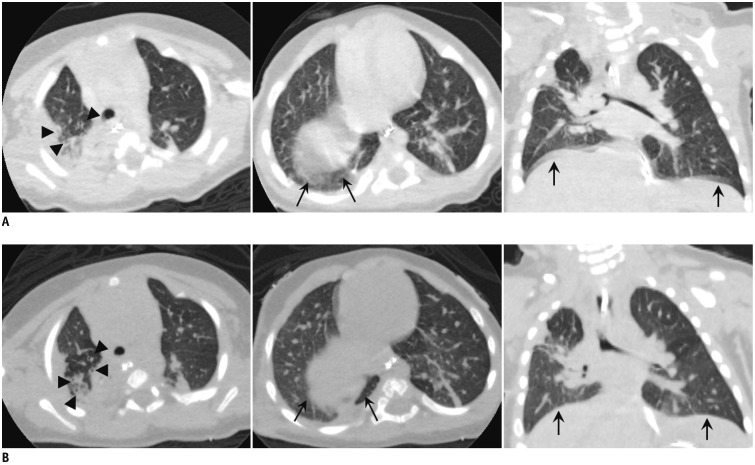
90. Greenberg SB. Dynamic pulmonary CT of children. AJR Am J Roentgenol. 2012; 199:435–440. PMID:
22826409.

91. Mok Q, Negus S, McLaren CA, Rajka T, Elliott MJ, Roebuck DJ, et al. Computed tomography versus bronchography in the diagnosis and management of tracheobronchomalacia in ventilator dependent infants. Arch Dis Child Fetal Neonatal Ed. 2005; 90:F290–F293. PMID:
15857878.

92. Baroni RH, Feller-Kopman D, Nishino M, Hatabu H, Loring SH, Ernst A, et al. Tracheobronchomalacia: comparison between end-expiratory and dynamic expiratory CT for evaluation of central airway collapse. Radiology. 2005; 235:635–641. PMID:
15798155.

93. Lee EY, Boiselle PM. Tracheobronchomalacia in infants and children: multidetector CT evaluation. Radiology. 2009; 252:7–22. PMID:
19561247.

94. Lee KS, Sun MRM, Ernst A, Feller-Kopman D, Majid A, Boiselle PM. Comparison of dynamic expiratory CT with bronchoscopy for diagnosing airway malacia: a pilot evaluation. Chest. 2007; 131:758–764. PMID:
17356090.
95. Wagnetz U, Roberts HC, Chung T, Patsios D, Chapman KR, Paul NS. Dynamic airway evaluation with volume CT: initial experience. Can Assoc Radiol J. 2010; 61:90–97. PMID:
20060258.

96. Greenberg SB, Dyamenahalli U. Dynamic pulmonary computed tomography angiography: a new standard for evaluation of combined airway and vascular abnormalities in infants. Int J Cardiovasc Imaging. 2014; 30:407–414. PMID:
24322888.

97. Andronikou S, Chopra M, Langton-Hewer S, Maier P, Green J, Norbury E, et al. Technique, pitfalls, quality, radiation dose and findings of dynamic 4-dimensional computed tomography for airway imaging in infants and children. Pediatr Radiol. 2019; 49:678–686. PMID:
30683962.

98. Kang EJ, Lee J, Lee KN, Kown H, Ha DH, Kim RB. An initial randomised study assessing free-breathing CCTA using 320-detector CT. Eur Radiol. 2013; 23:1199–1209. PMID:
23138388.

99. Liu Z, Sun Y, Zhang Z, Chen L, Hong N. Feasibility of free-breathing CCTA using 256-MDCT. Medicine (Baltimore). 2016; 95:e4096. PMID:
27399104.

100. Liu Z, Zhang Z, Hong N, Chen L, Cao C, Liu J, et al. Diagnostic performance of free-breathing coronary computed tomography angiography without heart rate control using 16-cm z-coverage CT with motion-correction algorithm. J Cardiovasc Comput Tomogr. 2019; 13:113–117. PMID:
30635197.

101. Park MJ, Jung JI, Choi YS, Ann SH, Youn HJ, Jeon GN, et al. Coronary CT angiography in patients with high calcium score: evaluation of plaque characteristics and diagnostic accuracy. Int J Cardiovasc Imaging. 2011; 27 Suppl 1:43–51. PMID:
22048849.

102. Andrew M, John H. The challenge of coronary calcium on coronary computed tomographic angiography (CCTA) scans: effect on interpretation and possible solutions. Int J Cardiovasc Imaging. 2015; 31 Suppl 2:145–157. PMID:
26408105.

103. Yoshioka K, Tanaka R. Subtraction coronary CT angiography for the evaluation of severely calcified lesions using a 320-detector row scanner. Curr Cardiovasc Imaging Rep. 2011; 4:437–446.

104. Tanaka R, Yoshioka K, Muranaka K, Chiba T, Ueda T, Sasaki T, et al. Improved evaluation of calcified segments on coronary CT angiography: a feasibility study of coronary calcium subtraction. Int J Cardiovasc Imaging. 2013; 29 Suppl 2:75–81. PMID:
24158235.

105. Fuchs A, Kühl JT, Chen MY, Helqvist S, Razeto M, Arakita K, et al. Feasibility of coronary calcium and stent image subtraction using 320-detector row CT angiography. J Cardiovasc Comput Tomogr. 2015; 9:393–398. PMID:
26091841.

106. Viladés Medel D, Leta R, Alomar Serralach X, Carreras Costa F, Pons-Lladó G. Reliability of a new method for coronary artery calcium or metal subtraction by 320-row cardiac CT. Eur Radiol. 2016; 26:3208–3214. PMID:
26662029.

107. Kidoh M, Utsunomiya D, Oda S, Yuki H, Funama Y, Namimoto T, et al. Optimized subtraction coronary CT angiography protocol for clinical use with short breath-holding time-initial experience. Acad Radiol. 2015; 22:117–120. PMID:
25481519.
108. Yamaguchi T, Ichikawa K, Takahashi D, Sugaya T, Furuya J, Igarashi K. A new contrast enhancement protocol for subtraction coronary computed tomography requiring a short breath-holding time. Acad Radiol. 2017; 24:38–44. PMID:
27765596.

109. Fuchs A, Kühl JT, Chen MY, Viladés Medel D, Alomar X, Shanbhag SM, et al. Subtraction CT angiography improves evaluation of significant coronary artery disease in patients with severe calcifications or stents-the C-sub 320 multicenter trial. Eur Radiol. 2018; 28:4077–4085. PMID:
29696430.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download