INTRODUCTION
Current guidelines recommend decision making based on the SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) score (SS) for patients with left main and/or 3-vessel disease.
1)2) Five-year clinical outcomes from the SYNTAX trial showed that the major adverse cardiac and cerebrovascular events (MACCE) were similar between the percutaneous coronary intervention (PCI) arm and the coronary artery bypass graft (CABG) arm in patients with low/intermediate SS (0–32).
3)4) In contrast, MACCE was significantly higher after PCI than after CABG in patients with high scores (≥33). Recently, SS II was proposed to overcome the limitations of anatomical SS by incorporating clinical variables, such as age, sex, creatinine clearance, left ventricular (LV) ejection fraction, chronic obstructive pulmonary disease, and peripheral vascular disease. However, SYNTAX trials were performed with paclitaxel-eluting stent, which is not used any more. Contemporary second-generation drug-eluting stent (DES), especially cobalt-chromium everolimus-eluting stent (CoCr-EES), demonstrated better safety and efficacy outcomes.
5)6)7)8) CoCr-EES was suggested to have the best combination of efficacy and safety
6) and may be one of the most advanced contemporary DESs. SS systems, including SS and SS II have not been validated in CoCr-EES; thus, we are not confident that the current guidelines based on SS systems can be justified in the contemporary DES era. In this study, we aimed to test whether the anatomical SS and SS II in incorporating clinical factors could still effectively predict the outcomes of patients with left main and/or 3-vessel disease undergoing PCI with the contemporary CoCr-EES.
DISCUSSION
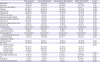
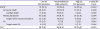
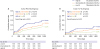
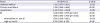
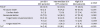
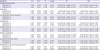
In this study, SS and SS II were assessed in patients with left main and/or 3-vessel disease who underwent PCI with the contemporary CoCr-EES from 2 large all-comer registries. The main findings were that: 1) SS was an independent predictor of 3-year POCE, 2) SS II held a substantially improved predictive power for 3-year POCE, but not for TLF, and 3) in a subgroup analysis, SS II showed particularly better predictive accuracy compared with SS, for 3-year POCE in patients with clinical cardiovascular risk factors or in patients presenting with stable angina.
The SS was developed based on the population of patients with left main and/or 3-vessel disease who underwent paclitaxel-eluting stent implantation.
12) Based on the long-term follow-up results of the validation study,
13) the SS is regarded as a useful tool to select the appropriate method of revascularization: PCI versus surgery.
14) Furthermore, various studies have shown that the SS can be used as a risk stratification tool for patients with coronary artery disease who received PCI.
15)16) However, the critical weak point of SS system is that the SYNTAX trial was performed about a decade earlier. It is a study of the first-generation DES era when the DES performance was not as good as that of contemporary DESs and when intravascular imaging and fractional flow reserve were not frequently adopted. Moreover, adjunctive medical therapy, such as dual antiplatelet agents and statin was not thoroughly used. In this regard, re-validation of SS system is needed before applying SS to the current clinical practice. In addition, various scoring systems were derived from the SS so as to improve the predictability for the original SS.
17)18) However, previous scores were derived from old generation stents, which was known to be inferior to current generation DESs. Especially, the SS II was recently proposed to overcome the intrinsic limitations of the SS which solely relied on anatomical factors. By adding clinical factors of a patient, SS II was intended to enhance the predictive value. This scoring system was also developed based on the SYNTAX trial, and validated on the Drug Eluting stent for LefT main coronary Artery disease registry of the first-generation DES era.
19) Thus, SS II also needs re-validation in contemporary patient population.
A few studies have assessed the predictive values of SS
15)18) and SS II for long-term clinical outcomes in a PCI population.
20)21)22) However, these studies included patients who received 1st generation DESs, and were not limited to patients with left main and/or 3-vessel disease in whom the use of SS was intended in the original SYNTAX study
3) and indicated by current guidelines.
1)2) In addition, regarding the comparison of SS and SSII, Song et al. recently compared the predictive value of SS and SS II for 2-year mortality in patients with left main and/or 3-vessel disease undergoing PCI.
23) In this single-center study, about 10% of study population did not receive 2nd generation DESs, and SS and SS II were quite low (SS: 16.0±8.2 compared with 21.1±9.6 in our study, SS II: 23.6±6.5 compared with 35.5±11.3 in our study). Furthermore, the mortality rate in this study was very low (1.3%, compared with 8.5% in our study), suggesting that this study included a very low-risk population that might not represent well the population that needs the calculation of SS or SS II. Collectively, previous studies did not thoroughly validate SS and SS II in a contemporary 2nd generation DES era. Therefore, the main purpose of our study was to validate the SS and SS II in a pure contemporary CoCr-EES population with left main and/or 3-vessel disease in a 3-year follow-up duration, which is the main difference between previous evidences and the current study. Through our analysis of more than 1,200 patients, we demonstrated the predictive value of both SS and SS II in the contemporary DES era. Interestingly, the predictive value of SS II was superior compared to SS for patient oriented clinical outcomes, while both values were comparable for lesion specific outcomes. This finding is reasonable because firstly, SS II was initially developed to predict all-cause mortality which was the ultimate patient-orient outcome, and secondly, SS II includes clinical variables in contrast to SS which only take anatomical variables of lesions into account. In fact, we found the superior predictive value of SS II especially for all-cause mortality.
Despite the improvement in the predictive performance of SS II, it may not have well penetrated into the daily practice. This situation is attributed to the 7 additional factors included in SS II that requires utilization of a complex nomogram or web-based calculator. Thus, to reveal the situations when SS II is superior to the SS is practically useful. Our study showed that SS II was superior in predicting patient-related outcomes, but had no additive value in predicting lesion-related outcomes. This means that an anatomical scoring system, such as SS may be sufficient to predict outcomes of the lesion. However, to predict outcomes of a patient, incorporating clinical variables are superior.
In addition, SS II was particularly useful to predict the clinical outcomes in patients with cardiovascular risk factors, such as male sex, old age, low BMI, hypertension, diabetes mellitus, chronic renal failure, and depressed LV systolic function. We think that this was a reasonable result, because combining more risk factors usually improves predictive values. Interestingly, regarding the clinical presentation, the additive value of SS II was limited in ACS patients; SS II was superior to SS only in patients presenting as stable angina. This may be explained by the importance of the coronary anatomy in ACS patients. ACS patients are more likely to have more significant stenosis which threatens the myocardial viability by decreased coronary flow. In these patients, relieving angiographic stenosis through PCI may have a larger effect on clinical outcomes. On the contrary, for patients with stable angina, medical treatment for clinical factors may have a larger portion to determine the clinical outcomes. Considering that the SYNTAX score II incorporates clinical risk factors to the anatomical risk factors, this may explain the observed better predictive value of SS II in patients with stable angina.
Our registries only included the patients undergoing PCI; hence, we could not provide the comparison between contemporary DES and CABG according to SS and SS II. In addition, our study patients were implanted with only CoCr-EES among the various contemporary DESs. However, CoCr-EES is regarded as the most advanced contemporary DESs. Thus, we believe that our study well represents the current status of the DES use. Also, according to current guidelines, CABG is preferred to those with a high SS. It should be noticed that the reason these patients were unsuitable for CABG might act as a factor of worst outcome. This can be addressed as a selection bias, that should be considered in interpretation of our results.
In conclusions, the usefulness of SS and SS II could be extended to patients with left main and/or 3-vessel disease who received PCI with CoCr-EES. SS II was superior to SS in predicting patient-oriented outcomes, particularly in patients with clinical cardiovascular risk factors or patients without ACS.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download