1. Practice Guidelines for Moderate Procedural Sedation and Analgesia. Practice guidelines for moderate procedural sedation and analgesia 2018: a report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology. 2018; 128:437–479.

2. Shabanie A. Conscious sedation for interventional procedures: a practical guide. Tech Vasc Interv Radiol. 2006; 9:84–88.


4. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017; 126:376–393.

5. Agarwal A, Chari P, Singh H. Fluid deprivation before operation. The effect of a small drink. Anaesthesia. 1989; 44:632–634.
6. Agrawal D, Manzi SF, Gupta R, Krauss B. Preprocedural fasting state and adverse events in children undergoing procedural sedation and analgesia in a pediatric emergency department. Ann Emerg Med. 2003; 42:636–646.


7. Bell A, Treston G, McNabb C, Monypenny K, Cardwell R. Profiling adverse respiratory events and vomiting when using propofol for emergency department procedural sedation. Emerg Med Australas. 2007; 19:405–410.


8. Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006; 104:228–234.

10. Choi JW, Kim DK, Cho CK, Park SJ, Son YH. Trends in medical disputes involving anesthesia during July 2009–June 2018: an analysis of the Korean Society of Anesthesiologists database. Korean J Anesthesiol. 2019; 72:156–163.

11. Metzner J, Domino KB. Risks of anesthesia or sedation outside the operating room: the role of the anesthesia care provider. Curr Opin Anaesthesiol. 2010; 23:523–531.


12. Cacho G, Pérez-Calle JL, Barbado A, Lledó JL, Ojea R, Fernández-Rodríguez CM. Capnography is superior to pulse oximetry for the detection of respiratory depression during colonoscopy. Rev Esp Enferm Dig. 2010; 102:86–89.


13. Qadeer MA, Vargo JJ, Dumot JA, et al. Capnographic monitoring of respiratory activity improves safety of sedation for endoscopic cholangiopancreatography and ultrasonography. Gastroenterology. 2009; 136:1568–1576.


14. Fruchter O, Tirosh M, Carmi U, Rosengarten D, Kramer MR. Prospective randomized trial of bispectral index monitoring of sedation depth during flexible bronchoscopy. Respiration. 2014; 87:388–393.


15. Weaver CS, Hauter WH, Duncan CE, Brizendine EJ, Cordell WH. An assessment of the association of bispectral index with 2 clinical sedation scales for monitoring depth of procedural sedation. Am J Emerg Med. 2007; 25:918–924.

16. Paspatis GA, Chainaki I, Manolaraki MM, et al. Efficacy of bispectral index monitoring as an adjunct to propofol deep sedation for ERCP: a randomized controlled trial. Endoscopy. 2009; 41:1046–1051.


17. von Delius S, Salletmaier H, Meining A, et al. Bispectral index monitoring of midazolam and propofol sedation during endoscopic retrograde cholangiopancreatography: a randomized clinical trial (the EndoBIS study). Endoscopy. 2012; 44:258–264.


18. Jung SM, Lee E, Park SJ. Validity of bispectral index monitoring during deep sedation in children with spastic cerebral palsy undergoing injection of botulinum toxin. Korean J Anesthesiol. 2019; [Epub ahead of print].

19. Forster A, Gardaz JP, Suter PM, Gemperle M. Respiratory depression by midazolam and diazepam. Anesthesiology. 1980; 53:494–497.


20. Raza SM, Zsigmond EK, Barabas E. Midazolam causes no adverse hemodynamic effects in cardiac patients. Clin Ther. 1987; 10:40–43.

21. Skarvan K, Schwinn W. Hemodynamic interaction between midazolam and alfentanil in coronary patients. Anaesthesist. 1986; 35:17–23.

22. Pentikäinen PJ, Välisalmi L, Himberg JJ, Crevoisier C. Pharmacokinetics of midazolam following intravenous and oral administration in patients with chronic liver disease and in healthy subjects. J Clin Pharmacol. 1989; 29:272–277.


23. Bauer TM, Ritz R, Haberthür C, et al. Prolonged sedation due to accumulation of conjugated metabolites of midazolam. Lancet. 1995; 346:145–147.

24. Golparvar M, Saghaei M, Sajedi P, Razavi SS. Paradoxical reaction following intravenous midazolam premedication in pediatric patients - a randomized placebo controlled trial of ketamine for rapid tranquilization. Paediatr Anaesth. 2004; 14:924–930.


25. Mancuso CE, Tanzi MG, Gabay M. Paradoxical reactions to benzodiazepines: literature review and treatment options. Pharmacotherapy. 2004; 24:1177–1185.


26. Jackson BF, Beck LA, Losek JD. Successful flumazenil reversal of paradoxical reaction to midazolam in a child. J Emerg Med. 2015; 48:e67–e72.

27. Khan LC, Lustik SJ. Treatment of a paradoxical reaction to midazolam with haloperidol. Anesth Analg. 1997; 85:213–215.


28. Bryson HM, Fulton BR, Faulds D. Propofol. An update of its use in anaesthesia and conscious sedation. Drugs. 1995; 50:513–559.

29. Schüttler J, Ihmsen H. Population pharmacokinetics of propofol: a multicenter study. Anesthesiology. 2000; 92:727–738.

31. Hughes MA, Glass PS, Jacobs JR. Context-sensitive half-time in multicompartment pharmacokinetic models for intravenous anesthetic drugs. Anesthesiology. 1992; 76:334–341.

32. Dahan A, Nieuwenhuijs DJ, Olofsen E. Influence of propofol on the control of breathing. Adv Exp Med Biol. 2003; 523:81–92.


33. Goodman NW, Black AM, Carter JA. Some ventilatory effects of propofol as sole anaesthetic agent. Br J Anaesth. 1987; 59:1497–1503.


34. Larsen R, Rathgeber J, Bagdahn A, Lange H, Rieke H. Effects of propofol on cardiovascular dynamics and coronary blood flow in geriatric patients. A comparison with etomidate. Anaesthesia. 1988; 43 Suppl:25–31.

35. Robinson BJ, Ebert TJ, O'Brien TJ, Colinco MD, Muzi M. Mechanisms whereby propofol mediates peripheral vasodilation in humans. Sympathoinhibition or direct vascular relaxation? Anesthesiology. 1997; 86:64–72.

36. Kazama T, Ikeda K, Morita K, et al. Comparison of the effect-site k
eOs of propofol for blood pressure and EEG bispectral index in elderly and younger patients. Anesthesiology. 1999; 90:1517–1527.

37. Mamiya H, Noma T, Fukuda K, Kasahara M, Ichinohe T, Kaneko Y. Pain following intravenous administration of sedative agents: a comparison of propofol with three benzodiazepines. Anesth Prog. 1998; 45:18–21.


39. Brechmann T, Maier C, Kaisler M, et al. Propofol sedation during gastrointestinal endoscopy arouses euphoria in a large subset of patients. United European Gastroenterol J. 2018; 6:536–546.


40. Bennett SN, McNeil MM, Bland LA, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med. 1995; 333:147–154.


42. Guo TZ, Jiang JY, Buttermann AE, Maze M. Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology. 1996; 84:873–881.


43. Angst MS, Ramaswamy B, Davies MF, Maze M. Comparative analgesic and mental effects of increasing plasma concentrations of dexmedetomidine and alfentanil in humans. Anesthesiology. 2004; 101:744–752.


44. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–394.


45. Hsu YW, Cortinez LI, Robertson KM, et al. Dexmedetomidine pharmacodynamics: part I: crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology. 2004; 101:1066–1076.

46. Kang D, Lim C, Shim DJ, et al. The correlation of heart rate between natural sleep and dexmedetomidine sedation. Korean J Anesthesiol. 2019; 72:164–168.


47. Bhana N, Goa KL, McClellan KJ. Dexmedetomidine. Drugs. 2000; 59:263–268.

48. Riker RR, Fraser GL. Adverse events associated with sedatives, analgesics, and other drugs that provide patient comfort in the intensive care unit. Pharmacotherapy. 2005; 25:8S–18S.

50. Litman RS. Conscious sedation with remifentanil during painful medical procedures. J Pain Symptom Manage. 2000; 19:468–471.


51. Servin F. Remifentanil; from pharmacological properties to clinical practice. Adv Exp Med Biol. 2003; 523:245–260.


52. Salukhe TV, Willems S, Drewitz I, et al. Propofol sedation administered by cardiologists without assisted ventilation for long cardiac interventions: an assessment of 1000 consecutive patients undergoing atrial fibrillation ablation. Europace. 2012; 14:325–330.


53. Wutzler A, Loehr L, Huemer M, et al. Deep sedation during catheter ablation for atrial fibrillation in elderly patients. J Interv Card Electrophysiol. 2013; 38:115–121.


54. Cho JS, Shim JK, Na S, Park I, Kwak YL. Improved sedation with dexmedetomidine-remifentanil compared with midazolam-remifentanil during catheter ablation of atrial fibrillation: a randomized, controlled trial. Europace. 2014; 16:1000–1006.


55. Di Biase L, Conti S, Mohanty P, et al. General anesthesia reduces the prevalence of pulmonary vein reconnection during repeat ablation when compared with conscious sedation: results from a randomized study. Heart Rhythm. 2011; 8:368–372.


56. Di Biase L, Saenz LC, Burkhardt DJ, et al. Esophageal capsule endoscopy after radiofrequency catheter ablation for atrial fibrillation: documented higher risk of luminal esophageal damage with general anesthesia as compared with conscious sedation. Circ Arrhythm Electrophysiol. 2009; 2:108–112.

57. Pires LA, Huang SK, Wagshal AB, Kulkarni RS. Electrophysiological effects of propofol on the normal cardiac conduction system. Cardiology. 1996; 87:319–324.

58. Niksch A, Liberman L, Clapcich A, Schwarzenberger JC, Silver ES, Pass RH. Effects of remifentanil anesthesia on cardiac electrophysiologic properties in children undergoing catheter ablation of supraventricular tachycardia. Pediatr Cardiol. 2010; 31:1079–1082.


59. Khan ZP, Ferguson CN, Jones RM. alpha-2 and imidazoline receptor agonists. Their pharmacology and therapeutic role. Anaesthesia. 1999; 54:146–165.
60. Lau W, Kovoor P, Ross DL. Cardiac electrophysiologic effects of midazolam combined with fentanyl. Am J Cardiol. 1993; 72:177–182.


62. Lewis SR, Nicholson A, Reed SS, Kenth JJ, Alderson P, Smith AF. Anaesthetic and sedative agents used for electrical cardioversion. Cochrane Database Syst Rev. 2015; CD010824.

63. Kalogridaki M, Souvatzis X, Mavrakis HE, et al. Anaesthesia for cardioversion: a prospective randomised comparison of propofol and etomidate combined with fentanyl. Hellenic J Cardiol. 2011; 52:483–488.

64. Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015; 116:1509–1526.


65. Trentman TL, Fassett SL, Mueller JT, Altemose GT. Airway interventions in the cardiac electrophysiology laboratory: a retrospective review. J Cardiothorac Vasc Anesth. 2009; 23:841–845.


66. Park JH, Soh S, Kwak YL, Kim B, Choi S, Shim JK. Anesthetic efficacy of dexmedetomidine versus midazolam when combined with remifentanil for percutaneous transluminal angioplasty in patients with peripheral artery disease. J Clin Med. 2019; 8:E472.


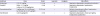




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download