Abstract
Purpose
Men take testosterone (T) boosting supplements to naturally improve T levels. We evaluated the composition and advertised claims of “T boosting” supplements, and supporting published evidence.
Materials and Methods
Fifty “T booster” supplements were evaluated for active ingredients and product claims, discovered via Google search. PubMed was reviewed for any literature supporting the claims, followed by review of Recommended Daily Allowance (RDA) and upper tolerable intake level (UL) for each component.
Results
Ninety percent of supplements claimed to “boost T”, 50% “improve libido”, and 48% “feel stronger”. One-hundred nine unique components were found, with a mean number of 8.3 per product. On PubMed, 24.8% of supplements had data showing an increase in T with supplementation, 10.1% had data showing a decrease in T, and 18.3% had data showing no change in T. No data were found on 61.5% of supplements on their effect on T. Supplements contained a median 1,291% of the RDA for vitamin B12, 807.6% for vitamin B6, 272% of zinc, 200% of vitamin B5, and 187.5% of vitamin B3. Thirteen products exceeded the US Food and Drug Administration UL of ingredients (zinc, vitamin B3, and magnesium).
Conclusions
Ninety percent of “T booster” supplements claimed to boost T. However, only 24.8% of these had data to support these claims. A total of 10.1% contained components with data suggesting a negative effect on T. Many had supra-therapeutic doses of vitamins and minerals, occasionally over the UL. Patients should be informed that “T booster” supplements may not have ingredients to support their claims.
A progressive decline in testosterone (T) is seen with male aging, estimated at 0.4% to 2.0% decline per year after age 30 [1]. It is estimated that men in their 70s have mean T levels 35% lower than younger men [2]. The reasons for this decline may be related to failure of the testes to produce T, impaired function of the hypothalamic-pituitary-gonadal axis, comorbid medical issues, exogenous medications or other factors. The symptoms of low T are relatively non-specific and can be seen with several other medical conditions, and an accurate diagnosis is vital to direct treatment.
Testosterone replacement therapy (TRT) is a well-established option for those with symptomatic hypogonadism related to low T levels. However, one study found that 87.8% men with low T were not receiving treatment, despite adequate access to care [3]. The reasons for this are unknown, but some of these men may be seeking alternative treatments, such as care at rejuvenation centers or using over the counter T supplements. These may be used in addition to TRT for males with diagnosed symptomatic hypogonadism, or as a stand-alone regimen.
Approximately 50% of American adults consume dietary supplements to promote overall health and fill dietary gaps [45]. These over the counter “T boosters” are often taken with the hopes of raising endogenous T production and doing this in a more “natural” manner. Many of these compounds have been used in ancient Indian Ayurvedic and Unani medicine systems for their aphrodisiac or anti-aging properties [6].
Despite their popularity, the scientific rationale for these products often remains unexplained or unproven. In addition, these compounds are often loosely regulated. Highlighting this, a 2015 evidence based review of medicinal plants used for the treatment of sperm abnormalities found that “more reliable evidence was found” for some of the supplements than others, and that further studies were needed to demonstrate safety and efficacy of these products [7]. The US Food and Drug Administration (FDA) clearly states that, “Unlike drugs, supplements are not intended to treat, diagnose, prevent, or cure diseases. That means supplements should not make claims, such as “reduces pain” or “treats heart disease”. Claims like these can only legitimately be made for drugs, not dietary supplements.” [8]. However, despite this clear FDA statement, there continue to be products that either directly claim or imply to have certain effects on medical conditions.
Men may take dietary supplements in hopes of improving their endogenous T production. It is important that these men have access to information that is evidence-based and will give them a realistic picture of what they can hope to see after using these supplements. The purpose of this study was to evaluate the composition of “T boosting” supplements, their advertised claims, and compare them with both the published literature and FDA recommendations.
We searched Google to identify 50 T supplements. We chose Google because it is the most widely used search engine, comprising 74.5% of Internet searches [9]. The search term used was “Testosterone Booster”. Other search terms such as “Testosterone Supplement” yielded products that contained exogenous sources of hormone, which is beyond the scope of this study. The first 50 supplements that were found were included in analysis. The individual combination supplements were evaluated for active ingredients and product claims. A total of 109 individual components were found.
A structured PubMed search was the performed for “testosterone” and each of the 109 components found in the supplements. Only studies looking at males were reviewed. Only articles that looked at the effect of supplementation were included.
We then reviewed the FDA Recommended Daily Allowance (RDA) for each of the vitamins contained in these supplements, as well as the upper tolerable intake level (UL) as set by the Institute of Medicine of the National Academy of Science [10] and compared this with the stated content for each supplement.
The present study is descriptive in nature, without direct patient or subject involvement, using commercially available online information on over-the-counter T supplements. The University of Southern California Institutional Review Board granted an exemption of this study (No. IIR00002922).
For the T booster supplements surveyed, 109 components were identified. There were a mean 8.3 components per supplement (range, 29; median, 7; mode, 6; standard deviation, 5.52; interquartile range, 1–7). The most common components for the supplements were zinc, fenugreek, vitamin B6, Tribulus, magnesium, boron, diindolemethane, Eurycoma longifolia, and Maca extract. A full list of the individual components, with percent of supplements containing these components, is found in Table 1.
A total of sixteen general claims to benefit patients were made by these supplements. Most frequently, claims to “boost T or free T”, “build body lean mass or muscle mass”, or “increase sex drive or libido” were advertised by the supplements. The claims and the number of supplements claiming these benefits are detailed in Table 2.
Regarding the results of our PubMed review, there were no studies looking at the effect of the individual supplements on T levels for 67 of the supplements (61.5%). For 19 supplements (17.4%) there was a single study looking at the effect of supplementation on T. For 13 supplements (11.9%) there were 2 studies; for 3 supplements (2.8%) there were 3 studies; for 4 supplements (3.7%) there were 4 studies; for 1 supplements (0.9%) there were 5 studies; for 1 supplements (0.9%) there were 6 studies.
For 27 individual supplements (24.8%), there was data showing an increase in T with supplementation. Eleven individual supplements (10.1%) had data showing a decrease in T with supplementation, and 20 individual supplements (18.3%) had data showing no change in T with supplementation. Given these findings, 15 individual supplements (13.8%) therefore had conflicting data regarding their effect on T. These data are summarized in Table 3.
We then surveyed the RDA and UL for each of the individual supplements. These results are in Table 2. Supplements contained a median 1,291% of the RDA for vitamin B12, 807.6% of vitamin B6, 272% of zinc, 200% of vitamin B5, and 187.5% of vitamin B3. Interestingly, the supplements contained a mean 3.1% of the RDA of calcium. Two supplements had greater than or equal to the UL of zinc (40 mg), 2 had greater than the UL of vitamin B3 (35 mg), and 9 were greater than the UL of magnesium (350 mg).
The progressive decrease in serum T with aging is a well-documented progress. TRT is a well-established treatment option for those with symptomatic T deficiency. TRT has a well-defined risk profile, with clear guidelines for indications, contraindications, dosing, treatment goals, and monitoring during treatment [11]. However, despite the FDA approved status of exogenous T, a recent review looking at the quality of online information related to TRT found that online information is incomplete, often failing to describe important safety information and the need for regular monitoring [12].
Herbal supplements designed to increase T are poorly studied yet remain popular among aging men who seek to increase their T without standard TRT. There is often the hope that supplements will increase T in a more “natural” manner, and therefore be free from risk. However, this does not appear to be the case. These products are often poorly regulated and minimally studied, both in terms of efficacy and toxicity profile.
Illustrating this, a 2017 case report described new-onset, bilateral pulmonary embolisms secondary to over-the-counter fenugreek-extract-containing T supplements [13]. In 2014, the FDA issued a general warning for the risk of venous blood clots associated with T product use [14]. While not specified in the FDA warning, this potential risk may extend to herbal T supplements as well. Another study looking at the effect of red clover on the quality of life, and sexual function in men found that this supplement did not change sexual or erectile function, and resulted in a significant increase in liver transaminases [15]. In short, these vitamin and herbal substances may not be as safe as the public perceives them to be.
In this study we sought to evaluate the composition of “T booster” supplements, their advertised claims, and we compared this with the published literature and RDA. In general, the available literature supporting the claims made by the supplements was often sparse or non-existent. Only 5.5% of supplements had more than two studies looking at their effect on T. Supplements 61.5% had no data looking at their effect on T.
For 24.8%, or 27 out of 109 individual supplements, there was data showing an increase in T with supplementation. However, for many of these (15 of the 27, or 55.5%) there was also conflicting data showing no change or a decrease in T with supplementation. Of concern, 10.1% of components had published data that found a decrease in T with supplementation. It is unclear why companies would include components in their supplements that have no evidence to support their use. However, it is even more concerning that some of these supplements may in fact decrease serum T.
RDA information was not available for many of the individual components for the “T boosters”. The FDA does not issue RDA and upper tolerable limit data for herbal supplements. Supplements contained a median 1,291% of the RDA for vitamin B12, 807.6% of vitamin B6, 272% of zinc, 200% of vitamin B5, and 187.5% of vitamin B3 (Table 4).
It is worrisome that two supplements had greater than the UL of zinc. Relatively low levels of zinc over-supplementation have been shown to interfere with the utilization of copper and iron and to adversely affect high-density lipoprotein cholesterol concentrations. Slightly higher doses have been shown to result in anemia and neutropenia, as well as impaired immune function [16].
According to the 2018 American Urological Association Guidelines on the Evaluation and Management of T Deficiency, patients should be informed that T therapy may improve in erectile function, low sex drive, anemia, bone mineral density, lean body mass and/or depressive symptoms. While TRT may have these effects, the FDA states that “Unlike drugs, supplements are not intended to treat, diagnose, prevent, or cure diseases. Claims like these can only legitimately be made for drugs, not dietary supplements.” [8]. However, despite this FDA statement, the “T booster” supplements made a host of claims. While some of these may be associated with improvements in T, others may not.
In addition, supplements also made promises for which there is limited to no available data for, including: to “feel or be stronger”, “increase energy”, “burn fat or prevent fat build up”, “reduce recovery time”, “improve sleep”, “improved vascularity”, “promote healthy aging”, and “improve bones and joints”. It is important that patients have a realistic picture of what to expect with T supplementation. Certainly, it is not a substitute for a healthy lifestyle, which is what many of the claims seem to tout.
Limitations of our study are that we used only Google as our search engine, and there may be regional and geographic differences in search engine results. We chose Google as our search engine because it is the most commonly used search engine [9], however, the addition of other search engines (Yahoo or Bing) may yield different results. In addition, only the first and most frequently appearing 50 supplements were included in the study, acknowledging that other products and supplements may be available that were not studied here. This study also only utilized a single search term (“Testosterone Booster”). While different search times produced results that were not relevant to this study, such as products with exogenous T and hormones, a different search phrase may have produced a varied supplement list. However, despite these limitations, our data clearly demonstrates the unrealistic expectations that are stated online for the role of vitamins and antioxidants in male infertility. This highlights the need for evidence-based patient education materials relating to this topic.
Despite the FDA statement against the use of supplements to treat conditions, 90% of “T booster” supplements claimed to boost T. However, only 24.8% of these had data to support these claims, based on their components. A total of 10.1% contained components with data to demonstrating a negative effect on T. Many had supra-therapeutic doses of vitamins and minerals, occasionally over the upper tolerable limit, with associated risks. Patients should be informed that “T booster” supplements may not have components with mechanisms to support their claims.
References
1. Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW, et al. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab. 2008; 93:2737–2745. PMID: 18270261.

2. Vermeulen A, Kaufman JM. Ageing of the hypothalamo-pituitary-testicular axis in men. Horm Res. 1995; 43:25–28. PMID: 7721258.
3. Hall SA, Araujo AB, Esche GR, Williams RE, Clark RV, Travison TG, et al. Treatment of symptomatic androgen deficiency: results from the Boston Area Community Health Survey. Arch Intern Med. 2008; 168:1070–1076. PMID: 18504335.
4. Bailey RL, Gahche JJ, Thomas PR, Dwyer JT. Why US children use dietary supplements. Pediatr Res. 2013; 74:737–741. PMID: 24002333.

5. Dickinson A, Blatman J, El-Dash N, Franco JC. Consumer usage and reasons for using dietary supplements: report of a series of surveys. J Am Coll Nutr. 2014; 33:176–182. PMID: 24724775.

6. Aaberg RA, Sauer MV, Sikka S, Rajfer J. Effects of extracellular ionized calcium, diltiazem and cAMP on motility of human spermatozoa. J Urol. 1989; 141:1221–1224. PMID: 2540352.

7. Tahvilzadeh M, Hajimahmoodi M, Toliyat T, Karimi M, Rahimi R. An evidence-based approach to medicinal plants for the treatment of sperm abnormalities in traditional Persian medicine. Andrologia. 2016; 48:860–879. PMID: 27681644.

8. US Food and Drug Administration (FDA). Dietary supplement products & ingredients [Internet]. Silver Spring (MD): FDA;2019. cited 2019 Jan 2. Available from: https://www.fda.gov/Food/DietarySupplements/ProductsIngredients/default.htm.
9. Net Market Share. Market share statistics for internet technologies [Internet]. Aliso Viejo (CA): Net Market Share;cited 2018 Jan 8. Available from: https://netmarketshare.com/search-engine-market-share.aspx?options=%7B%22filter%22%3A%7B%22%24and%22%3A%5B%7B%22deviceType%22%3A%7B%22%24in%22%3A%5B%22Desktop%2Flaptop%22%5D%7D%7D%5D%7D%2C%22dateLabel%22%3A%22Trend%22%2C%22attributes%22%3A%22share%22%2C%22group%22%3A%22searchEngine%22%2C%22sort%22%3A%7B%22share%22%3A-1%7D%2C%22id%22%3A%22searchEnginesDesktop%22%2C%22dateInterval%22%3A%22Monthly%22%2C%22dateStart%22%3A%222017-01%22%2C%22dateEnd%22%3A%222017-12%22%2C%22segments%22%3A%22-1000%22%7D.
10. National Institutes of Health, Office of Dietary Supplements. Nutrient recommendations: dietary reference intakes (DRI) [Internet]. Bethesda (MD): National Institutes of Health, Office of Dietary Supplements;cited 2018 Jan 19. Available from: https://ods.od.nih.gov/Health_Information/Dietary_Reference_Intakes.aspx.
11. Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and management of testosterone deficiency: AUA guideline. J Urol. 2018; 200:423–432. PMID: 29601923.

12. Sehn E, Mozak C, Yuksel N, Sadowski CA. An analysis of online content related to testosterone supplementation. Aging Male. 2019; 22:141–149. PMID: 29921150.

13. Nguyen SM, Ko Ko N, Sattar AS, Gucuk Ipek E, Ali S. Pulmonary embolism secondary to testosterone-enhancing herbal supplement use. Cureus. 2017; 9:e1545. PMID: 29018642.

14. US Food and Drug Administration (FDA). FDA drug safety communication: FDA cautions about using testosterone products for low testosterone due to aging; requires labeling change to inform of possible increased risk of heart attack and stroke with use [Internet]. Silver Spring (MD): FDA;2018. cited 2019 Feb 28. Available from: https://www.fda.gov/Drugs/DrugSafety/ucm436259.htm.
15. Engelhardt PF, Riedl CR. Effects of one-year treatment with isoflavone extract from red clover on prostate, liver function, sexual function, and quality of life in men with elevated PSA levels and negative prostate biopsy findings. Urology. 2008; 71:185–190. discussion 190. PMID: 18308079.

Table 1
Individual components for “T booster” supplements and the percentage of surveyed supplements containing those components
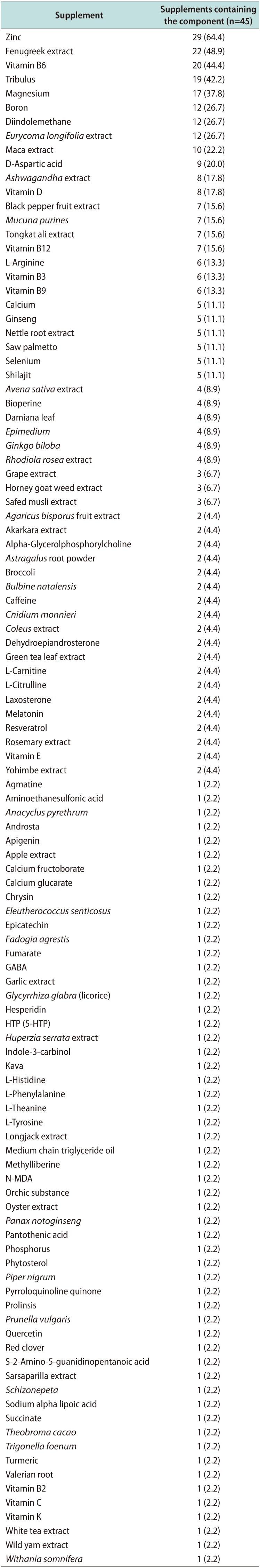
Table 2
“Beneficial” claims made by supplements
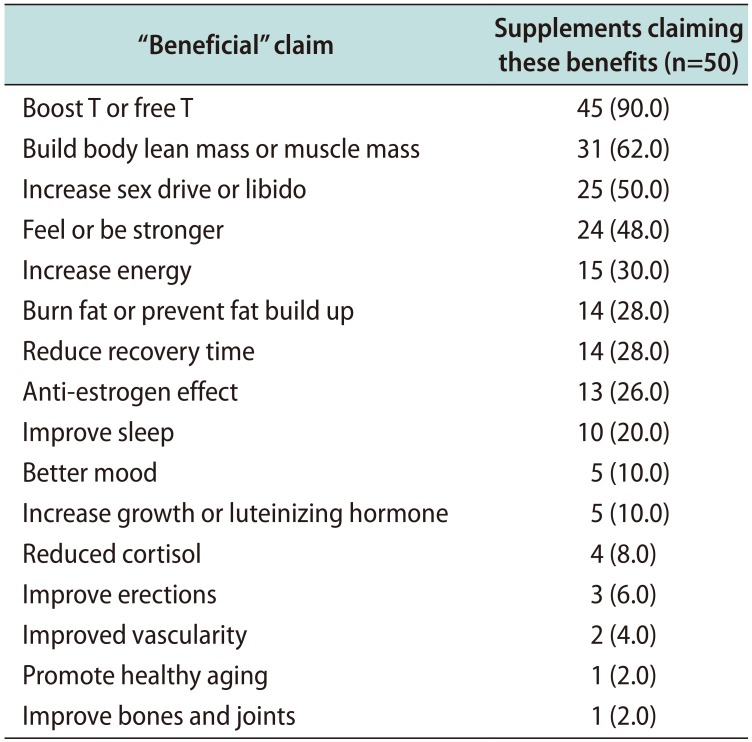
Table 3
Published evidence showing an increase, decrease or no change in testosterone (T) with supplementation
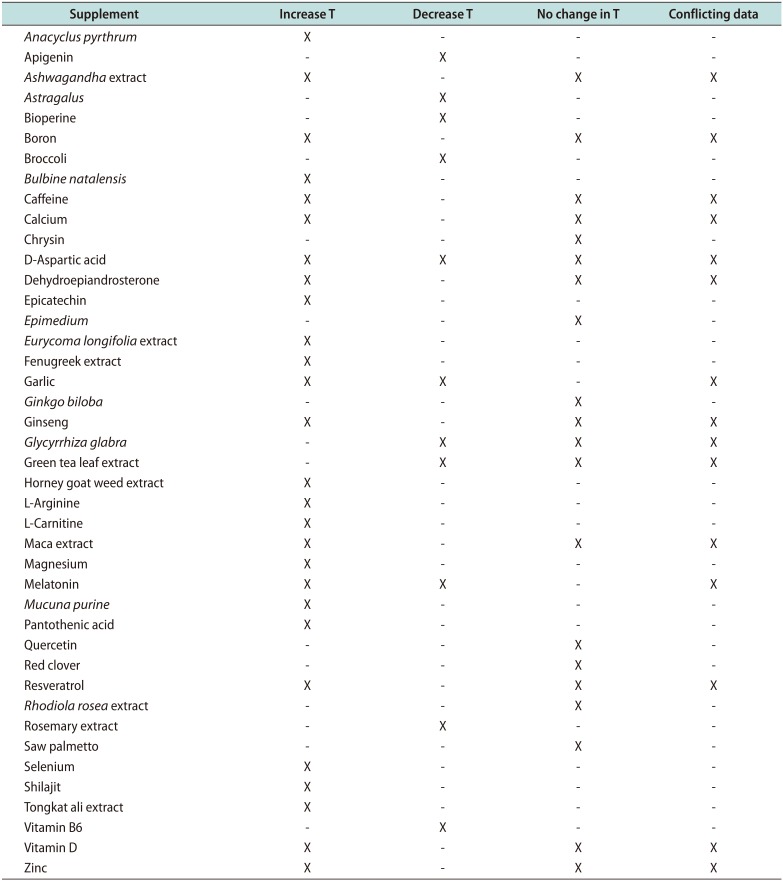
Table 4
Recommended Daily Allowance (RDA) and upper tolerable limit for each of the individual supplement components (when available)





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download