MATERIALS AND METHODS
The dermoscopic images evaluated in this study were collected in the database of the Department of Dermatoveneorology of the Bezmialem Vakif University. This study was approved by the Institutional Review Board of the Bezmialem Vakif University (IRB no. 54022451-050.05.04). The written consent from the patient to report and publish the identifiable patient images was obtained from the patients. In total, images of 504 melanocytic nevi were obtained from patients (47 females and 53 males). All patients had skin types II, III, or IV according to Fitzpatrick's classification
1. Dermoscopic evaluations at each visit were performed using a computerized polarized-light video dermoscopy system (FotoFinder dermoscope; Teach Screen Software, Bad Birnbach, Germany) with an alcohol interface solution. Dermoscopic images of follow-up visits, which were performed at baseline, 12 months, 24 months, and 48 months were evaluated. Dermoscopic changes in lesions were evaluated by the observation of 2 groups of changes in subsequent visits, changes in size and changes in color, to determine their dermoscopy scores. Patterns were defined according to the 2003 consensus conference
2. Congenital types of nevi were excluded from the study, and only nevi acquired after the first two years of life were included in this study. Dermoscopic images of up to five nevi were obtained.
Statistical analysis
Descriptive analysis of the sample was performed, including percentages for categorical variables and the mean, minimum, and maximum values and standard deviations for continuous variables. All statistical analyses were performed using the SPSS Statistical software program ver. 15.0 (SPSS Inc., Chicago, IL, USA). The results were considered to be statistically significant when the p-value was less than 0.05.
Go to :

RESULTS
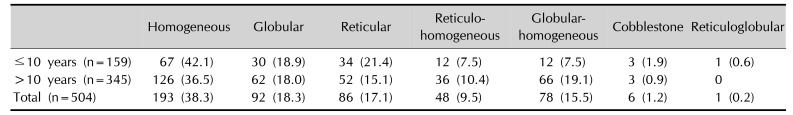
Five hundred and four nevi from one hundred patients were enrolled in the study: 53 male (53%) and 47 female (47%). The mean age of the patients was 12.01±3.38 (minimum: 3, maximum: 16). Only nevi located on the trunk were included in the study. Nine patients had Fitzpatrick skin type II, 52 had Fitzpatrick skin type III, and 39 had Fitzpatrick skin type IV. The most common dermoscopic patterns were homogeneous (193 nevi; 38.3%), globular (92 nevi; 18.3%), reticular (86 nevi; 17.1%), globular-homogeneous (78 nevi; 15.5%), reticulo-homogeneous (48 nevi; 9.5%), reticuloglobular (1 nevus; 0.2%), and cobblestone (6 nevi; 1.2%) (
Table 1). There were 11 halo nevi at baseline; at the end of the 4 years, all of these nevi had faded.
Table 1
Dermoscopic patterns of groups younger and older than 10 years old per nevus count
|
Homogeneous |
Globular |
Reticular |
Reticulohomogeneous |
Globularhomogeneous |
Cobblestone |
Reticuloglobular |
|
≤10 years (n=159) |
67 (42.1) |
30 (18.9) |
34 (21.4) |
12 (7.5) |
12 (7.5) |
3 (1.9) |
1 (0.6) |
|
>10 years (n=345) |
126 (36.5) |
62 (18.0) |
52 (15.1) |
36 (10.4) |
66 (19.1) |
3 (0.9) |
0 |
|
Total (n=504) |
193 (38.3) |
92 (18.3) |
86 (17.1) |
48 (9.5) |
78 (15.5) |
6 (1.2) |
1 (0.2) |

The mean diameter of the nevi with complex patterns was 9.06±1.42 mm, that of nevi with only one pattern (reticular, globular, and cobblestone) was 7.22±0.74 mm, and that of nevi with homogenous patterns was 6.83±0.92 mm. There were statistically significant differences between the the groups related to the diameter of the nevi (p=0.041).
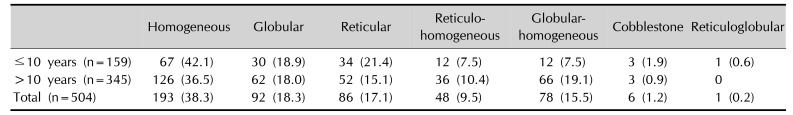
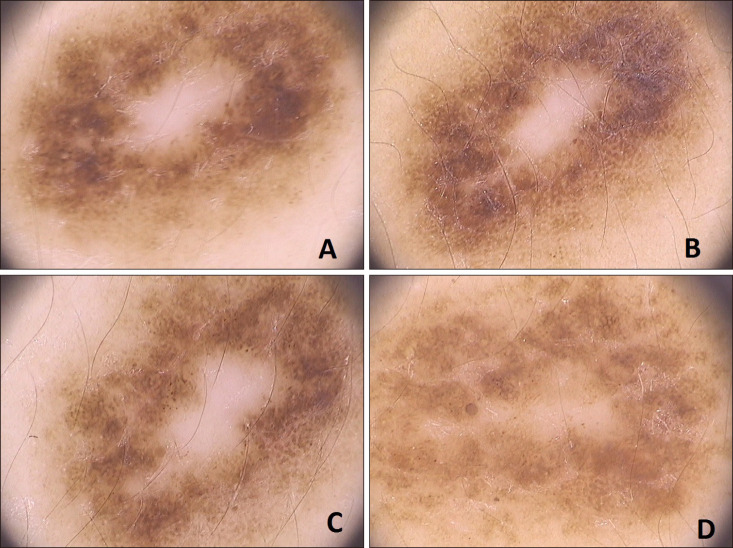
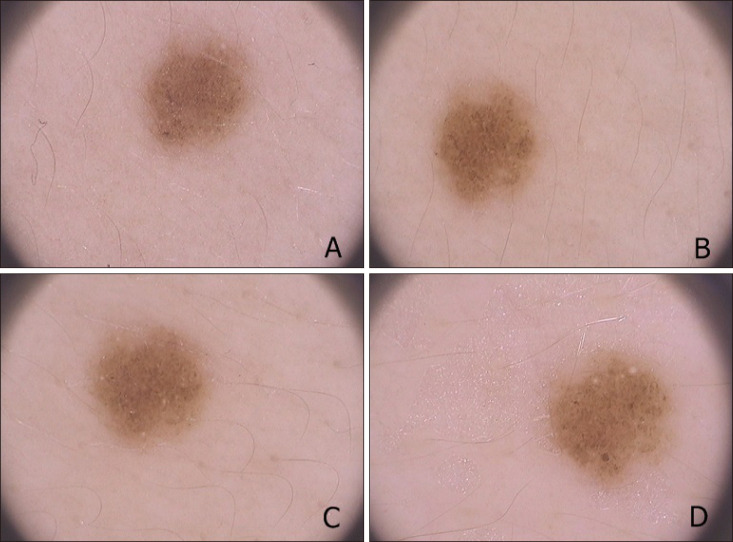
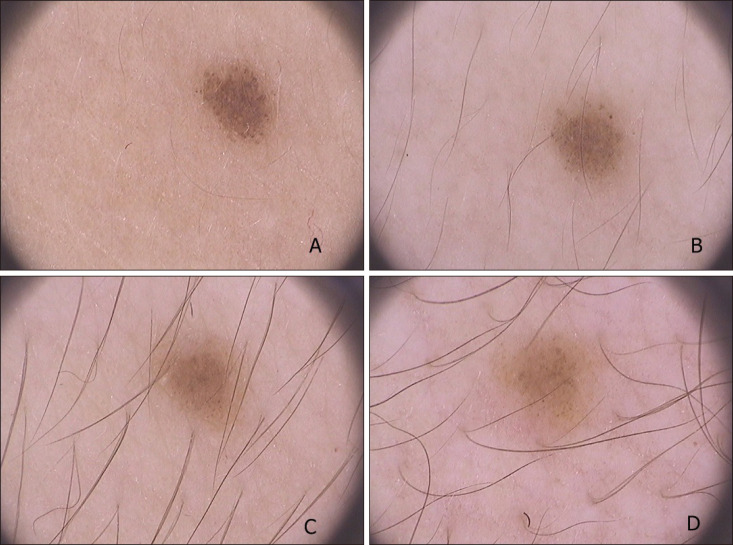
The transformation from a homogeneous to a globular-homogeneous pattern was the most frequent pattern change (19 of 114; 16.7%) (
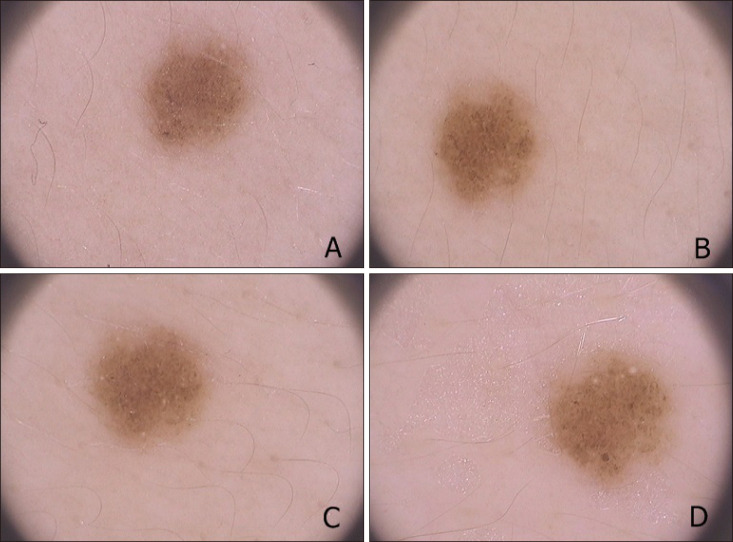
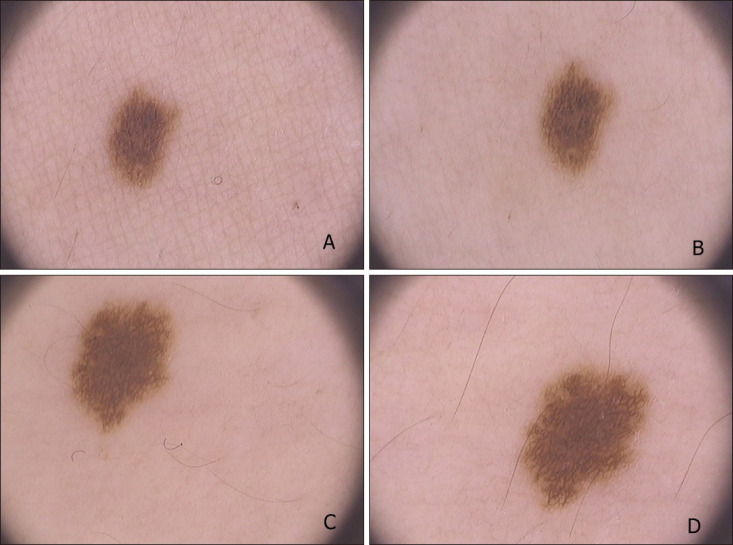
Fig. 1). The transformation from a homogeneous pattern to a reticular-homogeneous pattern was the second most common pattern change (14 of 114; 12.2%), and globular to globular-homogeneous was the third most common pattern change (12 of 114; 10.5%) (
Fig. 2).
 | Fig. 1A 9-year-old boy, nevus on the arm, dermoscopic change of homogeneous pattern to homogeneous-globular pattern (A: baseline, B: 12 months after, C: 24 months after, D: 48 months after).
|
 | Fig. 2A 14-year-old boy, nevus on the leg, dermoscopic change of globular pattern to homogeneous pattern (A: baseline, B: 12 months after, C: 24 months after, D: 48 months after).
|
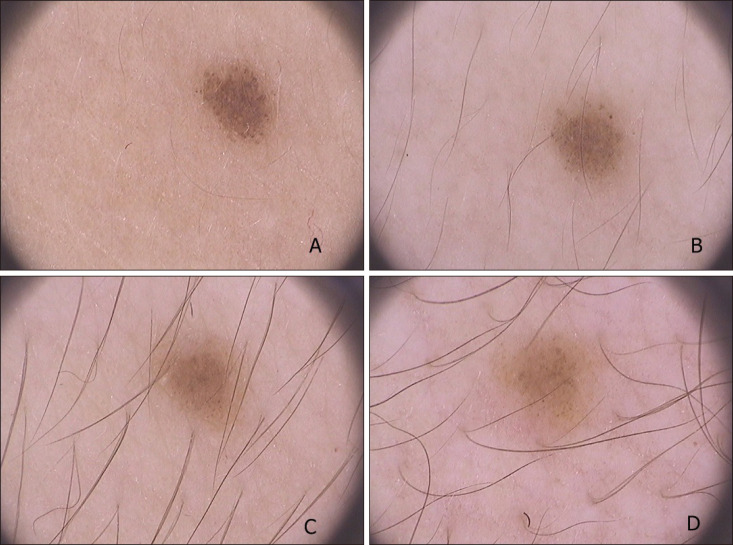
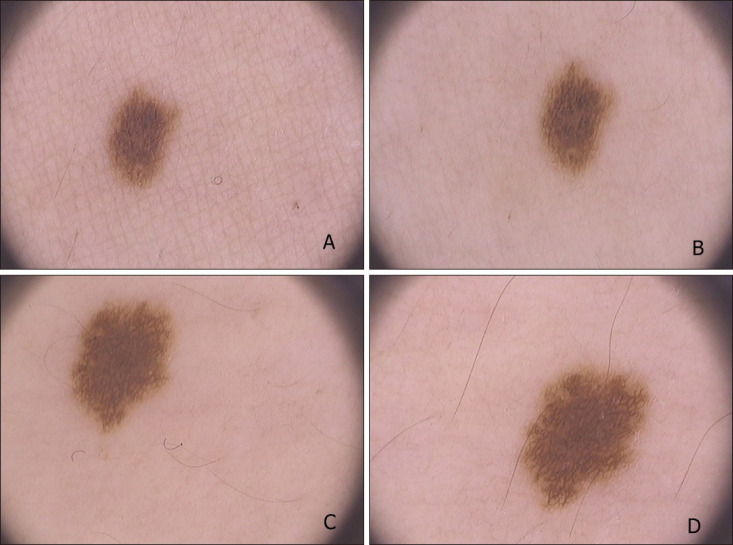
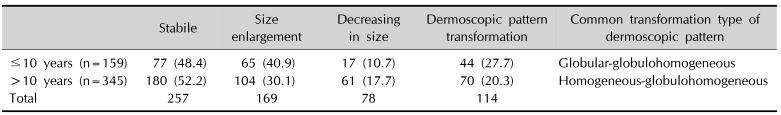
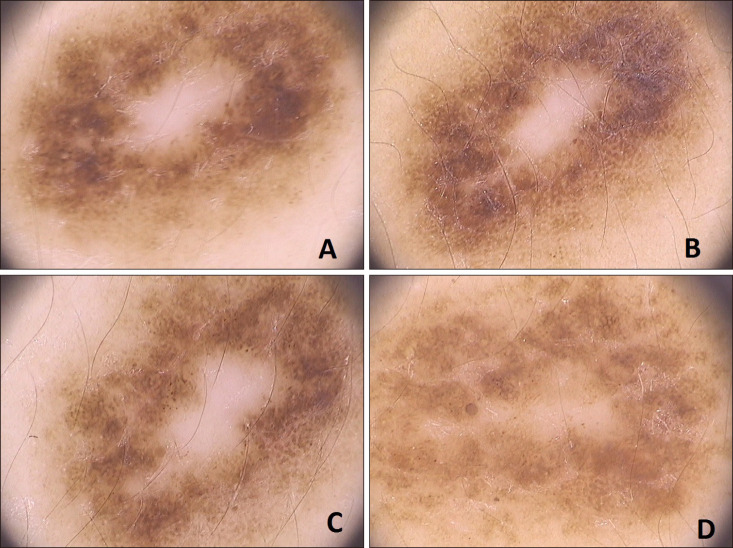
Although 257 of the 504 nevi (51.0%) have shown a stable duration without size changes, 169 of the 504 nevi (33.5%) had enlarged (
Fig. 3,
4), and 78 of the 504 nevi (15.5%) had become smaller during our 4-year experience of dermoscopic monitoring. Of the 169 nevi, 81 had homogeneous pattern (47.9%), 37 had globular pattern (21.9%), 21 had reticular pattern (12.4%), 14 had globular-homogeneous (8.3%), 13 had reticular-homogeneous pattern (7.7%), 3 had cobblestone pattern (1.8%). There was statistical difference between the groups related to enlargement (
p=0.041). All of the halo nevi had disappeared at this time. One hundred and fourteen nevi had pattern transformation (22.6%).
 | Fig. 3A 10-year-old girl, nevus on the back, dermoscopic change of homogeneous pattern to reticular pattern, enlargement of nevus (A: baseline, B: 12 months after, C: 24 months after, D: 48 months after).
|
 | Fig. 4A 12-year-old girl, nevus on the back, dermoscopic change of homogeneous-globular pattern to homogeneous-reticular pattern (A: baseline, B: 12 months after, C: 24 months after, D: 48 months after).
|
Thirty-three of 61 patients (54.1%) who had pattern changes were male, and 28 of 61 patients (45.9%) were female. No significant difference between genders related to pattern changes was observed (
p=0.839). There were 30 children younger than 10 years old (159 nevi) and 70 children older than 10 years old (345 nevi). There was no statistical association between age and pattern changes (
p=0.372) (
Table 2).
Table 2
Differences of groups younger and older than 10 years old per nevus count
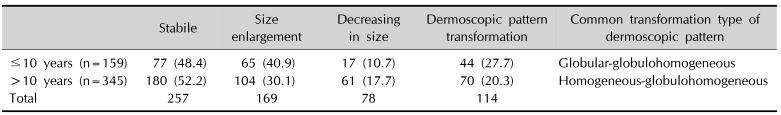
|
Stabile |
Size enlargement |
Decreasing in size |
Dermoscopic pattern transformation |
Common transformation type of dermoscopic pattern |
|
≤10 years (n=159) |
77 (48.4) |
65 (40.9) |
17 (10.7) |
44 (27.7) |
Globular-globulohomogeneous |
|
>10 years (n=345) |
180 (52.2) |
104 (30.1) |
61 (17.7) |
70 (20.3) |
Homogeneous-globulohomogeneous |
|
Total |
257 |
169 |
78 |
114 |
|

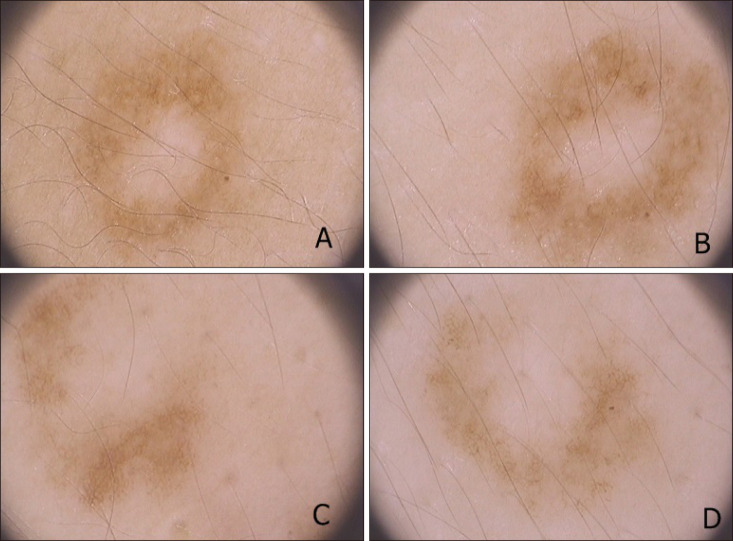
Color changes were observed in 70 of 504 nevi (13.9%). Fifty-one nevi were fading in color (
Fig. 5). Nineteen of the nevi darkened in color. There was no significant difference between genders and age-related groups (
p=0.243,
p=0.751). Peripheral dots and clods were found in 49 of 100 patients at baseline (198 nevi). At the end of 4 years, 128 of 198 nevi (64.6%), lost these structures.
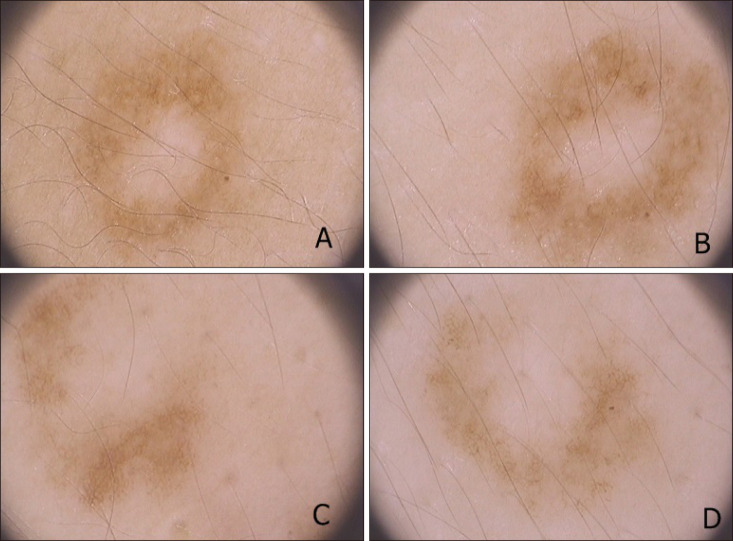 | Fig. 5A 8-year-old boy, nevus on the back, dermoscopy of homogeneous-reticular pattern, fading in color (A: baseline, B: 12 months after, C: 24 months after, D: 48 months after).
|
Go to :

DISCUSSION
Commonly acquired nevi are defined as small, flat, brown lesions that can appear anywhere on the surface of the body after birth. Childhood is a dynamic period with regard to the development of nevi. Many new nevi will appear, enlarge, and finally begin to disappear. To make an accurate diagnosis of melanoma in childhood and adolescence without performing unnecessary biopsies and excisions, dermoscopic patterns, size changes, and color changes must be well understood.
Peripheral dots and clods are usually found in common nevi of children, and during follow-up examinations, these structures disappear while the sizes of the lesions enlarge. This finding is consistent with observations described in the literature
34.
All halo nevi have a central globular pattern at first, and during follow-up, they begin to fade.
Finally, all of the nevi disappeared with only a gray-brown homogeneous pigmentation. It has been proposed that the central part of the nevus has a progressive involution by T lymphocytes
5. Due to the disappearance of all halo nevi by four years, we suggest that symmetrical halo nevi should not be excised, and the preferential management for these nevi with this pattern is simply monitoring.
It has been thought that the globular pattern is the most common dermoscopic pattern in childhood, and nevi in children evolve from globular to reticular through the years
6. Zalaudek et al.
6 found that the globular pattern is the most prevalent pattern (60%), followed by complex (21%), reticular (12%), and homogeneous (5%) patterns.
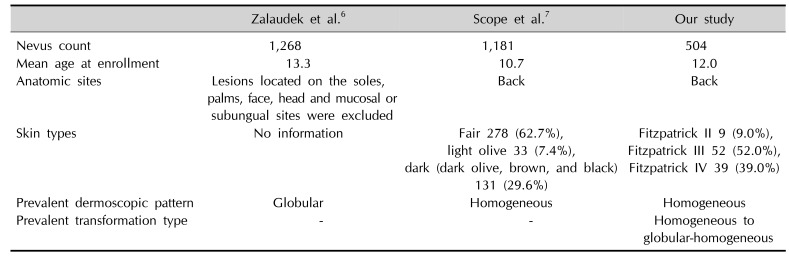
There are significant differences in the distribution of nevi by dermoscopic classification between studies present in the literature: Zalaudek et al.
6 classified 8 of 151 nevi (5%) as homogeneous, Scope et al.
7 classified 468 of 936 nevi (50%) as homogenous, and we classified 193 of 504 nevi (38%) as homogenous. The mean age of the children was 13.3 years in the study of Zalaudek et al.
6, 10.7 years in the study of Scope et al.
7, and 12.01 years in our study.
Zalaudek et al.
6 studied patients presenting nevi >5 mm. For comparison, if we analyze larger nevi in our study, the frequency of homogeneous patterns decreases, similar to the findings of Scope et al.
7. We also enrolled the smallest nevi as well as the largest nevi. In addition, Zalaudek et al.
6 studied older children, with a mean age of 13.3 years (10.7 in Scope et al.
7 vs. 12 in our study). The SONIC study demonstrated that the frequency of the homogeneous pattern decreased from 38% at baseline (mean age 12 years) to 28% after 1 year (mean age 13 years) (
Table 3)
8. Most of our patients had Fitzpatrick skin type III and IV. The phenotypic features of our population were similar to those examined by Scope et al.
7. The proportion of reticular pattern was lower among children under the age of 10 years, and our results support this observation.
Table 3
Comparison of studies about dermoscopy of pediatric nevi
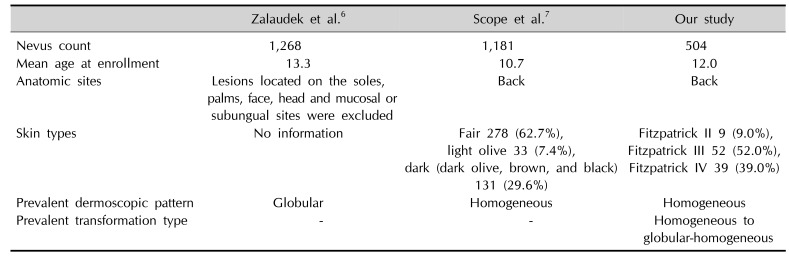
|
Zalaudek et al.6
|
Scope et al.7
|
Our study |
|
Nevus count |
1,268 |
1,181 |
504 |
|
Mean age at enrollment |
13.3 |
10.7 |
12 |
|
Anatomic sites |
Lesions located on the soles, palms, face, head and mucosal or subungual sites were excluded |
Back |
Back |
|
Skin types |
No information |
Fair 278 (62.7%), light olive 33 (7.4%), dark (dark olive, brown, and black) |
Fitzpatrick II 9 (9.0%), Fitzpatrick III 52 (52.0%), Fitzpatrick IV 39 (39.0%) |
|
131 (29.6%) |
|
|
Prevalent dermoscopic pattern |
Globular |
Homogeneous |
Homogeneous |
|
Prevalent transformation type |
- |
- |
Homogeneous to globular-homogeneous |

In this study, we aimed to identify dermoscopic transformations in our country. We found the homogeneous pattern to be the prevalent dermoscopic pattern (38%), and the transformation from a homogeneous pattern to a globular-homogeneous pattern (16%) was the prevalent transformation type. Although the reticular nevus pattern on dermoscopy correlates with junctional nevi histopathologically, the globular nevus pattern correlates with compound or dermal nevi
910.
However, it is more difficult to histopathologically predict the location of homogeneous pattern nevus. Worret and Burgdorf
11 reported that in their series, none of the children under the age of 10 years showed completely junctional nevi, and their nevi were often characterized by compound and dermal nevi.
From a histological perspective, nevi with a globular pattern are dermal proliferations of melanocytes, while nevi with a reticular pattern are epidermal proliferations of melanocytes
12.
Although dermoscopy correlates with the histopathological pattern of melanocytic neoplasms, there are limitations to the dermoscopic-pathological correlation. Using dermoscopic-reflectance confocal microscopy (RCM)-histopathological correlation, Pellacani et al.
13 showed that nevi with a globular dermoscopic pattern correlated either with a predominantly junctional or a predominantly dermal nested proliferation of melanocytes. Furthermore, nevi with a reticular dermoscopic pattern correlated with either predominantly lentiginous or predominantly nested junctional proliferations of melanocytes. Using RCM for longitudinal tracking of changes in nevi, the authors showed that while some nevi changed dermoscopically from the globular pattern to reticular pattern, they did not demonstrate a change in their overall RCM pattern. These nevi showed a meshwork pattern on RCM throughout their evolution, consistent with a nested junctional proliferation of melanocytes
13.
Thus, we posited that, while such growing nevi can show a dermoscopic change from ahomogeneous to globular pattern, melanocytic proliferation occurs within the same anatomical compartment.
Fifty two percent of nevi did not demonstrate a change in size. While 33% of the nevi had symmetrical enlargement, 15% of nevi had involution. Cordoro et al.
14 investigated whether conventional asymmetry, border, color, diameter, evolution (ABCDE) melanoma detection criteria adequately define pediatric melanoma and analyzed clinicopathological and outcome differences between younger and older children. They suggested that conventional ABCDE criteria and additional amelanotic; bleeding, bump; color uniformity; de novo, any diameter detection criteria may be helpful for earlier recognition and treatment of melanoma in children when these criteria were used together
14. Therefore, size changes, either enlargement or involution are common in pediatric population, and we recommend that parents not be concerned all enlargements of nevi. Even though, 15% of nevi had involution, 33% of nevi had enlargement in our study. As well as enlargement may be related with the growth of children, homogeneous pattern is more common in pediatric population in our study, and the most frequent pattern in the enlargement group was homogeneous pattern, therefore these nevi are more prone to enlarge in terms of diameter. These results showed that dermoscopic changes associated with suspicion for development of melanoma are common in children. Therefore, excision is not a good option when the clinician observes these findings in a pediatric population.
Our limitation was the lack of dermoscopic and pathological correlation. Since we did not excise the lesions, our study was based on a dermoscopic follow-up. Therefore, we observed the predominance of the homogeneous pattern, but we could not determine the actual histology of these nevi. Thus, further studies investigating dermoscopic patterns of children from different races are needed to better understand the anatomic correlates and clinical significance of each pattern.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download